Inflammatory myofibroblastic tumours are a very rare type of benign mesenchymal tumour. Most reported cases affect children and young adults, and these tumours are most often found in the lungs.1 They can also affect the soft tissue and visceral organs,2–6 and cases have been reported of their localisation in the mesentery, omentum, retroperitoneum, extremities, head and neck, genitourinary tract and other organs. Their presence in the stomach, however, is extremely rare. There are fewer than 20 cases of gastric involvement described in the literature, most of which are incidental findings or presentations with intestinal obstruction.3,4 Prognosis is unclear, but there have been case reports with recurrence or malignisation with metastasis. For this reason, treatment entails tumour resection; if this is not possible due to the location or involvement, chemotherapy or radiotherapy treatments are other options.3,5
We report the case of an 88-year-old male patient with a history of arterial hypertension, dyslipidaemia, an episode of acute myocardial infarction (resolved with a coronary stent), chronic atrial fibrillation treated with dicoumarol, and chronic obstructive pulmonary disease; his surgical history included elective cholecystectomy due to symptomatic bile stones at the age of 60. The patient came to the emergency room with oppressive abdominal pain, predominantly in the right hypochondrium and epigastrium, general malaise, nausea and vomiting. On physical examination, the patient was haemodynamically stable, with fever and jaundice of the skin and mucous membranes. The abdomen was soft, painful to palpation in the right hypochondrium and epigastrium with an uncertain Murphy sign; there were no palpated masses or enlargements, and no signs of peritoneal irritation. Analytical parameters showed haemoglobin (10.2g/dL), haematocrit 29.9%, elevated C reactive protein (3mg/dL) and a pattern of cholestasis (GGT 487IU/L, alkaline phosphatase 2013IU/L). Given the clinical suspicion of acute cholangitis, an abdominal ultrasound was ordered, which detected dilatation of the intrahepatic bile duct and proximal common bile duct, with an unclear image of biliary sludge. Having met the criteria for the Charcot triad, the patient was diagnosed with acute cholangitis and was admitted to the general surgery unit for a complete study and administration of endovenous antibiotic treatment.
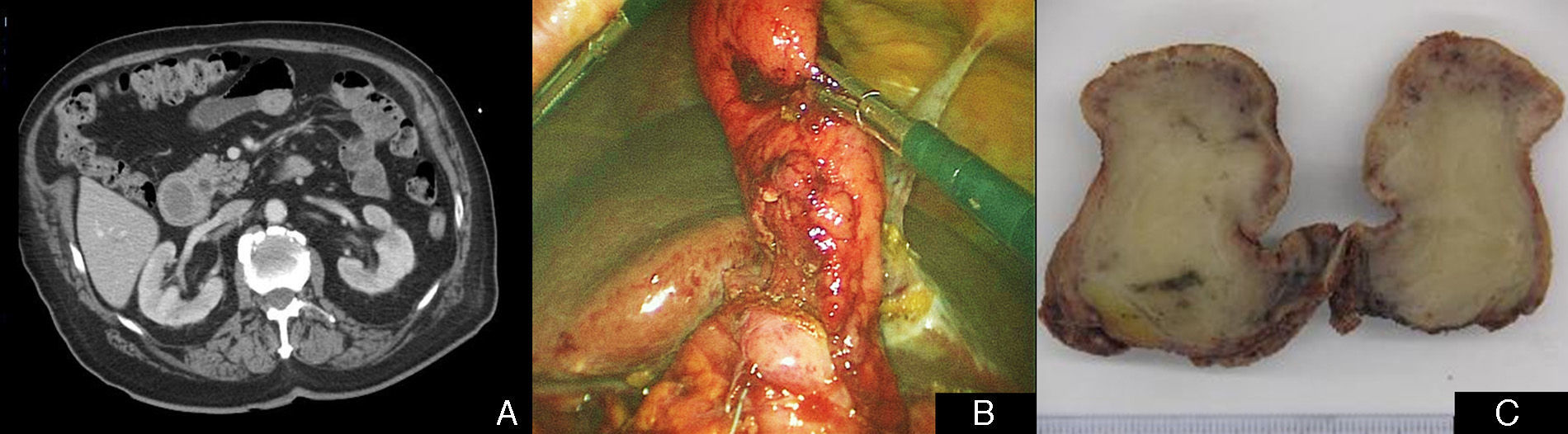
