Difference analysis of ambulatorization rate, pain, analgesic requirements and daily activities recovery in patients undergoing laparoscopic cholecystectomy with standard multiport access (CLMP) versus a minilaparoscopic, 3mm size, technique.
MethodsProspective randomized trial of 40 consecutive patients undergoing laparoscopic cholecystectomy. Comparison criteria included predictive ultrasound factors of difficult cholecystectomy, previous history of complicated biliary disease and demographics. Results are analysed in terms of ambulatorization rate, pain, analgesic requirements, postoperative recovery, technical difficulty, haemorrhage intensity, overnight stay, readmission rate and total or partial conversion.
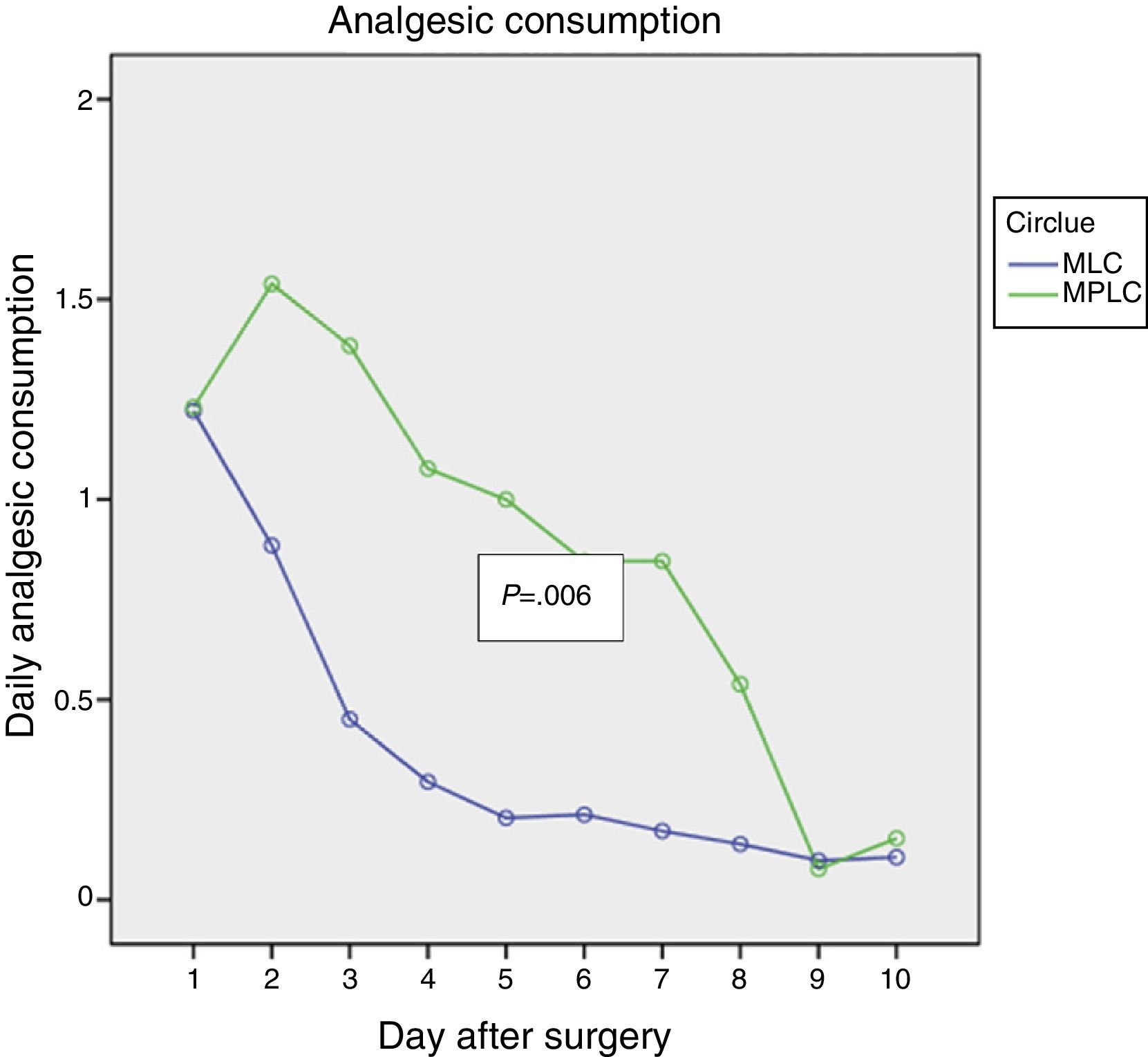
