We present the case of a 79-year-old male patient with a history of hypertension, paroxysmal atrial flutter, first-degree AV block, and non-obstructive carotid atheromatosis. His history of digestive disease included a Zenker's diverticulum diagnosed 5 years earlier and carcinoma in situ of the ascending colon that had been resected endoscopically.
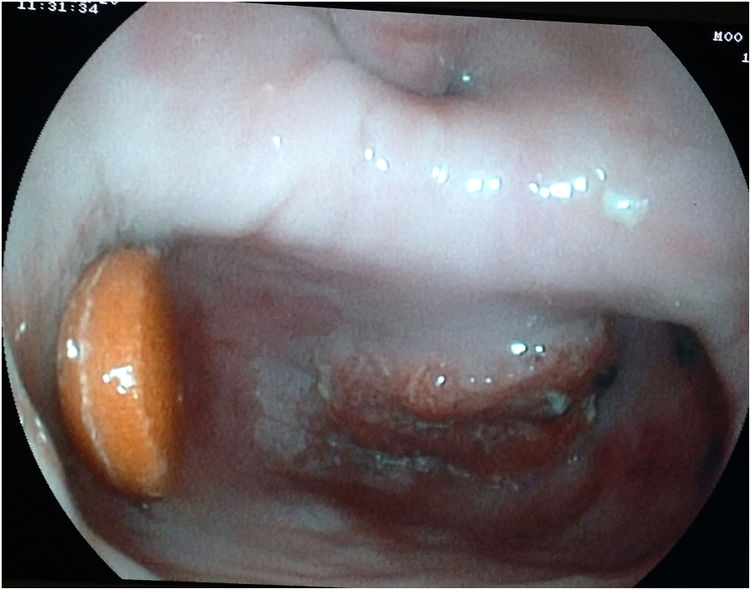
At a follow-up visit of the diverticulum, the patient reported increased regurgitation and cough. Esophagoscopy demonstrated a 4–5cm diverticulum with a tablet inside (Fig. 1), and on the anterior side, more than 1cm from the diverticular neck, a 2–3cm raised lesion was observed with a neoplastic appearance. The pathological study suggested the presence of infiltrating squamous cell carcinoma. The extension study computed tomography (CT) scan revealed nonspecific regional lymphadenopathies, with no other findings.
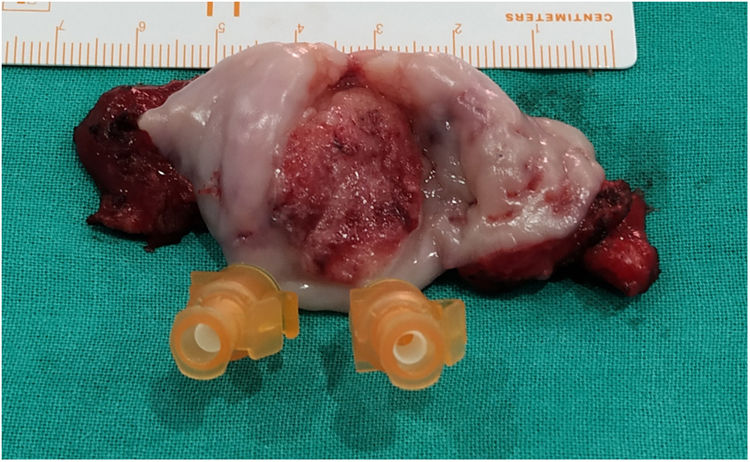
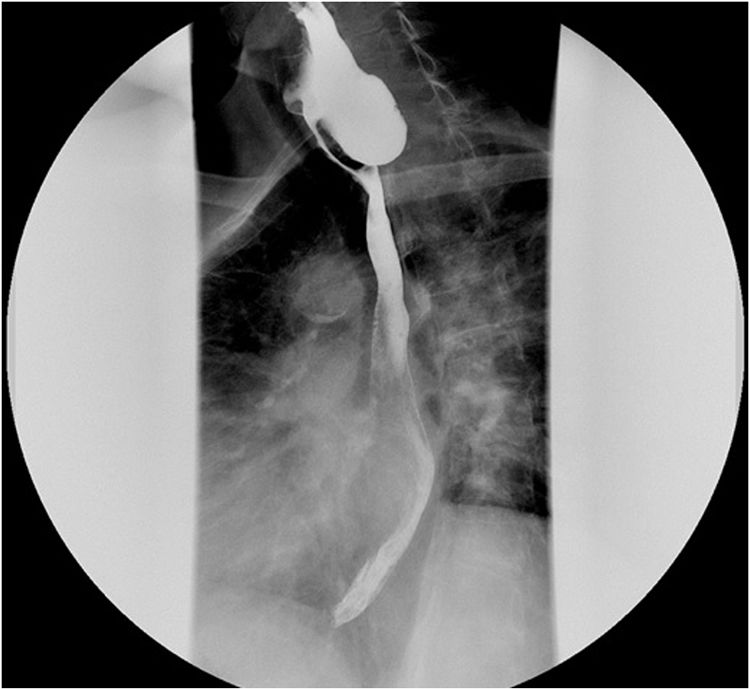
After diagnosis, the tumor committee ruled out neoadjuvant radiotherapy because of the mobility of the area and to reduce postoperative complications. Instead, they agreed to administer chemotherapy due to the size of the lesion and the risk of lymph node invasion. Subsequently, the patient underwent surgery, which began with a left cervical incision parallel to the anterior edge of the sternocleidomastoid muscle. During surgery, we observed a 3cm×2cm tumor that was limited to the diverticulum (Fig. 2) as well as a jugular lymphadenopathy, which was removed and studied intraoperatively, showing no evidence of malignancy. We performed diverticulectomy and cricopharyngeal myotomy. The postoperative period transpired without complications, and the patient was discharged on the 6th postoperative day (Fig. 3).