During hospitalisation, magnetic resonance cholangiopancreatography demonstrated a slightly dilated bile tract with no images of choledocholithiasis, which was interpreted as normal given the post-cholecystectomy status. Due to the persistence and intolerance of oral intake, a barium swallow study was ordered. This test showed adequate permeability of the oesophagus, stomach and duodenum, with some irregularities but no clear stenosis, as well as slowed intestinal transit. An associated motor disorder was suspected, and a gastroscopy was performed. This revealed a 2-cm polypoid lesion at the gastroduodenal junction that prolapsed towards the duodenum; biopsies were taken for a pathology study. This test was complemented with an extension study using thoracoabdominal computed tomography, which showed oedematous-looking wall thickening in the region of the bulb and the first-second parts of the duodenum (Fig. 1A). During hospitalisation, the jaundice progressively disappeared and the bilirubinaemia normalised, but an anaemia of 5g/dL of haemoglobin was detected with a drop of 13 points of haematocrit compared with the initial analyses, and no external evidence of bleeding. After blood transfusion, diagnostic-therapeutic gastroscopy was ordered because of the suspicion of gastrointestinal bleeding secondary to a gastroduodenal polyp. On this occasion, there was a 4-cm polypoid lesion that completely occupied the lumen of the duodenal bulb, extending to the proximal region of the second portion of the duodenum with traces of blood, which appeared to be prolapsed from the prepyloric antrum, forming a false pedicle. The papilla was identified, which presented a discharge of clear bile. Given the size and location, endoscopic resection was not possible, so we proceeded with laparoscopic surgical resection by means of gastroduodenostomy. The polyp was located in the gastric-pyloric region on a prolapsed gastric mucosa, so polypectomy was carried out with a Heineke-Mikulicz pyloroplasty (Fig. 1B). The macroscopic image is shown in Fig. 1C.
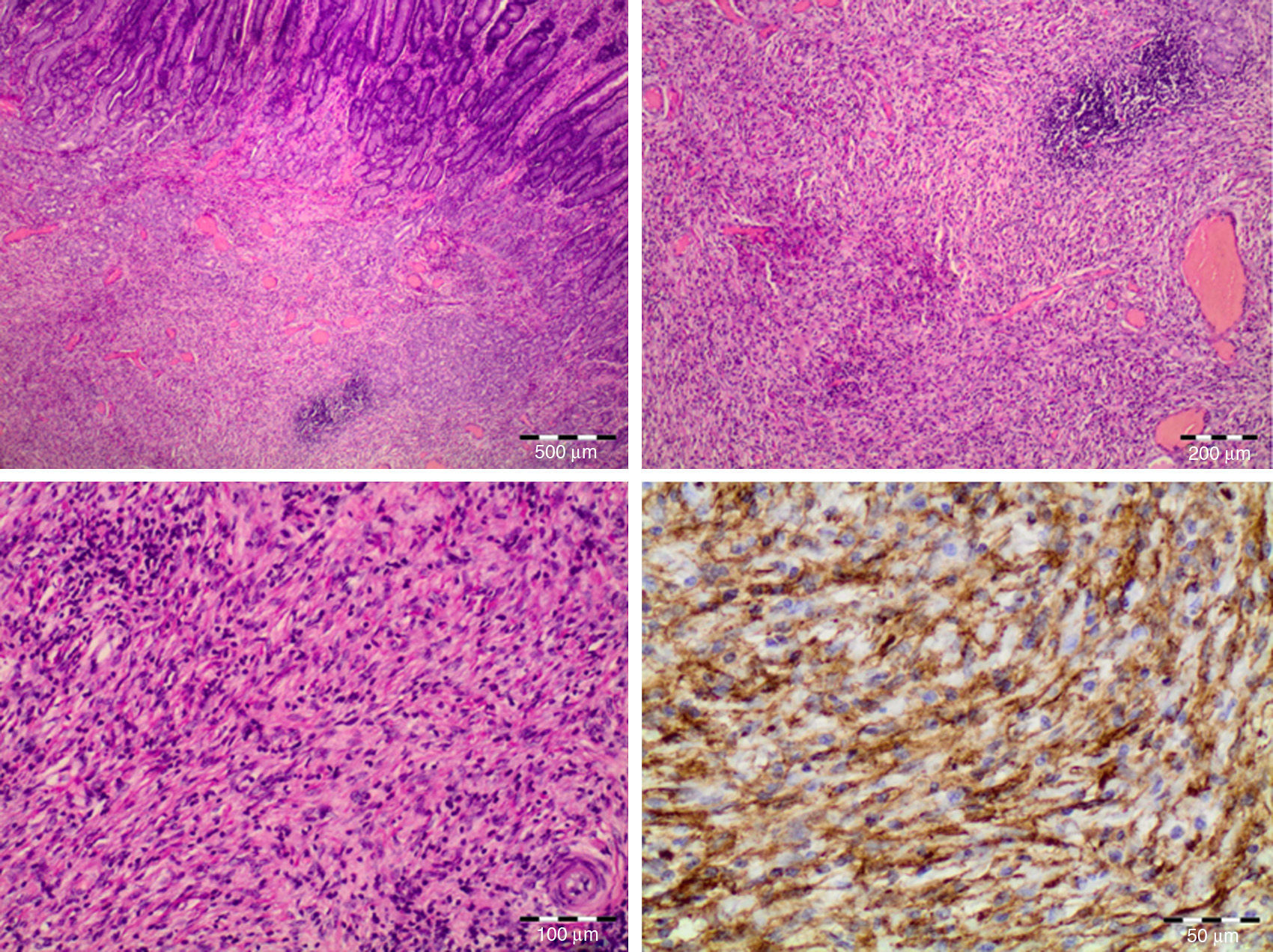
The patient progressed correctly, with adequate oral tolerance and disappearance of the abdominal pain. He was discharged from hospital on the 8th day post-op. The pathology report of the polyp reported a mass with morphological and immunohistochemical characteristics compatible with an inflammatory myofibroblastic tumour. Histologically, there was a proliferation of mesenchymal spindle cells mixed with inflammatory cells, predominantly lymphocytes. In the immunohistochemistry study, the tumour cells showed positive immunoreactivity for CD34 but negativity for CD117, desmin, smooth muscle actin and S-100. It was also positive for anaplastic lymphoma kinase (ALK) (Fig. 2).