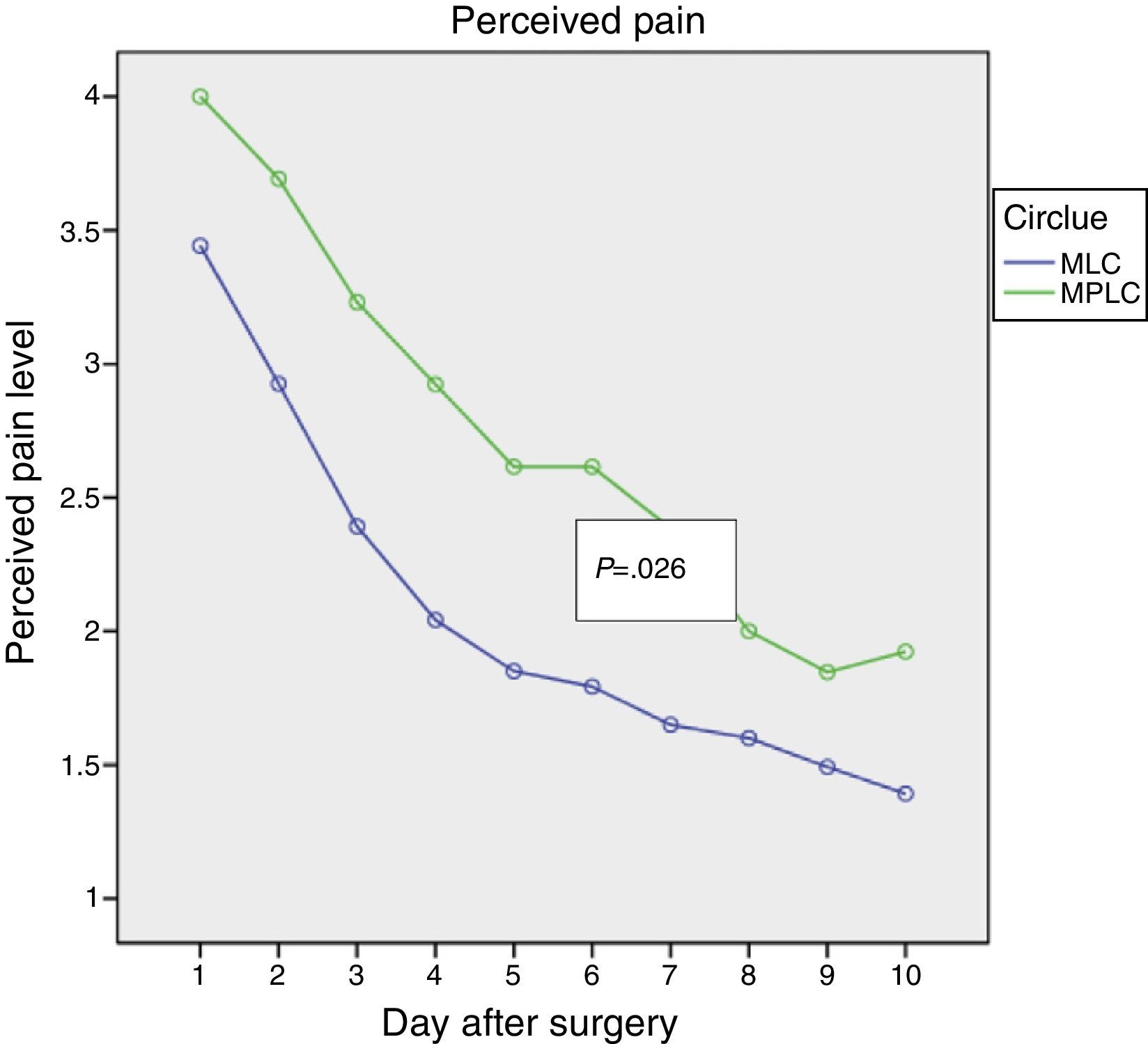
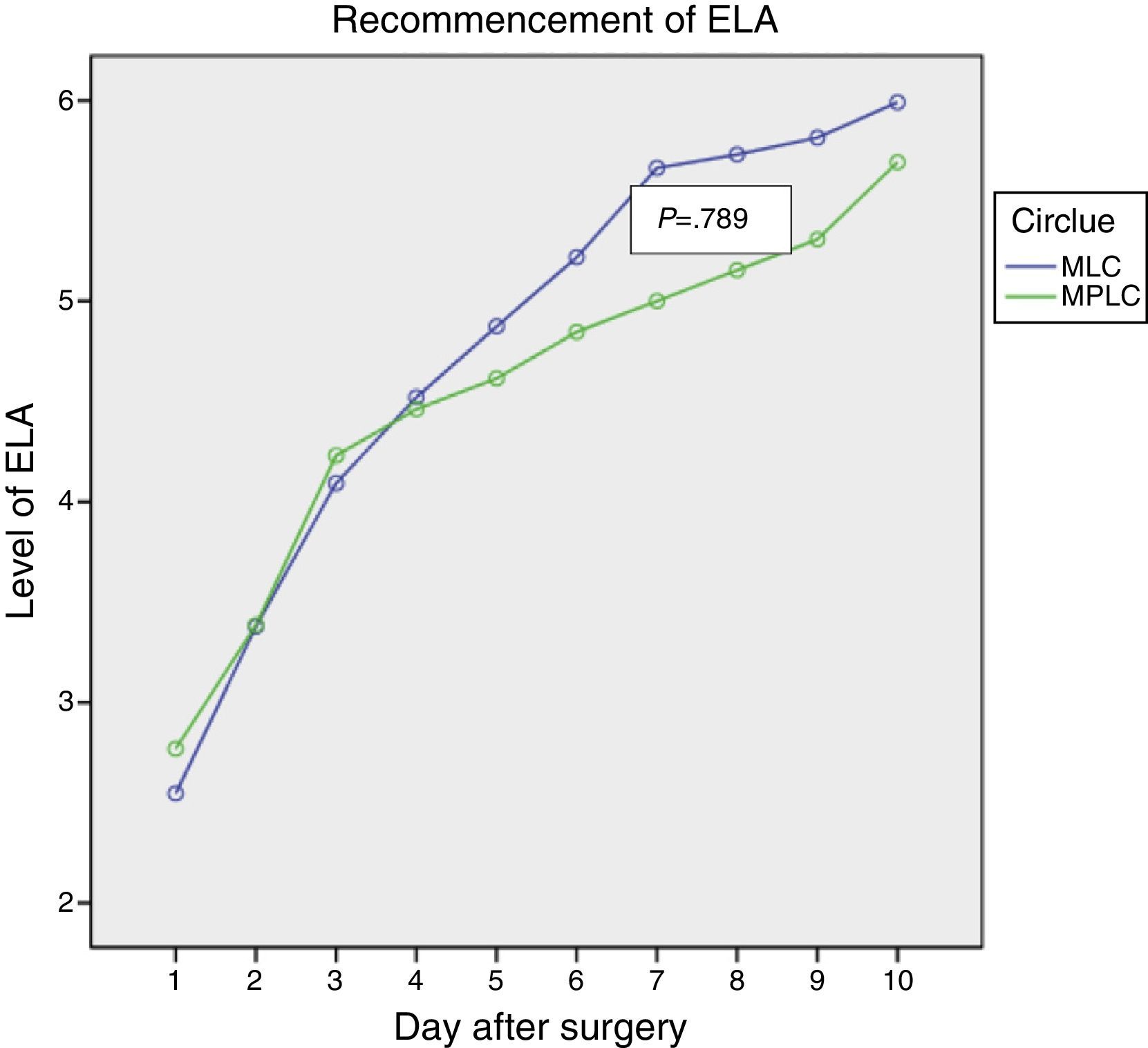
ResultsBoth procedures were similar in surgery time, technical score and haemorrhage score. MLC was associated with similar ambulatorization rate, 85%, and over-night stay 15%, with only 15% partial conversion rate. MLC showed less postoperative pain (P=.026), less analgesic consumption (P=.006) and similar DAR (P=.879).
ConclusionsMLC is similar to CLMP in terms of ambulatorization with less postoperative pain and analgesic requirements without differences in postoperative recovery.
Determinar la existencia de diferencias en tasa de ambulatorización, dolor percibido, consumo de analgésicos y recuperación de las actividades de la vida diaria (AVD) en pacientes tratados mediante colecistectomía laparoscópica multipuerto (CLMP) y colecistectomía por minilaparoscopia con material de 3mm (MLC).
MétodoEstudio prospectivo aleatorizado de 40 pacientes consecutivos tratados mediante colecistectomía laparoscópica. Los criterios de pareamiento incluyeron factores ecográficos predictivos de colecistectomía técnicamente dificultosa, historia previa de enfermedad biliar complicada y factores demográficos. Se analizan los resultados en términos de tasa de ambulatorización, dolor percibido, consumo de analgésicos, recuperación de las AVD, grado de dificultad técnica, grado de hemorragia asociada, tasa de ambulatorización, porcentaje de estancia over-night, reingresos y conversión parcial o total.
