Coloplasty is a surgical technique reserved for oesophageal reconstructions when stomach interposition is not feasible. This procedure is associated with significant perioperative morbidity and mortality and, above all, the development of long-term stenosis. In addition, neoplasms may also arise in the interposed colon, although this possibility is rare. There are few cases described in the literature, and it is therefore common for its diagnosis to be unsuspected and delayed due to its limited incidence and lack of awareness.
We report the case of a 72-year-old male patient who, 23 years earlier, had been hospitalised for massive upper gastrointestinal (UGI) bleeding secondary to a benign ulcer of the gastric body. The patient required emergency surgery and underwent total gastrectomy and Roux-en-Y reconstruction. On the sixth day post-op, due to symptoms of peritonitis and respiratory failure, the patient was reoperated on, at which time a total dehiscence was observed of the oesophagojejunal anastomosis. Surgical treatment involved transhiatal oesophagectomy, terminal cervical oesophagostomy, closure of the jejunal loop and a jejunostomy feeding tube. Seven months later, digestive reconstruction was performed with isoperistaltic transverse coloplasty dependent on the left intestinal vessels and through the anterior mediastinum. Gastrointestinal continuity was achieved with the former Roux-en-Y loop. The patient was discharged and did not attend the scheduled outpatient follow-up visits.
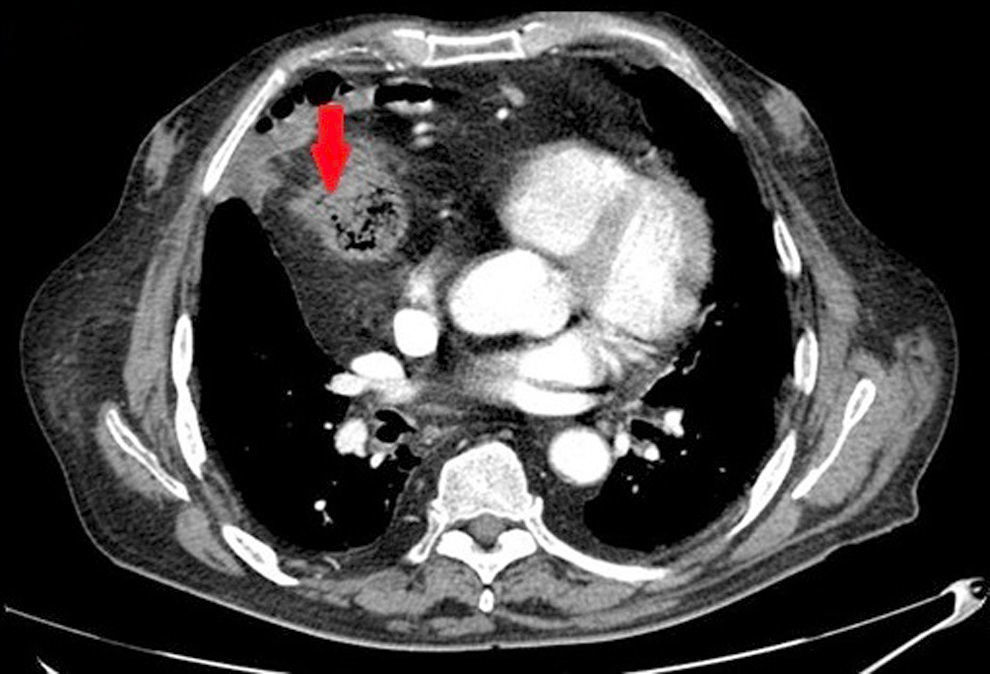
Presently, because of progressive dysphagia, an endoscopy study was ordered, which found a neoplasm 30cm from the dental arch. Biopsy identified the mass as a moderately differentiated intestinal adenocarcinoma. The extension study result was cT3N0 (Fig. 1). We performed a surgical approach with iterative cervicotomy, median sternotomy and midline laparotomy, followed by exeresis of the coloplasty. The digestive tract reconstruction was done with a “supercharged” jejunal segment that was provided with additional blood flow by means of anastomosis of the jejunal vein and artery to the left internal mammary vessels. The digestive anastomoses included an end-to-side oesophagojejunostomy and a side-to-side jejunojejunostomy on the Roux-en-Y loop of the former coloplasty.
