Transanal endoscopic microsurgery (TEM) has been shown to be very useful in the removal of intraluminal lesions of the rectum, both benign and malignant.1 Nevertheless, there is little experience in its use in diseases outside of Coloproctology or in other locations. We present a case that shows endoscopic ultrasound localization and resection by means of TEM of a pararectal recurrence of prostate cancer.
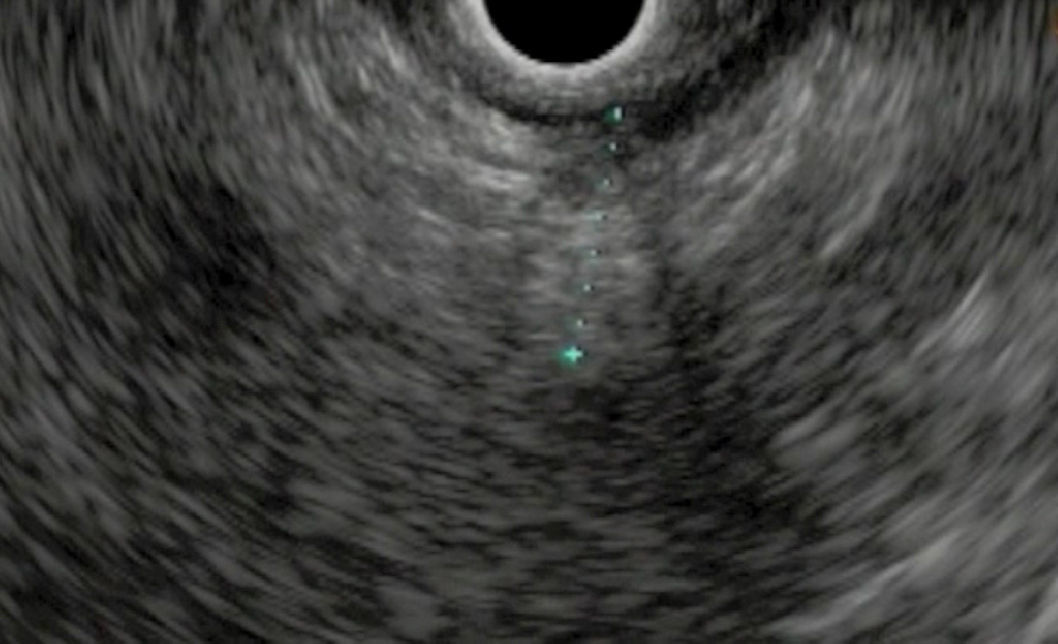
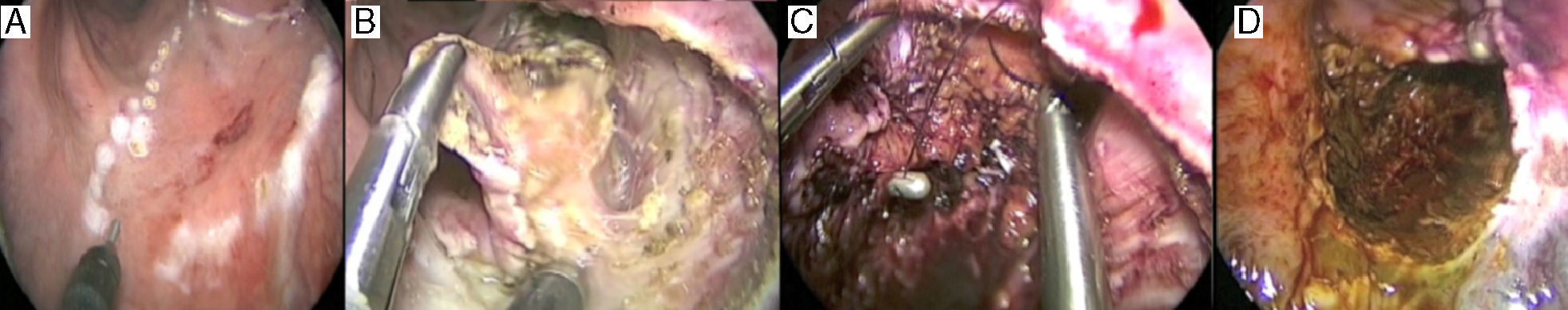
The patient is a 66-year-old male with a previous diagnosis of prostate adenocarcinoma (T1c N0 M0, Gleason 6) that was treated with brachytherapy and radioactive seed implantation125 in May 2006. The patient had periodic follow-ups with control of symptoms and biochemistry showing no evidence of recurrence of the disease for 44 months, until in February 2010 a progressive elevation in PSA levels was observed (up to 8.6ng/ml). Pelvic MRI revealed a right pararectal node measuring 2cm in diameter that was also observed in a choline-PET study as a single nodular area of uptake in the pararectal region suggestive of local recurrence.2 By means of rectal endoscopic ultrasound, the presence of a node was confirmed in the perirectal fat of the right anterolateral quadrant with infiltration of the rectal musculature. Needle biopsy was performed and the node was marked with the implantation of a gold seed marker. Cytology confirmed the diagnosis of adenocarcinoma. Treatment was initiated with complete androgen blockade using Zoladex and Casodex, after which we observed a good biochemical response translated into a reduction in PSA levels of 0.5ng/ml after 3 months. In spite of this, the persistence of the node was observed on MRI, although there were changes as a result of the treatment. Six months later, a choline-PET study revealed normalization of the focus described in the pararectal region related to the metabolic response to the treatments received. Given this situation of good biochemical response and persistence of the lesion on MRI, we decided to perform surgical exeresis. In December 2010, with prior intraoperative localization of the lesion by rectal endoscopic ultrasound (Fig. 1) and marking with biopsy forceps, resection was performed with the TEM technique (Fig. 2A and B). The resected specimen measured 4.5cm×4.2cm with a tumor in its interior measuring 1.2cm×1.2cm. The closure of the defect was done with a continuous monocryl 3/0 suture, fastened with silver stops at the ends. After povidone–iodine lavage, an orifice measuring 0.5cm was left in the medial distal portion for drainage (Fig. 2C and D). Surgical time was 158min and there were no additional technical difficulties. The day before the intervention, complete large-bowel prep had been carried out.