ResultadosAmbos procedimientos mostraron similar duración de intervención, puntuación de dificultad técnica y de hemorragia. La MLC mostró porcentaje similar de ambulatorización (85%) y de estancia over-night (15%), con solo un 15% de conversiones parciales y 0% de conversión a CLMP. La MLC mostró menor dolor postoperatorio (p=0,026), menor consumo de analgésicos (p=0,006) con similar recuperación de las AVD (p=0,879).
ConclusionesLa MLC no es inferior a la CLMP en términos de ambulatorización, resultando en menor dolor postoperatorio y menor consumo de analgésicos, con similar resultado en cuanto a reincorporación a las AVD.
Over recent years surgeons have tried to improve the results of surgery by reducing pain, especially incision pain, shortening hospitalisation, increasing the speed of recovery of everyday life activities (ELA) and improving aesthetic results by reducing the number and size of incisions. Two procedures have been proposed instead of traditional multiport cholecystectomy (MPLC): minilaparoscopic cholecystectomy (MLC) and single port laparoscopic cholecystectomy (SPLC). The theoretical basis for this is that, by using fewer smaller ports the degree of invasiveness is minimised and the surgical result is potentially better.1 The disadvantages associated with this minimisation include the longer time taken for both surgical procedures, an increase in the incidence of hernia and a higher rate of complications (SPLC). Postoperative pain is also potentially greater due to an incision longer than 10mm in cases of SPLC.2
In both cases the aim of these alternatives to MPLC is to reduce hospitalisation and convalescence times, reducing direct and indirect costs and also improving aesthetic results. The potential benefits, safety and reliability of MLC were established by small series in 1990, although interest has resurged due to the development of SPLC and the appearance of new 3mm instrumentation.
MethodsThis is a prospective randomized study of 40 consecutive patients treated by laparoscopic cholecystectomy. This work was undertaken in the ICAD (Department of General and Digestive Surgery) of Quirón Hospital, Valencia, following authorisation by the Quirón Hospital ethics and quality committee. The chief aim of the study was to show that MLC is able to keep rates of outpatient treatment that are similar or not lower than those achieved by MPLC. The secondary objectives included analysis of the repercussions of MLC in comparison with MPLC in terms of perceived pain, analgesic consumption and the recommencement of ELA. The randomisation system was based on order of inclusion in the surgical waiting list, and cases were recruited on an intention to treat (ITT) basis except when cases were excluded due to sclero-atrophic gallbladder and morbid obesity. The study commenced in May 2012 and finished in December 2012. The exclusion criteria were: ASA III, morbid obesity, ERCP-EE 15 days prior to surgery, chronic use of analgesic medication, depression, chronic anxiety or a history of alcoholism or drug addiction, the suspicion of choledocholithiasis based on ultrasound or the analytical profile confirmed by NMR-cholangiography and preoperative ultrasound diagnosis of sclero-atrophic gallbladder. Regarding the biliary disease no case was excluded due to a history of cholecystitis or pancreatitis. The first 15 cases in which MLC was used were also excluded from the study, i.e., the cases in the learning curve. This was to ensure surgical strategy in this procedure had been optimised in connection with the trocars, optical equipment and clamping alternatives to be used.
Surgical TechniqueThe operations were performed by the same surgical and anaesthetic team. The standard French technique with 4 trocars (2 of 10 and 2 of 5mm) was used in the MPLC group. MLC was performed in the following way: open pneumoperitoneum with a supraumbilical Hasson trocar and 3 3mm trocars with 5mm optics (Karl Storz). The 5mm endoclip was inserted parallel to the 5mm optics through the Hasson trocar at the moment the hilus was clamped, as it if were a single port. The gallbladder was extracted by inserting a 3mm traction clamp parallel with the 5mm optics through the Hasson trocar, or by displacing the gallbladder with the 3mm trocar clamp from the left hypochondrium to the umbilical incision using direct vision. In the case of intraoperative perforation of the gallbladder the extraction took place with a bag.
Partial conversion was considered to take place (changing any of the 3mm trocars for an alternative) when it was necessary to replace the 3mm left hypochondrium trocar with a 5mm one to clamp the elements of the hilus.
The 10mm optics was rejected at the start of the experience after it was found to give no better view than the 5mm device. Equally, the 3mm optics was also rejected as it offered a very limited quality view that did not permit the safe clamping of the elements of the hilus.