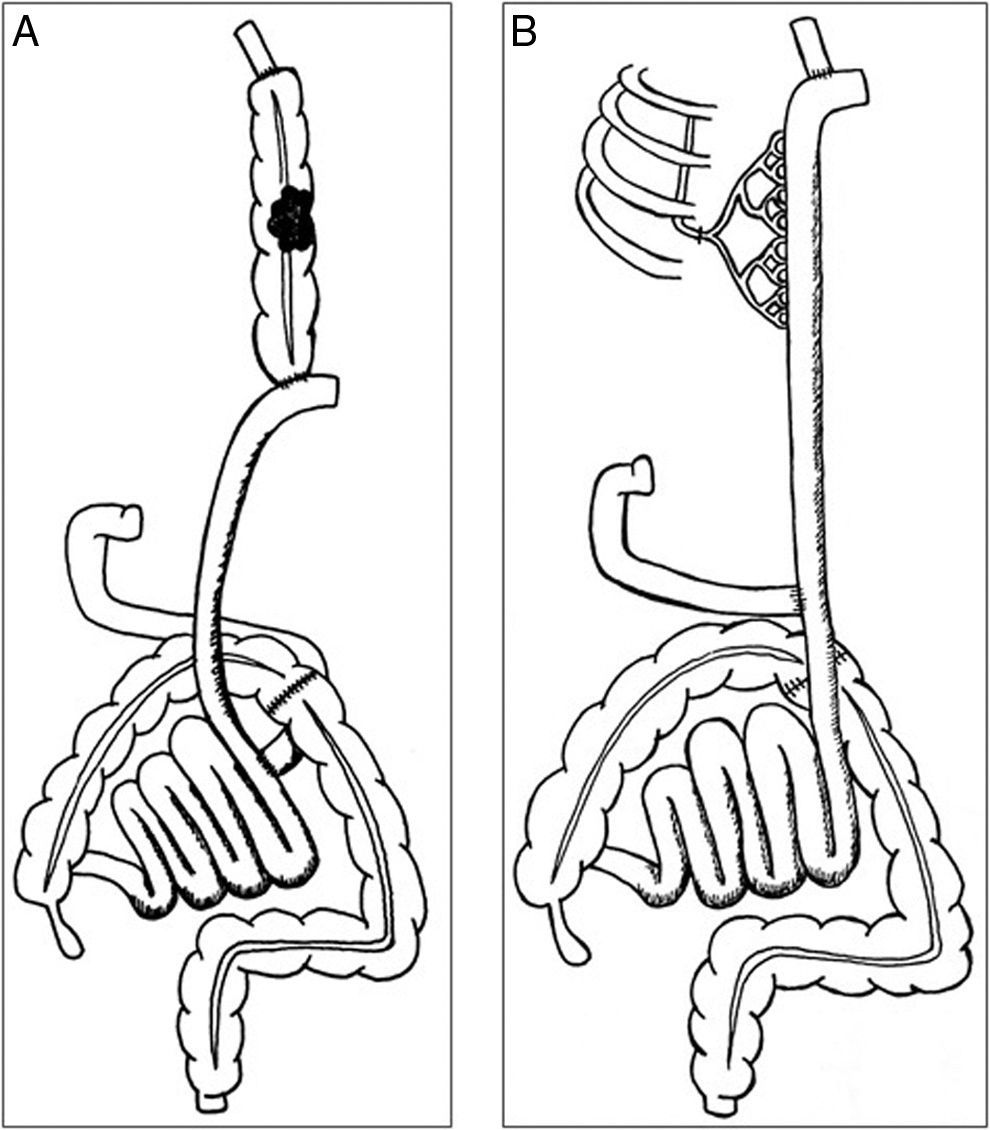
A sequential diagram of the reconstruction is presented in Fig. 2.
Diagram showing: (A) the previous situation of the patient with the adenocarcinoma that arose in the interposed bowel; and (B) the reconstruction, after exeresis of the colon, using interposition of a long segment of the jejunum with anastomosis of the jejunal vein and artery to the internal mammary vein and artery (supercharged).
The postoperative recovery was favorable, although a low-discharge cervical fistula was diagnosed on the 11th day postop, which was resolved with conservative treatment. The definitive pathology result was infiltrating low-grade adenocarcinoma pT4aN2b, so adjuvant chemotherapy was indicated. Currently, the patient is being followed-up in the outpatient clinic and continues with exclusively oral nutrition.
Coloplasty is a surgical alternative after oesophagogastrectomy, although it is associated with considerable morbidity and mortality. Reported complications include: ischemia of the coloplasty, dehiscence of the anastomosis, dysmotility and stenosis.1,2
In the literature, there are few cases that describe the development of adenocarcinoma in a coloplasty. It has been suggested that the physiopathology of its appearance is the same as for a colon neoplasm, although some authors propose that the action of the bile reflux on the mucosa of the bowel can favor dysplastic changes. Our group always conducts upper gastrointestinal reconstructions with a Roux-en-Y loop to avoid bile reflux that can be incapacitating. The time until the development of a neoplasm in a coloplasty is very variable and can appear from 3 to 55 years after surgery.3–6
As for treatment, surgery should respect oncologic criteria with wide resection margins and lymphadenectomy for correct staging. Adjuvant chemotherapy, in this case for colon cancer, should be administered according to the stage and following the TNM classification, while radiotherapy is not recommendable due to the possibility of radiation enteritis.1,7,8
Although to date screening is not necessary for all patients with a coloplasty, we believe it is important to consider this rare diagnosis at the onset of dysphagia.
AuthorshipAll the authors have contributed to the creation of this article and have read and approved of the manuscript. The requirements for authorship have been met.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Gálvez-Saldaña A, Miró M, López A, Toral D, Farran L. Neoplasia de colon, una excepcional posibilidad en una coloplastia. Cir Esp. 2016;94:191–192.