Follow-up office visits were scheduled after one, 3, 6 and 12 months. The patient remained asymptomatic, with a slight weight gain and no progression observed in the tests performed (UGI series and CT). The pathological study reported a well-differentiated epidermoid carcinoma with invasion to the adventitia, and surgical margins were free of involvement (pT3N0).
Malignant degeneration is a rare complication of pharyngeal diverticula, with an incidence reported in the literature ranging from 0.3% to 7%.1 The first description was by Halstead in 1904. Since then, publications have been scarce, and most have been isolated case reports, so there is no consensus regarding its management.
Risk factors for malignization of a diverticulum include advanced age, male sex, large size, and long-term progression of the diverticulum.2 The latter is the main predisposing factor due to chronic irritation of the diverticular lining caused by food retention.3
The most common histological type is epidermoid carcinoma, with different degrees of differentiation. Although less frequent, benign in situ lesions have also been described inside the diverticulum.4
Typical symptoms of a Zenker's diverticulum are dysphagia, regurgitation, weight loss, fetor, cervical gurgling sounds, cough, and aspiration,5 although some presentations may be asymptomatic. There does not seem to be a direct relationship between the duration of diverticulum symptoms and malignancy.6
Symptoms that suggest possible malignancy include worsening dysphagia, regurgitation7 (sometimes with remnants of blood5,8,9), and/or significant weight loss.6 Pain is an unusual symptom, but it is highly suggestive of malignancy.3
In many cases, the diagnosis is incidental during surgery or after the anatomopathological study of the piece.3 Useful complementary tests for diagnosis are the barium swallow and esophagoscopy.3,10 Loss of definition in the contour of the diverticulum seen in the esophagogram is a suspicious sign of a lesion,5,9 although this sign can be imitated by the presence of content and may have a later onset. Other methods have been suggested, such as the cytological examination of the material aspirated from the diverticulum endoscopically.8
Esophagoscopy provides direct visualization of the mucosa and allows for biopsies to be taken, although it can have serious complications, such as perforation of the diverticulum.
The tests of choice for the diagnosis of extension are CT scan and magnetic resonance imaging, although there is little experience in this regard.
Curative treatment requires surgery, which is often sufficient in lesions confined to the diverticulum wall.9
The role of chemotherapy and radiotherapy is highly controversial,7 and they have been shown to be most effective in tumors with squamous cell histology. They also can be of value as palliative treatment in inoperable patients. In addition, they may be useful as neoadjuvant treatment with the aim of cytoreduction, either associated or not. Their indication as adjuvant treatment after surgery is highly debated, although some authors believe that they could be valid in cases of borderline tumors versus other more aggressive surgical strategies.3
In cases in which the tumor infiltrates the diverticular neck or invades neighboring structures, more extensive resections are indicated, and 5-year survival in these cases is less than 10%.3
Patients with Zenker's diverticula must be carefully monitored before and after surgical treatment since a carcinoma can develop even after resection of the diverticulum.2
In conclusion, despite the low incidence of carcinoma in Zenker's diverticulum, it must be considered in the differential diagnosis, especially in patients with long-term diverticula or changes in symptoms, in whom esophagoscopy and barium swallow should be performed. If diagnosed, surgery is recommended depending on the stage, which may or may not be associated with chemo-radiotherapy.
Please cite this article as: Luengo Ballester O, Usero Rebollo S, Rueda Martínez JL, Abad Martínez M, García Blázquez E. Carcinoma epidermoide sobre divertículo de Zenker. Cir Esp. 2021;99:241–242.