The synchronous presentation of abdominal aortic aneurysm (AAA) and colorectal cancer (CRC) is rare, with an estimated incidence of 0.49%–2% of AAA cases.1,2 There are several therapeutic options, but no accepted protocol has been established to date.
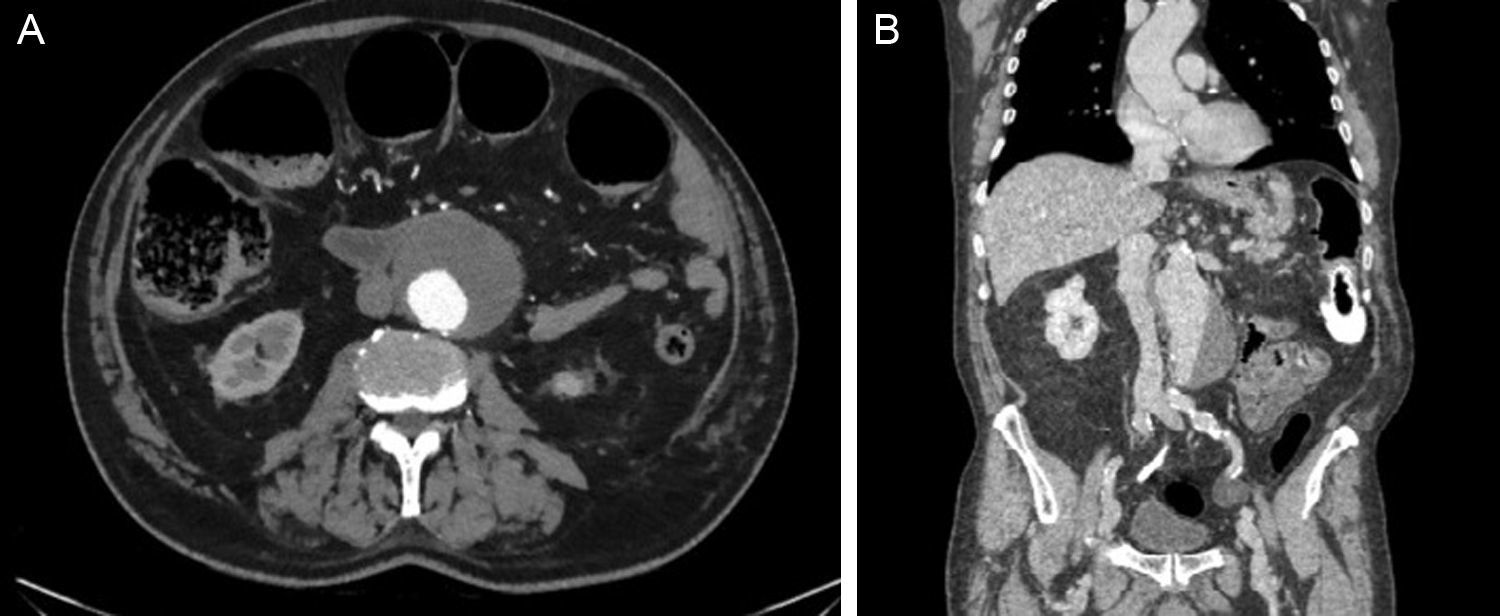
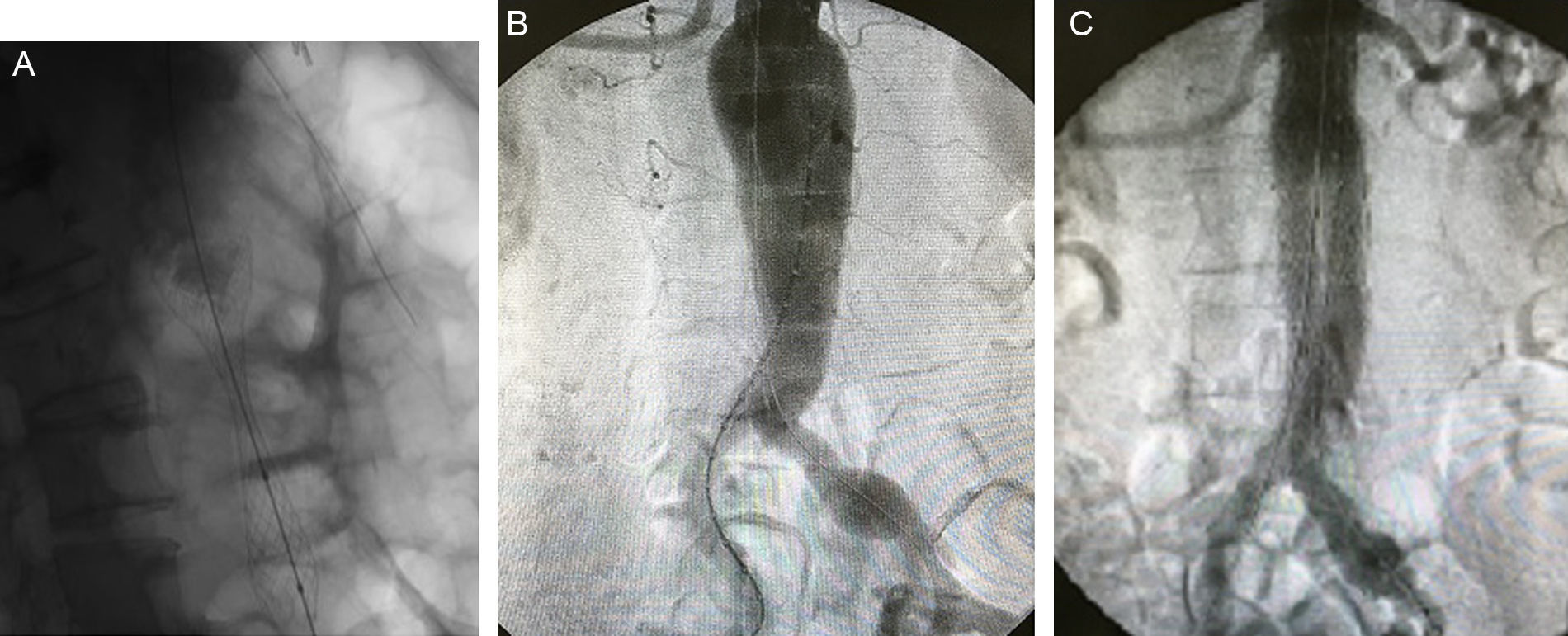
We present the case of an 83-year-old man with arterial hypertension, ischemic heart disease treated with percutaneous revascularization 9 years earlier, and Paget's disease. He came to the emergency room with symptoms of bowel obstruction, and computed tomography (CT) revealed a obstructive carcinoma of the descending colon, liver metastases in segments IV–VIII and VII, and asymptomatic infrarenal AAA measuring 6.4cm (Fig. 1). Given the clinical stability of the patient, a stent was placed in the colon, which resolved the obstructive symptoms. Afterwards, endovascular exclusion of the AAA was performed percutaneously with a bifurcated aortoiliac endoprosthesis, anchored in both common iliac arteries (C3® Excluder®, Gore® Medical), with no incidences or endoleaks (Fig. 2). Ten days later, a left hemicolectomy was performed along with resection of the liver metastases. The patient had a favorable postoperative course without complications, and the 3-month follow-up with CT angiogram showed no pathological findings.
In spite of the low incidence of the synchronous presentation of these diseases (0.49%–2% of AAA cases1,2), CRC represents 50% of cancers associated with AAA3 and 9%–13% of abdominal neoplasms.4 Its incidence is increasing due to population aging and the presence of common risk factors. Even so, treatment continues to be controversial.
After confirming the surgical indication of CRC (depending on its TNM classification5), we considered the need for operating the AAA. Since the publication by Szilagyi et al.6 in 1967, we are aware of the increased risk for AAA rupture associated with performing laparotomy secondary to the lysis of collagen induced by the intervention itself, nutritional depletion and surgical dissection, which is estimated at 6%–11%, especially if the AAA is larger than 5cm.1,2,5 Hence, the recommended treatment indication is stricter than in the general population, reducing the established diameter of 5.5cm7 or even disregarding it.1 Most authors concur in treating the AAA first in cases where it is symptomatic, even though these cases are rare.
Baxter et al.8 support the initial treatment of AAA if it is larger than 5cm. However, they observed a significant delay in the treatment of CRC, which was 122 days on average, and expected improved results with the development of endovascular techniques. More recently, Lin et al.4 concurred with this plan and defend the endovascular exclusion of AAA (EVAR) in infrarenal cases due to the significant decrease observed in intraoperative blood loss, hospital stay and CRC treatment delay, as well as higher 48-month survival.