MLC with a transumbilical 5mm port was rejected at the start of our experience due to the need to create an abdominal wound that permitted the extraction of a gallbladder containing calculi, so it was replaced with the port using a 10mm trocar.
In no case was intraoperative cholangiography used.
In both groups pre-incision wounds were infiltrated using bupivacaine. Intraperitoneal bupivacaine was administered before dissecting in the area of the hilus, and at the end of the procedure an icodextrin solution with intraperitoneal bupivacaine was administered to reduce visceral pain (somatovisceral blocking). Patients followed a fast track recovery procedure and were discharged within 6h of their surgical operation.3 The estimation of the potential technical difficulty before operating (positive ultrasound or ultrasound factors predictive of technically difficult cholecystectomy) was based on quantification of the ultrasound Surgical Complexity Classification Index (SCCI) previously published by our group.4 Intraoperative technical difficulty was quantified by a technical scoring system and the degree of haemorrhage detected, as previously published by our group.5
Partial conversion was defined as the need to change one or more 5mm or 10mm trocars, while complete conversion was defined as the need to transform the procedure to MPLC, and conversion was the need for laparotomy.
Pain EvaluationPatients were asked to keep a diary of postoperative pain after surgery, showing their consumption of analgesics and recommencement of ELA during a total of 20 days. This diary had been published beforehand by our group.6
Statistical AnalysisThe groups were compared by using the Mann–Whitney test for continuous variables and the chi squared test for the comparison of discrete variables. Data are presented as average and range, or standard deviation or percentages, depending on which was appropriate. Perceived pain, analgesic consumption and the recommencement of ELA were compared by repeated ANOVA measurements.
ResultsPatient recruitment was terminated after 20 cases due to the detection of significant differences in the perceived pain parameters and analgesic consumption in the preliminary analyses. It was also found that the rate of outpatient treatment remained the same with no increase in the complications associated with the MLC procedure, so that, in methodological terms, this study must be considered to be a comparative prospective pilot study.
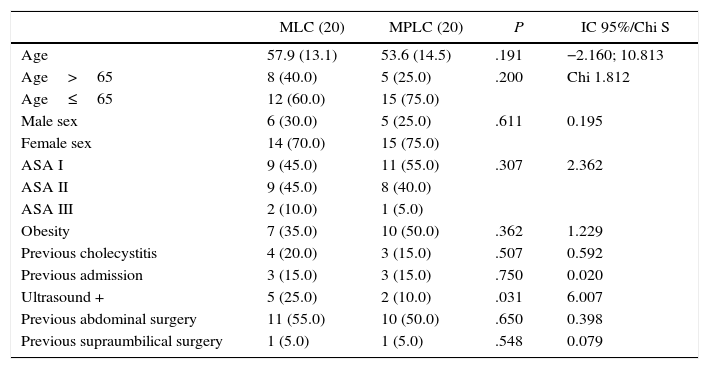
Table 1 shows the demographic data of the 2 groups analysed. There were no differences in age, sex, ASA classification or associated obesity. The histories of complicated biliary disease were similar in both groups, as were the percentages of patients who had required admission beforehand for this reason. There were more ultrasound findings suggestive of a technically difficult cholecystectomy (wall thickening, a hardly distended gallbladder, calculi larger than 3cm, infundibular calculi) in the MLC group. Nor were there any differences in the percentage of previous abdominal or supramesocolic surgery.
Demographic Data.
| MLC (20) | MPLC (20) | P | IC 95%/Chi S | |
|---|---|---|---|---|
| Age | 57.9 (13.1) | 53.6 (14.5) | .191 | −2.160; 10.813 |
| Age>65 | 8 (40.0) | 5 (25.0) | .200 | Chi 1.812 |
| Age≤65 | 12 (60.0) | 15 (75.0) | ||
| Male sex | 6 (30.0) | 5 (25.0) | .611 | 0.195 |
| Female sex | 14 (70.0) | 15 (75.0) | ||
| ASA I | 9 (45.0) | 11 (55.0) | .307 | 2.362 |
| ASA II | 9 (45.0) | 8 (40.0) | ||
| ASA III | 2 (10.0) | 1 (5.0) | ||
| Obesity | 7 (35.0) | 10 (50.0) | .362 | 1.229 |
| Previous cholecystitis | 4 (20.0) | 3 (15.0) | .507 | 0.592 |
| Previous admission | 3 (15.0) | 3 (15.0) | .750 | 0.020 |
| Ultrasound + | 5 (25.0) | 2 (10.0) | .031 | 6.007 |
| Previous abdominal surgery | 11 (55.0) | 10 (50.0) | .650 | 0.398 |
| Previous supraumbilical surgery | 1 (5.0) | 1 (5.0) | .548 | 0.079 |
Ultrasound +: ultrasound factors predictive of a technically difficult cholecystectomy.4
Preoperative analytical values for hepatic functioning and inflammatory tests (fibrinogen) showed no significant differences between both groups.
