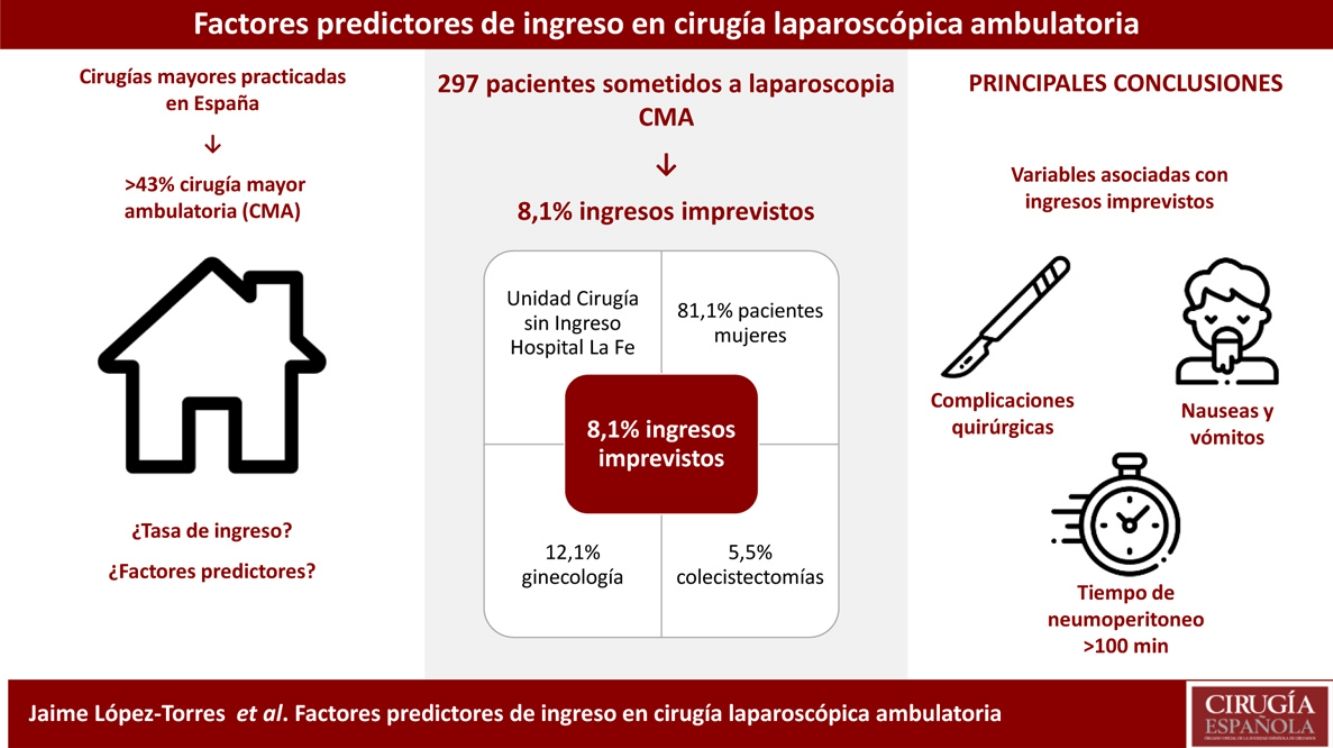
The aim of the study is to analyze the rate of unplanned hospitalization after ambulatory surgical procedures by laparoscopy, and identify associated risk factors to failure in the ambulatory manage of this patients.
MethodsA prospective observational study was performed during 18 months and included 297 patients treated with ambulatory laparoscopies performed at University Hospital La Fe of Valencia. The need for hospital admission, same day after surgery, was considered the main variable. Variables were recorded for preoperative, intraoperative or postoperative factors. To identify risk factors and variables associated with complications, statistical analyses were calculated with logistic regression models.
ResultsAfter laparoscopic surgery, 8.1% of patients required hospitalization. This rate was significantly superior in gynecologic surgery, patients with previous surgery complications, superior ASA score (II and III) and smokers. Likewise, patients with pneumoperitoneum time over 45minutes presented a higher hospitalization rate, also found in patients with anesthetic or surgery complications (including conversion to laparotomy). Finally, the rate of hospitalization was significantly superior in relation with postoperative nausea and vomiting (PONV).
ConclusionThe rate of patients who need hospitalization after ambulatory laparoscopic surgery was 8.1%, of which 5.5% were general surgeries and 12.1% were gynecologic surgeries. The most frequently related factors with failed ambulatory management, analyzed with multiple regression, were the appearance of surgery complications, pneumoperitoneum time over 100minutes and PONV.
