Thoracoabdominal tumors are infrequent, and their situation in the aortic hiatus is exceptional. Their diagnosis and type of surgical approach usually present difficulties, mainly when these lesions have a thoracic component and an abdominal component through a natural diaphragmatic orifice.1
We present the cases of 2 patients with tumors in the posterior mediastinum, specifically in the aortic hiatus.
The first patient is a 75-year-old man who had undergone left adrenalectomy and complete splenectomy due to left pheochromocytoma 11 years ago. He presented with generalized tremor, asthenia and poorly controlled arterial hypertension (with medication) over the past 3 months. Computed tomography (CT) and magnetic resonance imaging (MRI) scans demonstrated a thoracoabdominal mass measuring 6cm in the aortic hiatus (Fig. 1). Blood analysis showed elevated levels of catecholamines, which suggested the diagnosis of secretory paraganglioma; therefore, treatment was initiated with alpha-adrenergic blockers. Prior to surgical intervention, arteriography identified the exit of the anterior spinal artery from the twelfth left intercostal artery. The same procedure included embolization of the distal vascular bed and trunk of the artery feeding the tumor.
The patient is a 76-year-old woman who was being monitored by the pulmonology department due to bronchial asthma. A follow-up CT scan identified a right para-aortic mass measuring 5cm with thoracic and abdominal components. Blood work showed no alterations. Prior to surgery, arteriography showed the outflow of the anterior spinal artery at the expense of the ninth left intercostal artery. No embolization was performed since no arterial branch was found to irrigate the tumor.
In both cases, a right video-assisted thoracoscopic approach (VATS) was performed under general anesthesia with selective intubation, while the patient was in the left lateral decubitus position at a forward inclination of 45°.
Two 10-mm trocars were used on the midaxillary line along with a 4-cm minithoracotomy on the posterior axillary line and ninth intercostal space.
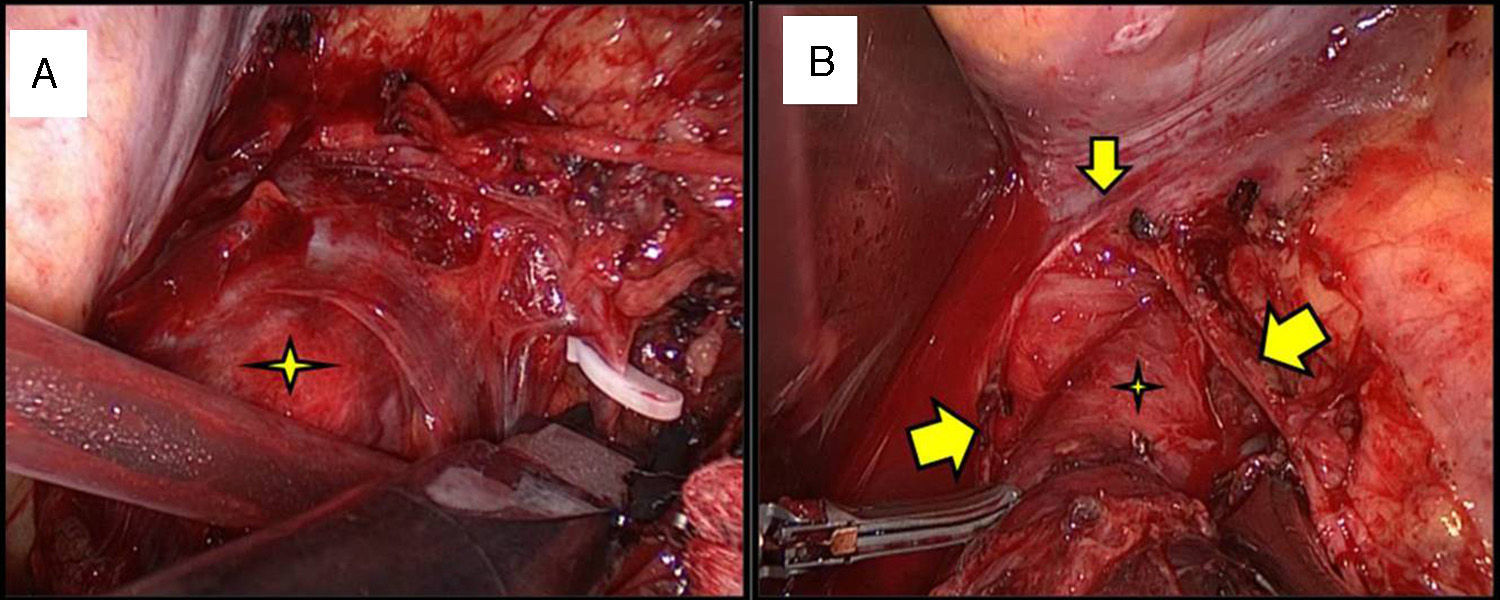
Initially, complete thoracoscopic exploration was performed with dissection of the triangular ligament. Adhesions were released, and vascular pedicles that were directly dependent on the aorta and the intercostal vessels were ligated (Fig. 2). The crura of the diaphragm were dissected to obtain better control of the lower pole of the tumor. In some sections, it was necessary to perform subadventitial dissection of the aorta to completely resect the tumor. In neither case the thoracic duct or signs of intraoperative lymphorrhagia were identified. A fibrin sealant was applied (to prevent possible lymphadenectasis) and a pleural drain was inserted.