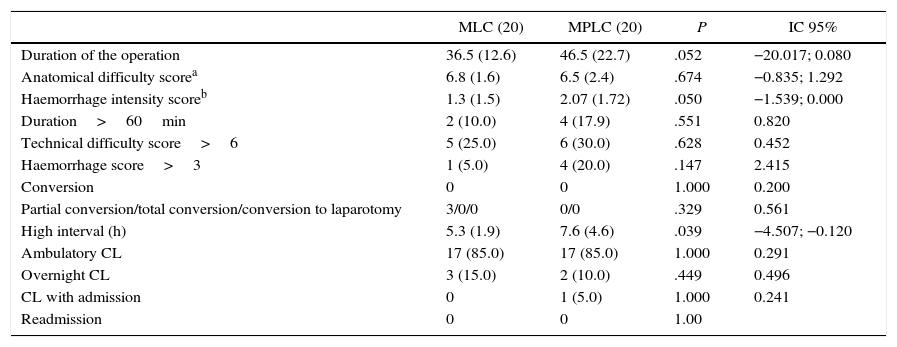
Table 2 shows the results variables analysed. The duration of the operation was similar in both procedures, with similar percentages of operations lasting more than 1h. There were no differences in the degree of technical difficulty (scoring in a range of from 6 to 18) or intraoperative haemorrhage. Although there were no conversions to laparotomy, there were 3 partial conversions in the ML group (due to the need for an additional 5mm trocar because of difficulty in exposing the gallbladder hilus at the moment of clamping). Clamping with a 5mm endoclip parallel to the 5mm optics caused the latter to bend, and eventually it had to be replaced because of this damage. The time to patient discharge was significantly shorter in the MLC group, although the percentage of outpatient treatment was similar in both groups. There were no readmissions in either of the groups studied.
Results.
| MLC (20) | MPLC (20) | P | IC 95% | |
|---|---|---|---|---|
| Duration of the operation | 36.5 (12.6) | 46.5 (22.7) | .052 | −20.017; 0.080 |
| Anatomical difficulty scorea | 6.8 (1.6) | 6.5 (2.4) | .674 | −0.835; 1.292 |
| Haemorrhage intensity scoreb | 1.3 (1.5) | 2.07 (1.72) | .050 | −1.539; 0.000 |
| Duration>60min | 2 (10.0) | 4 (17.9) | .551 | 0.820 |
| Technical difficulty score>6 | 5 (25.0) | 6 (30.0) | .628 | 0.452 |
| Haemorrhage score>3 | 1 (5.0) | 4 (20.0) | .147 | 2.415 |
| Conversion | 0 | 0 | 1.000 | 0.200 |
| Partial conversion/total conversion/conversion to laparotomy | 3/0/0 | 0/0 | .329 | 0.561 |
| High interval (h) | 5.3 (1.9) | 7.6 (4.6) | .039 | −4.507; −0.120 |
| Ambulatory CL | 17 (85.0) | 17 (85.0) | 1.000 | 0.291 |
| Overnight CL | 3 (15.0) | 2 (10.0) | .449 | 0.496 |
| CL with admission | 0 | 1 (5.0) | 1.000 | 0.241 |
| Readmission | 0 | 0 | 1.00 |
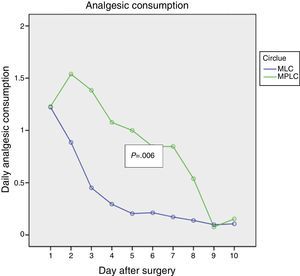
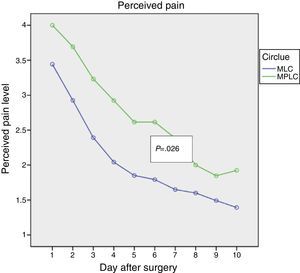
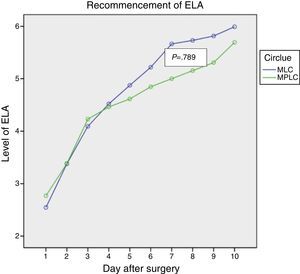
Figs. 1–3 show the results in terms of perceived pain, analgesic consumption and recommencing ELA. Repeated measurements variance analysis showed significant differences in favour of MLC in comparison with MPLC for perceived pain (0.026) and analgesic consumption (0.006), and no differences in connection with recommencing ELA (0.879).