If the anatomical characteristics are appropriate, Shalhoub et al.1 also defend the use of EVAR, although they recommend the initial treatment of AAA greater than 6cm after observing a lack of complications in smaller presentations. They also propose prior placement of a stent for the provisional treatment of cancer in cases of occlusion if the AAA is >6cm, thereby reducing the risk of rupture and prosthetic infection compared to open surgical resection. In our case, we followed this plan due to the clinical stability of the patient, which allowed us to perform EVAR and subsequent CRC resection, resulting in good patient progress.
When Porcellini et al.9 compared treatment with open surgery and EVAR in these patients, they also observed significant declines in mortality and morbidity rates (34% vs 0.0% and 21% vs 8%, respectively). Possible EVAR complications include branch thrombosis, which is why prostheses with the greatest possible flexibility are recommended. Furthermore, although the risk of ischemic colitis does not seem higher than with open surgery, it is necessary to maintain at least one hypogastric artery permeable as the inferior mesenteric artery will be occluded. This condition should always be ruled out before CRC resection.5 For patients with juxtarenal, pararenal or thoracoabdominal aneurysms, fenestrated and branched stent-grafts are starting to be used.
A single, combined intervention for the treatment of both diseases is also considered a technical option. The main disadvantages to note are the prolonged surgical time and the theoretical increase in the risk of contamination and infection,1,2,9 with high associated mortality (46%–65%).1,5 Although Minicozzi et al.3 did not observe increased mortality (4.2%), reoperation rate (3.3%) or stent infection (0.0%) after combined surgery, most authors recommend reserving this procedure for select cases, such as large or symptomatic AAA associated with CRC complicated with compromised vital functions requiring urgent surgery,5 as the associated mortality rate reaches 13%.10 Currently, the option of performing EVAR together with CRC resection during the same surgery is contemplated, although there have been few published case reports.
In our octogenarian patient with metastatic colon cancer and associated infrarenal AAA, the stent approach provided resolution of the acute bowel obstruction and facilitated the early treatment of AAA with EVAR and subsequent colon cancer treatment with open surgery. This staged approach could be of choice for this complex patient population.