Aortic spasm is an unknown clinical entity about which there is little mention in the international literature. In contrast, however, arterial vasospasms are a relatively frequent condition caused by numerous factors,1,2 such as autoimmune diseases, drugs and recessive autosomal diseases, but there are no data about it affecting the aorta. It is a very rare clinical condition and difficult to diagnose, which could explain the lack of reports in the literature, together with the fact that intensive medical treatment can lead to its disappearance, with no imaging studies to confirm the patient's clinical profile.
The patient is a 56-year-old male with no prior medical history of interest who came to the emergency department with sudden-onset abdominal pain together with general decline in his physical status. Blood work showed: leukocytes 19 000mm3 (range: 4000–10 000), neutrophils 87% (range: 40–60), lactate dehydrogenase (LDH) 534IU/L (range: 105–333), C-reactive protein 20mg/L (normal level: up to 6), pH 7.30 (range: 7.35–7.45); activated partial thromboplastin time (APTT) 75s (range: 20–40).
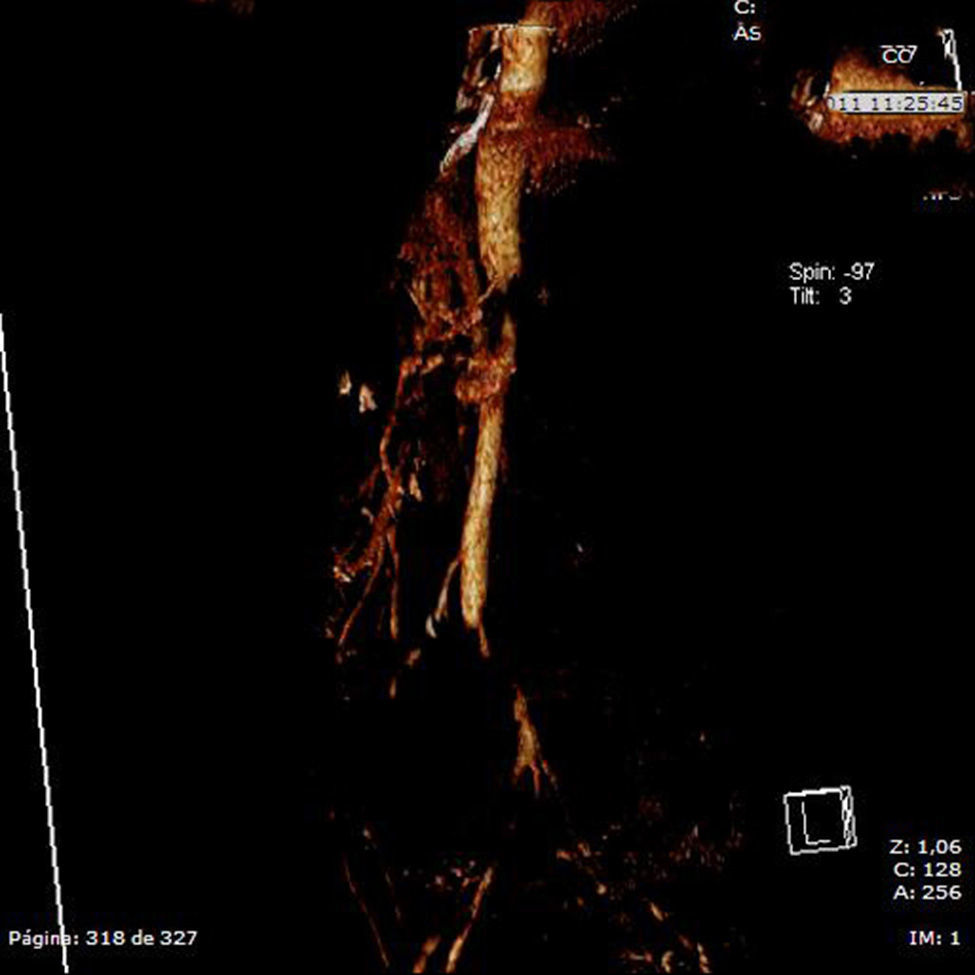
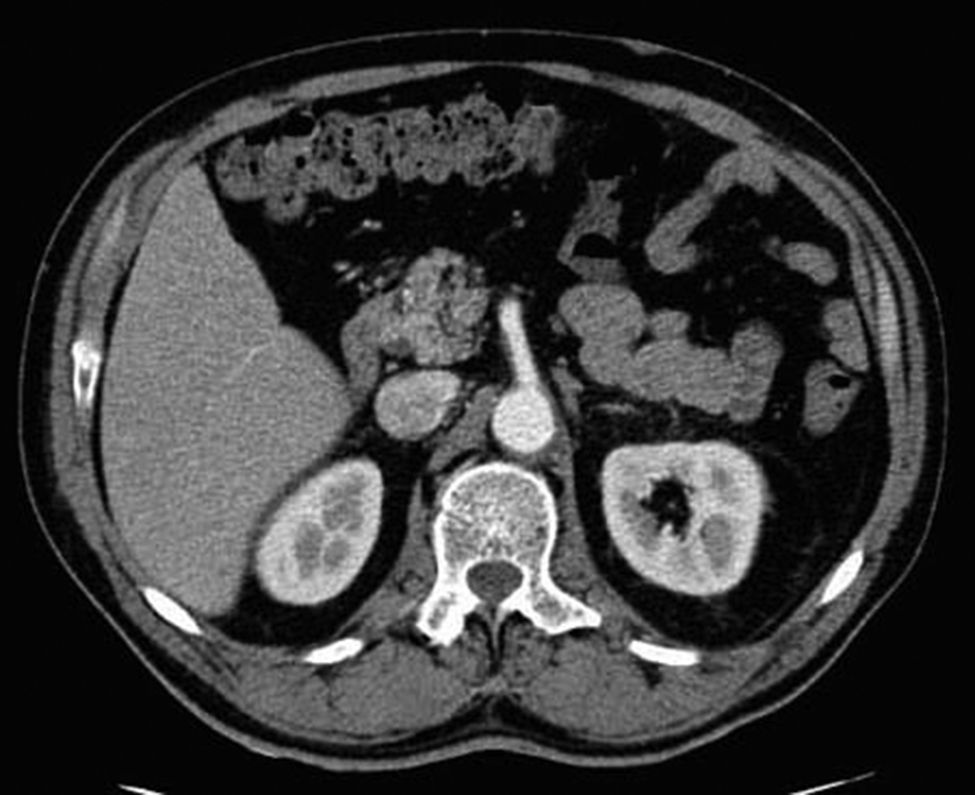
Given the suspicion of an acute abdominal process, probably intestinal ischemia, computed tomography (CT) scans with intravenous contrast were ordered of the abdomen and pelvis. Far from identifying signs suggestive of such a process within the arteries that are most frequently affected, complete aortic spasm was observed (Figs. 1 and 2) in a fleur-de-lis pattern that completely occluded the lumen and impeded the passage of contrast material to the superior and inferior mesenteric arteries. No intestinal pneumatosis was found, although there was important dilatation of the small bowel loops. The presumed diagnosis established was mesenteric ischemia due to aortic spasm.
Radiologically, no signs of ischemia were found, although livedo reticularis was observed in the lower limbs, while the lab work-up showed elevated serum creatinine (2.5g/dL), although this could have been due to the toxicity caused by intestinal ischemia.