In CL the pain of the incision predominates over the visceral pain and omalgia. This is so for intensity as well as incidence in the first week after surgery.7 The first study by Bisgaard8 was interrupted due to the high rate of conversion to MPLC because of problems with seizing, pulling and exposing secondary to inflammation of the gallbladder, as this analysis was undertaken in ITT with no patient selection. Although no statistically significant differences were found, there was a tendency for there to be less perceived pain in the MLC group, of the incision as well as in general. The next study by Bisgaard9 was undertaken using 3.5mm material, and in this study, unlike the previous one, the wounds of the trocars were preventatively infiltrated with Bupivacaine, leading to a significant reduction in the postoperative pain of the incision as well as an improvement in the aesthetic results.
The conclusion of the study that “smaller is not better”10 stated that the advantages of MLC were limited, and that MLC is only appropriate for young, thin patients, due to the fragility of the 3mm instrumentation,11 and that in comparison with MPLC the aesthetic result is better at one month after the operation, while ELA are recommenced earlier.12 It was considered to be a feasible alternative in selected patients, with less postoperative pain and better aesthetic results,13 although it should be considered a technically demanding procedure which has to be performed by teams with experience in laparoscopic surgery.14
The meta-analysis by McCloy15 published 6 years ago using 3mm material that was lower quality than is currently the case, indicates that conversion to MPLC is usually due to the fact that small calibre instrumentation is unable to provide appropriate traction and exposure of the gallbladder,8 as well as the problems associated with using a 3mm laparoscope.9 The systematic revision undertaken showed that MLC has some limited advantages over MPLC, although no definitive conclusions were drawn. In fact, the evidence for an improvement in postoperative pain was limited, so that it is therefore impossible to recommend this procedure based on this parameter, given that the affect on the pain of the incision and visceral pain were limited.1 Moreover, no other benefits during postoperative recovery were found, although satisfaction with the aesthetic result was higher.
Although the aesthetic result is an appreciable benefit of MLC, evaluating this is highly subjective16 and varies over the follow-up time. It may be irrelevant 6 months after surgery, as was published recently.17 And again, although the clinical benefit of an aesthetic improvement is clearly marginal, it may be psychologically important for some patients, such as young women.18,19
In many of the published studies the cases were very carefully selected, avoiding gallbladders with thickened walls and cases of obesity. The exceptions to this rule are Bisgaard's study and our series, although in our case the presence of a sclero-atrophic gallbladder was an exclusion criterion for the study.
One of the potential complications of CL is the development of hernia at the incision, generally in 10mm ports at an umbilical level. These are usually due to inadequate closure of the wound.20 One of the problems associated with SPLC is therefore its potentially higher incidence of hernia at the port incision, which in theory would be higher than it would be for patients treated using classical MPLC. 3mm and 5mm ports do not require closure, although the need for a 10mm access wound for the extraction of the gallbladder means that there must be at least one port or wound of that calibre. Moreover, gallbladders with chronic cholecystitis and those with large calculi cannot always be extracted through a 10mm port without lengthening the cutaneous or fascial incision, reinforcing the need for an abdominal wound at least 10mm long.
Thin instruments are more fragile, and this increases costs as they are less durable. This was supported in our study in connection with the 5mm optics and the cutting instruments which were of limited duration in use. Additionally, in patients with a thick adipose panicle dissection was hindered by the lack of rigidity of the instruments, even though they were inserted obliquely.