(A) Outline of the safety margin around the lesion, previously marked with the biopsy forceps; (B) resection of the tumor recurrence by means of TEM; observe the opening of the complete thickness of the rectal wall up until the prostatic plane; (C) partial closure of the defect with continuous monofilament 3/0 suture, fastened at the ends with silver stops; and (D) final appearance of the rectum after the partial closure of the defect and povidone–iodine lavage.
The pathological diagnosis was infiltration of the perirectal fat and muscle layer of the large intestine by an adenocarcinoma compatible with prostatic origin, with post-treatment modifications. The resection margins were tumor-free.
There were no complications during the postoperative period and the patient was discharged from hospital on the third day after surgery. After discharge, the patient did experience an episode of fever associated with anal pain secondary to dehiscence of the suture line, with no presence of collections. The patient presented good clinical response to treatment with antibiotics and anti-inflammatory drugs.
When faced with the need to resect a perirectal lesion, a minimally invasive approach such as TEM becomes a good therapeutic option. In this case, if TEM were not used, anterior resection of the rectum would have been necessary. This would have been much more aggressive, with important functional repercussions and a longer and more painful post-operative period.3–6 In situations like the one we present, TEM becomes a less painful technique that safeguards the principles of oncological safety by presenting disease-free resection margins. To ensure the margins, it was essential to use complementary intraoperative rectal endoscopic ultrasound for the localization and exact marking of the lesion. Endoscopic ultrasound could have been performed before surgery in order to reduce operative time, but in this case we opted to do it during the surgery itself to avoid additional sedation. Since its first description, the TEM technique has progressively been used for more indications, from benign lesions or early rectal cancer7 to the resection of benign rectal stenoses,8 retrorectal tumors,9 rectal prolapse, rectal trauma or impacted fecal matter.10 We can conclude that the association of rectal endoscopic ultrasound and the TEM technique provides for complete exeresis of extraluminal lesions that are difficult to access by other approaches.
Please cite this article as: Arredondo J, Baixauli J, Subtil JC, Cambeiro M, Hernández-Lizoáin JL. Empleo de la microcirugía transanal endoscópica en recidiva de cáncer de próstata a nivel pararrectal. Cir Esp. 2013;91:458–459.