El objetivo del estudio fue evaluar la tasa de ingreso no planificado tras cirugía laparoscópica ambulatoria e identificar factores relacionados con el fracaso de la ambulatorización en este tipo de pacientes.
MétodosEstudio observacional prospectivo de 297 pacientes adultos intervenidos mediante cirugía laparoscópica en régimen ambulatorio en el Hospital Universitari i Politècnic La Fe de Valencia durante 18 meses. Como variable principal se consideró la necesidad de ingreso hospitalario el mismo día de la intervención. Como variables independientes se registraron factores preoperatorios, intraoperatorios y postoperatorios. Mediante regresión múltiple se comprobó la asociación de ingreso postoperatorio con sus factores condicionantes, realizando un ajuste estadístico por las posibles variables de confusión.
ResultadosTras la cirugía laparoscópica el 8,1% de los pacientes precisó ingreso hospitalario. Esta proporción fue significativamente superior en las pacientes intervenidas de cirugía ginecológica, en los que habían presentado complicaciones en cirugías previas, en pacientes con un ASA superior y en fumadores, así como en quienes se prolongó el tiempo de neumoperitoneo por encima de 45minutos. También lo fue entre los pacientes que presentaron complicaciones anestésicas o quirúrgicas intraoperatorias. Por último, la proporción de pacientes ingresados fue significativamente superior cuando presentaron NVPO.
ConclusiónLa proporción de pacientes que ingresaron tras cirugía laparoscópica ambulatoria fue del 8,1%, correspondiendo al 5,5% de los sometidos a cirugía general y al 12,1% de las sometidas a cirugía ginecológica. Los factores más relacionados con el fracaso ambulatorio fueron la presencia de complicaciones quirúrgicas, el tiempo de neumoperitoneo superior a 100minutos y la aparición de náuseas postoperatorias.
Major outpatient surgery (MOS) contributes significantly to the sustainability of healthcare systems. In 2012, day surgery represented 43.4% of the major surgeries performed at hospitals of the Spanish National Healthcare System.1 Many laparoscopic procedures are performed on an outpatient basis and are listed as candidates for this treatment modality in the Manual of Major Ambulatory Surgery: Standards and Recommendations, guidelines published by the Spanish Ministry of Health and Consumption in 2008.2
Laparoscopy is associated with better perioperative results and has even been incorporated into enhanced recovery after surgery programs.3 Several studies confirm the relative safety of laparoscopic cholecystectomy (LC) as an outpatient procedure.4 However, shorter postoperative stay is associated with higher readmission rates.5 In gynecological surgery, the situation is similar.6,7 The main causes of prolonged postoperative stay and/or unexpected admission are usually due to pain, nausea, urinary retention, and observation of intraoperative complications.8
The objective of this study is to evaluate the rate of unplanned hospital admissions after outpatient laparoscopy and to try to identify factors related with failed outpatient management in these types of patients.
MethodsA prospective observational study was conducted in a cohort of adult patients who underwent laparoscopic surgery on an outpatient basis at the Hospital Universitari i Politècnic La Fe over a period of 18 months. The project received favorable reports from the hospital Scientific Committee and Ethics Committee for Biomedical Research. We selected 297 consecutive patients, with the following inclusion criteria: age >18 years and indication for outpatient laparoscopic surgery. We excluded patients for whom necessary information for the study could not be obtained, as well as those who refused to participate. A history of previous abdominal surgery was not a limiting factor.
The diagnoses (coded according to the International Classification of Diseases [ICD-9]) and the surgical indications were made by the general surgery and gynecology services. The patients were selected in the pre-anesthesia consultation, where informed consent was obtained. The rules of good clinical practice and the ethical principles of the Declaration of Helsinki were followed. Personal data were protected in accordance with the provisions of Organic Law 15/1999.
The study variables included: preoperative factors, such as anthropometric measures, comorbidities or anesthetic risk according to the American Society of Anesthesiologists (ASA); intraoperative factors, such as surgical time, intraoperative drugs, CO2 pressure, pneumoperitoneum time or complications; postoperative factors, such as complications or recovery times. The need for hospital admission on the same day of the intervention was the dependent variable.
During the intervention, all patients underwent basic monitoring, standard anesthetic induction and maintenance with intravenous or inhalational anesthetics. Intraoperative analgesia and antiemetic prophylaxis were used according to the criteria of the anesthesiologist.