The introduction of SPLC has led to new comparative studies with MLC and MPLC. There is no clear evidence that SPLC reduces postoperative pain, and the data in the literature are contradictory. Although there is no doubt that the early aesthetic result is better in SPLC, this is no better than MLC in the overall aesthetic result, postoperative pain or the need for analgesics.21
When perceived pain, length of operation, technical difficulty, postoperative satisfaction and aesthetic result are analysed, comparing SPLC, MLC and MPLC, pain at 7 days is similar in all 3 procedures. The operation lasts longer in SPLC and MLC, while wound complications occur solely with SPLC. The aesthetic result at 6 months is better with MLC and SPLC, although there are no differences respecting those of MPLC at 12 months. Therefore, in terms of clinical efficacy over the medium term, neither SPLC nor MLC offer better results than MPLC.22
In general terms SPLC does not lead to differences in postoperative admission. Few studies cover ambulatory SPLC. Nor does it show any advantages in terms of recommencing ELA or returning to work, while it also has the most marked postoperative pain. However, there are no statistically significant differences in the analogical visual pain score or the use of analgesics, although there is a significant increase in costs.2
In the meta-analysis by Thakur,12 the beneficial aspects of MLC were reduction in postoperative pain and a better aesthetic result, although the majority of studies were not carried out in ITT, so that it is impossible to detect possible limitations of this technique due to the selection of patients. This meta-analysis showed similar rates of conversion for both procedures (MLC vs MPLC), with a lower rate of complications in MLC, better perceived aesthetics at one week and 30 days, an absence of differences in CVRS, faster commencement of ELA in MLC but with a longer operation time.
The meta-analysis by Li et al.23 analysed the results of 18 studies comparing SPLC with MPLC and 15 studies comparing MLC with MPLC. The conclusion was that MPLC would be the worst procedure in terms of postoperative pain, a longer postoperative stay and a lower aesthetic score. The best procedure would be MLC, due to its maximum aesthetic score, lower percentage of complications and less blood loss. SPLC could be an alternative because of its lower level of postoperative pain and shorter postoperative stay, although this would be at the cost of a higher rate of postoperative complications and greater loss of blood. In connection with the rate of complications, they occurred in 6.5% (0%–35.7%) for SPLC, 6.2% (0%–48.3%) for MPLC and 2.5% (0%–8.6%) for MLC. The highest aesthetic scores were for MLC, and the longest operation time was in SPLC.
The differences in hospital cost, adverse effects and the duration of the operation were analysed in the study by Chekan.24 The hospital cost was noticeably higher for SPLC, with a longer operating time and a far higher rate of adverse effects than MLC and MPLC. The hospital costs adjusted for ambulatory cholecystectomy were 18% higher between SPLC and MLC and 36% higher in comparison with MPLC. The lowest-cost procedure was MLC.
No study including MLC has been published in our country, although 2 studies were published on SPLC in connection with its potential for ambulatory surgery. The descriptive study by Martin Fernandez25 shows an average postoperative stay of 25.7h (9–72h) with admission lasting less than 24h for 76.9% of patients, although the study did not determine whether these were true ambulatory cases, as overnight stay data were not specified.
Nevertheless, the study by Fenollosa26 shows similar percentages of outpatient treatment for both procedures: 77% for SPLC and 83% for MPLC, with no significant differences in terms of postoperative pain between both procedures.
Although limited by sample size, our study shows that the rate of outpatient treatment with MLC remains in similar percentages to those for MPLC, which was our first aim in this analysis. It is better in terms of perceived pain and analgesic consumption in the immediate postoperative period for patients, although it has no influence on the recommencement of ELA. From a statistical point of view this difference is significant but of marginal value, given that it is not clinically relevant. Although we did not evaluate aesthetic repercussions, the subjective impression of the patients was highly positive.
However, the 3mm instrumentation still causes problems in connection with its capacity for traction and dissection. The need to use the Hasson umbilical port as a single pseudoport for shared access by the 5mm optics and the 5mm endoclip is even more problematic, given that they have to be parallel without triangulation for clamping structures, while they conflict for space. This is a long-term problem for the implementation of this technique.
To conclude, we believe that the MLC approach is feasible and safe. It makes it possible to achieve the same rate of outpatient treatment as MPLC and improves results in terms of perceived pain and analgesic consumption, while it has no relevant influence on the recommencement of ELA. Nevertheless, it should be restricted to carefully selected cases in which the aesthetic result is highly important for the patient, and to teams with long experience in CL. The question is whether aesthetic considerations can justify this procedure, when its clinical benefits are marginal and it increases costs.
Optimisation of the procedure would make it applicable without the need to select patients. This would probably involve using a mixed system of 2 3mm trocars (right empty, right hypochondrium) one 5mm trocar (left hypochondrium) with access through the Hasson trocar.
Conflict of InterestsThe authors have no conflict of interests to declare.
We would like to thank Karl Storz for the kind supply of minilaparoscopy material.
Please cite this article as: Planells Roig M, Arnal Bertomeu C, Garcia Espinosa R, Cervera Delgado M, Carrau Giner M. Colecistectomía laparoscópica ambulatoria por minilaparoscopia versus colecistectomía laparoscópica ambulatoria multipuerto tradicional. Estudio prospectivo aleatorizado. Cir Esp. 2016;94:86–92.