Given the origin of the entity, we decided to maintain conservative medical treatment with intense serum therapy and vasodilators (nifedipine and captopril). The patient was once again interviewed in order to identify predisposing factors, such as the consumption of associated drugs (ergotamine) or autoimmune diseases, which the patient denied.
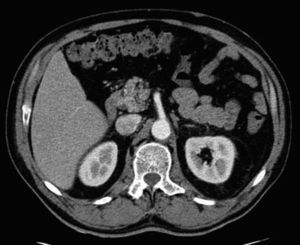
After 3h of intense medical treatment, the symptoms slowly began to recede. The analytical parameters 6h after the arrival of the patient showed: leucocytes 13 000, neutrophils 855, LDH 460, pH 7.35 and APTT 90%. Other parameters were unaltered. Another abdominal-pelvic CT scan with contrast was ordered, which confirmed the disappearance of the images from the previous scan (Fig. 3). The patient remained in observation for 48h, during which time the symptoms did not recur, and the patient was discharged. The patient was referred to the Internal Medicine Unit for complete studies and follow-up, although the aetiology was not determined.
Intestinal ischemia is relatively frequent in older patients with predisposing factors. Likewise, there are no reports of intestinal symptoms caused by aortic spasm. Thanks to conservative management, the episode was resolved without the need for surgery, which would have entailed an important risk for morbidity and mortality given the involvement of organs and arteries.
When treating symptoms of intestinal ischemia, one must consider the possibility of autoimmune and/or systemic diseases, or rather the use of drugs with associated activity, such as ergotamine or noradrenaline, as triggering factors of the disease. A detailed patient medical history is therefore necessary to be able to rule out any of these processes.
To the best of our knowledge, there have been no reports in the international literature to date about spontaneous aortic spasms with no predisposing factors. This could therefore be considered the first case described in the literature.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Pérez-Alonso AJ, Rubio-López J, Pérez-Durán C, Petrone P. Isquemia intestinal transitoria por espasmo aórtico. Cir Esp. 2016;94:192–194.