Lymphomas are neoplastic processes of the lymphocytes.1 They are classified as Hodgkin disease (Hodgkin lymphoma), which represents 25% of lymphomas, or non-Hodgkin lymphoma (NHL), which account for approximately 75% of all lymphomas.2 NHL can affect any lymphoid organ: lymph nodes, spleen, gastrointestinal tract, bone marrow and skin.3 Although splenic involvement in patients with NHL is between 50% and 60%, primary NHL of the spleen is a rare disease with an incidence of less than 1% in the general population.4
We present the case of a 50-year-old male patient with autosomal dominant polycystic kidney disease and developing chronic kidney disease (CKD) who was referred to us from the nephrology outpatient setting due to the finding of hypercalcemia (13.5mg/dL) and a decline in kidney function (creatinine 4.2mg/dL, after a previous value of 2.8mg/dL). He reported paresthesia in the lower right limb associated with night sweats, asthenia and unquantified weight loss. On examination, he was conscious and responsive, afebrile (35.8°C), with BP 143/84mmHg, HR 62 bpm, and SatO2 97%. In the abdomen, a mass was palpated in the upper left quadrant. No palpable lateral cervical, axillary, or inguinal lymphadenopathies were observed.
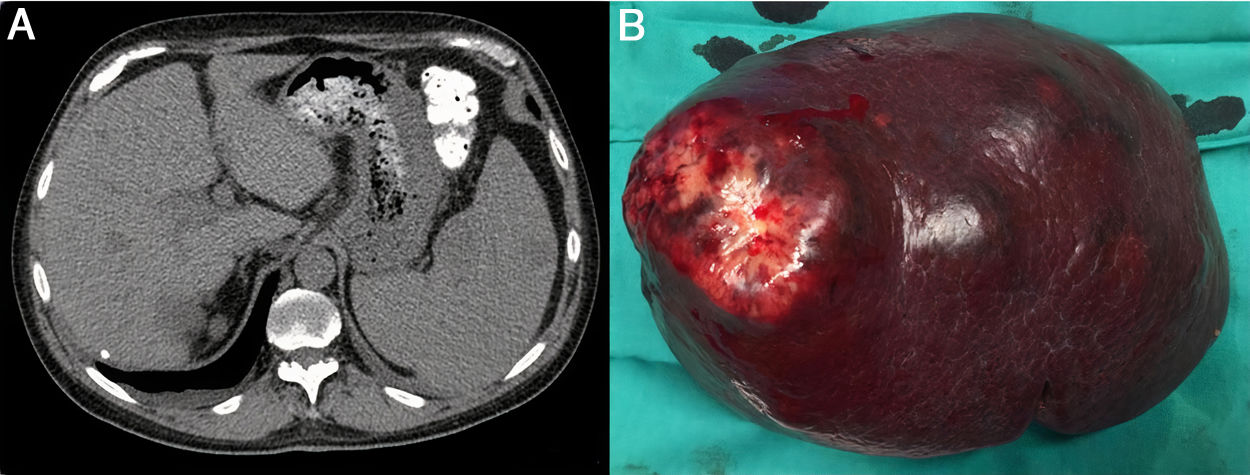
Blood tests revealed: hemoglobin 12.6g/dL, hematocrit 38%, MCV 85.4 fL, LDH 407 U/L, and platelet count 114×109/L. Abdominal computed tomography (CT) scan showed an enlarged spleen (16cm) with heterogeneous nodules of up to 5.5cm (Fig. 1). Positron emission tomography (PET) detected multiple hypodense lesions in the spleen, with a maximum SUV of 17.8 and no evidence of peripheral lymphadenopathy.
Despite treatment with zoledronic acid (4mg in a single dose), calcitonin 100 IU/mL every 12h, and methylprednisolone 20mg every 24h, hypercalcemia persisted with suppressed parathyroid hormone (11.3mg/dL), finding no lytic images on imaging tests.