(A) Ligature of multiple vascular pedicles dependent on the intercostal and direct aortic vessels. The tumor was drawn forward (star). The diaphragm, whitish in color, is at the right side of the image. (B) Dissection of the lower pole of the tumor (star) prior to opening the crura of the diaphragm (inverted V-shape; the dissection angle or end is marked with the smaller arrow and the edges with the larger arrows).
Mean surgical time was 3h and the hospital stay was 3 days in both cases. There were no intraoperative incidences or clinical/radiological signs of postoperative complications or recurrences (after follow-up ≥1.5 years).
The pathology study of the first case reported paraganglioma positive for chromogranin and synaptophysin antibodies, and the study of the second case revealed a benign schwannoma.
Both lesions were considered neurogenic tumors of the mediastinum, for which the treatment of choice is complete surgical resection.2 Surgery can be associated with a high risk of intraoperative hemorrhage secondary to tumor manipulation and the proximity of large vessels. To reduce this risk, some authors propose using arteriography for preoperative embolization of the main arterial pedicles.3–5 During the same procedure, they also recommend identifying the pathway of the anterior spinal artery (artery of Adamkiewicz) to avoid intraoperative injury. In 75% of cases, this is a branch of the last left intercostal arteries and is responsible for most of the spinal cord irrigation, therefore its injury can lead to irreversible spinal cord ischemia.6
The location of the tumor in the aortic hiatus raises doubts about the best type of surgical approach, since it can be performed by thoracotomy, laparotomy or minimally invasive techniques.
The laparoscopic approach is complex, requiring mobilization of the right hepatic lobe, opening of the hiatus and access to the posterior mediastinum with difficult vascular control. In addition, possible adhesions secondary to previous abdominal surgeries could make these maneuvers difficult, as in the first case described in this article. Laparotomy offers better vascular control than laparoscopy, although it requires a wide incision and mobilization of the viscera. In case of hemorrhage of the vascular pedicles in the thorax or thoracic aortic lesion, control from the abdomen seems insufficient and unsafe; therefore, the thoracic approach appears to be more indicated in these cases.
Thoracotomy provides a good operative field, and it is possible to expand to thoracophrenotomy or thoracophrenolaparotomy if needed.4 However, VATS offers excellent visualization of the aortic hiatus and control of tumor vascular pedicles, along with the added benefits of mini-invasive surgery (less pain, faster recovery, lower costs and fewer days of hospitalization).7 Video-assisted thoracoscopy should be indicated provided that it always meets criteria for oncologic resectability while maintaining patient safety, and conversion to thoracotomy is always a possible option.
We believe that preoperative arteriography (and embolization if needed) together with the VATS approach should be considered in cases of thoracoabdominal tumors located in the aortic hiatus since they allow us to treat this type of tumors with mini-invasive techniques, thereby reducing perioperative risk.
Please cite this article as: Rombolá CA, Crespo García del Castillo V, García Jiménez MD, Genovés Crespo M, García Blázquez E. Abordaje videotoracoscópico de tumores toracoabdominales situados en el hiato aórtico. Cir Esp. 2017;95:112–114.