Inflammatory myofibroblastic tumours are very uncommon and are also known as inflammatory pseudotumors. They are usually asymptomatic or run their course with nonspecific symptoms such as general malaise, abdominal pain, fever or weight loss. They typically affect children and young adults, with a higher prevalence in females (4:1). When adults are affected, it is usually in the 9th decade of life.7 The aetiology is unknown, although some support the hypothesis that it could be secondary to an infection, trauma, previous bile duct obstruction or surgical aggression.2,3,6 Histopathologically, these tumours are characterised by abundant inflammatory cells, fibroblasts and some collagen deposits.2,5 In the stomach, they are extremely rare. For their differentiation from gastrointestinal stromal tumours (GIST), immunohistochemistry should be used for confirmation4,6; even so, it may be negative for anaplastic lymphoma kinase protein.8 The evolution of this type of tumours is unpredictable: they can spontaneously regress or grow, become malignant or even metastasise.2,3,5,6 For this reason, surgical resection is considered the most effective treatment. In cases where complete resection is not possible or in patients with elevated morbidity, radiotherapy and chemotherapy should be used.3,5 The case we present occurred in an older adult patient who began with bile duct obstruction due to extrinsic compression, which triggered a series of symptoms that are unusual for this type of tumours: jaundice, fever, abdominal pain, intolerance to oral intake, and even acute anaemia due to the bleeding of the tumour itself. In conclusion, unpredictable progression of this type of masses should be considered in order to avoid underdiagnosis or undertreatment. In cases of inflammatory myofibroblastic tumour, treatment should involve complete exeresis when possible; if not, radiotherapy and chemotherapy are required. Post-adjuvant chemotherapy will depend on the baseline conditions of each patient.9
Please cite this article as: París-Sans M, Domènech-Calvet J, Raga-Carceller E, Sabench-Pereferrer F, del Castillo-Déjardin D. Tumor miofibroblástico inflamatorio gástrico como rara causa de obstrucción de la vía biliar. Cir Esp. 2016;94:188–190.