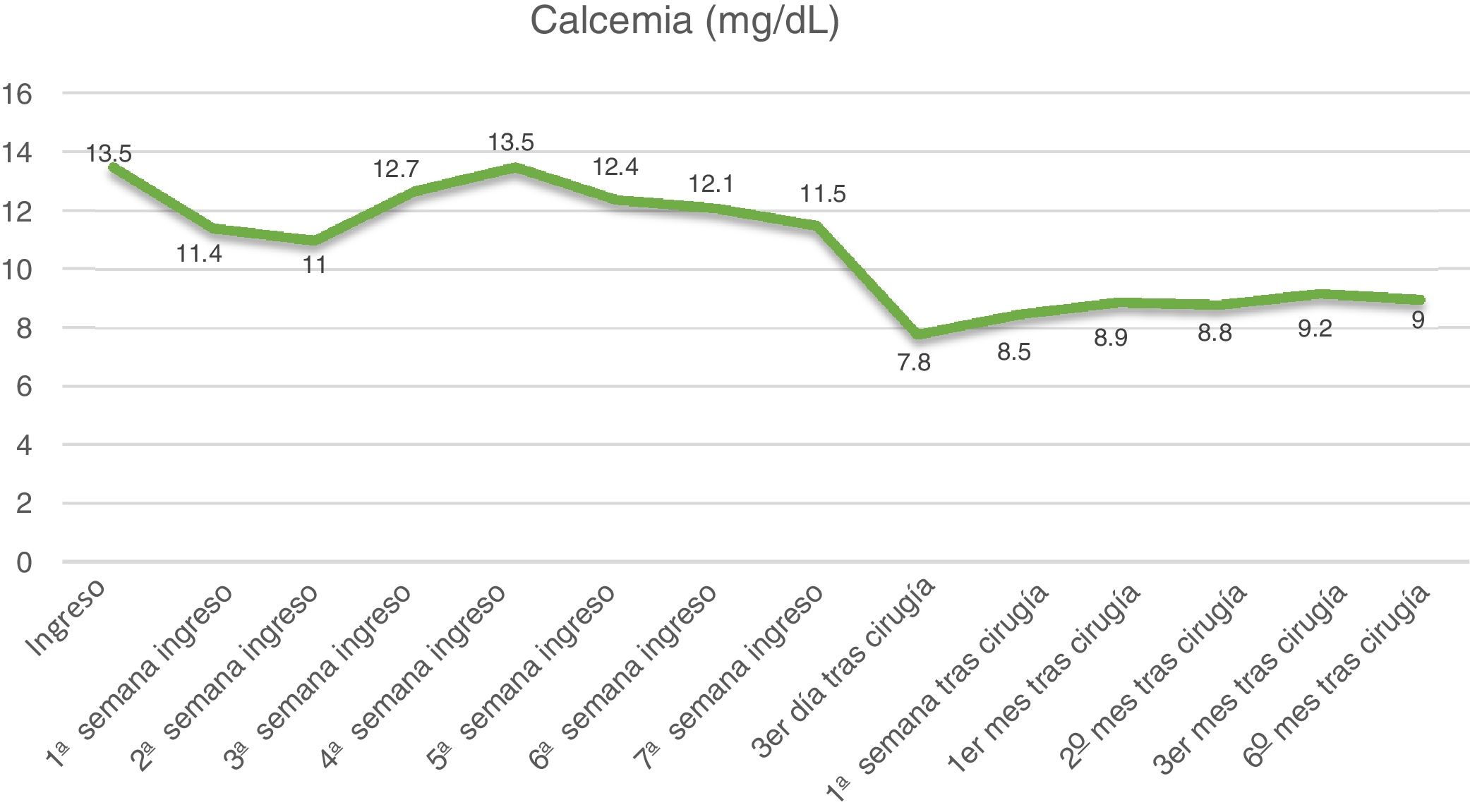
Given the suspicion of a splenic lymphoproliferative neoplastic process that associated hypercalcemia as a paraneoplastic syndrome, we decided to perform splenectomy which, in addition to establishing the definitive diagnosis by histological study of the specimen, would be the treatment of choice if the diagnosis of splenic lymphoma was confirmed. Using a left subcostal laparotomy, we observed a large spleen with multiple nodules that were stone-like in consistency, the largest of which was in the upper pole. Splenectomy was performed without incident (Fig. 1b). The histological study reported the diagnosis of a germinal center diffuse large B-cell NHL. The immunohistochemical study revealed positivity for CD20, BCL-2 and BCL-6 with a Ki67 cell proliferation marker of 80%.
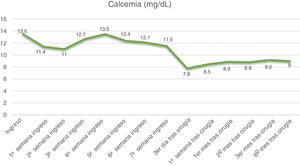
After surgery, the patient's progress was favorable, and calcium levels progressively normalized. He received 6 cycles of chemotherapy treatment following the R-CHOP scheme (rituximab associated with cyclophosphamide, doxorubicin, vincristine and prednisone), and is currently in remission. Fig. 2 shows the evolution of the calcium levels during admission and after surgery.
Primary NHL of the spleen is a rare entity, even more so if we consider the characteristics of this patient (who presented hypercalcemia despite CKD), so there are hardly any published cases. Diagnosis requires involvement of the spleen, either with or without splenomegaly and/or involvement of two cell lines (bicytopenia) in the absence of peripheral lymphadenopathies,4 which are criteria present in this case.
Symptoms are usually nonspecific, and some patients may be asymptomatic. On physical examination, splenomegaly is a frequent finding, together with the absence of peripheral lymphadenopathy. The most frequent laboratory abnormalities include anemia, thrombocytopenia, or leukopenia, with an increase in acute phase reactants and LDH.5 In our case, the patient presented anemia, thrombocytopenia, and elevated LDH.
Hypercalcemia is the most common paraneoplastic syndrome and is associated with epidermoid carcinoma of the lung, breast carcinoma, multiple myeloma, and lymphoma.6 However, the presence of hypercalcemia in B-cell NHL is rare (7%–8% of cases),7 and even more so in this case because CKD usually presents with hypocalcemia. Other possible causes of hypercalcemia associated with renal failure include multiple myeloma and the recovery phase of rhabdomyolysis, although in these cases renal failure is acute.8
The imaging tests of choice are ultrasound and CT, while PET is used to assess lymph node involvement, which would rule out the diagnosis of primary NHL of the spleen.9 Splenectomy is the treatment of choice because it is therapeutic and also establishes the definitive diagnosis. It can be performed by open surgery or laparoscopy, which has shown numerous advantages when performed by experienced surgeons. Subsequently, adjuvant therapy depends on the stage of the disease.10
Primary NHL of the spleen is a rare pathology, and its nonspecific symptoms make its diagnosis difficult. Imaging studies play a fundamental role, and the treatment of choice is splenectomy.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: López Morales P, Terol-Garaulet E, Méndez-Martínez M, Iniesta-Pino Alcázar I, Albarracín-Marín-Blazquez A. Hipercalcemia como manifestación inicial de linfoma primario esplénico difuso de células grandes B. Cir Esp. 2021;99:238–240.