After the procedure, the patients were awakened in the operating room and, depending on their clinical situation, transferred to the day surgery unit (DSU), to the post-anesthesia recovery unit, or to resuscitation. In the DSU, we recorded the appearance of postoperative nausea and vomiting (PONV), the degree of pain using a visual analog scale (VAS) ranging from 1–10 (1: absence of pain; 10: worst pain suffered) and the appearance of any other complication; this was done upon arrival and every 2hours. Discharge to home was considered when the patient achieved an evaluation greater than 8 points on the Aldrete scale, remained seated and began oral tolerance with liquids, remaining hemodynamically stable, conscious, had spontaneous urination, adequate ambulation, controlled pain and absence of PONV.
Statistical analysisThe information was entered into a database, refining and analyzing the data with the IBM SPSS Statistics program v.19. Initially, the characteristics of the subjects were described using frequency distribution and measures of central tendency and dispersion. In the bivariate analysis, comparison tests of means (Student’s t-test and ANOVA) and proportions (Chi-squared and Fisher’s exact test) were used. Using a logistic regression model, the association of the dichotomous dependent variable (postoperative admission), with its conditioning factors, were verified, using a statistical adjustment for possible confounding variables.
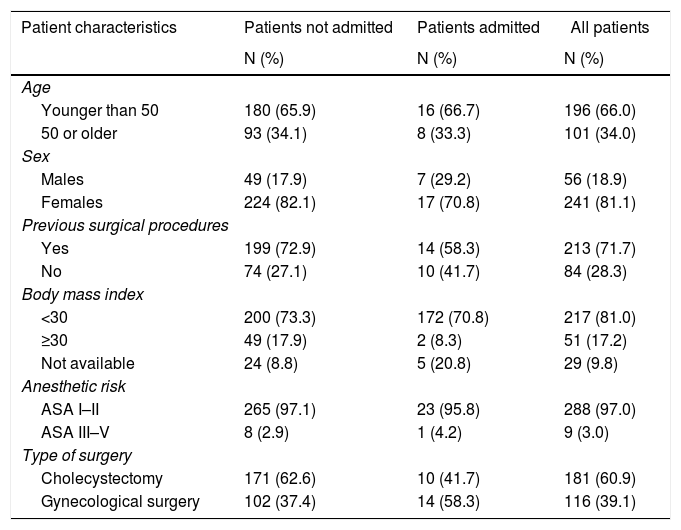
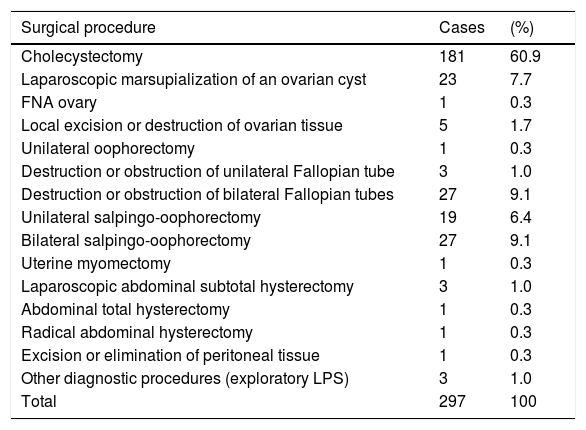
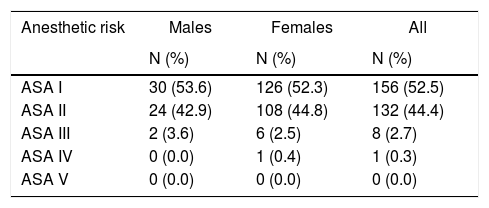
ResultsThe study included 297 patients whose mean age was 44.3±12 years, and the proportion of women was 81.1%. Table 1 shows the characteristics of the participants, and Table 2 shows the distribution of the cases studied according to the reason for surgery (ICD-9). Most of the patients (71.7%) had previously undergone surgical procedures, which was laparoscopic surgery in 12.1% of the cases. Table 3 shows the distribution of patients according to the ASA classification.
Patient characteristics.
| Patient characteristics | Patients not admitted | Patients admitted | All patients |
|---|---|---|---|
| N (%) | N (%) | N (%) | |
| Age | |||
| Younger than 50 | 180 (65.9) | 16 (66.7) | 196 (66.0) |
| 50 or older | 93 (34.1) | 8 (33.3) | 101 (34.0) |
| Sex | |||
| Males | 49 (17.9) | 7 (29.2) | 56 (18.9) |
| Females | 224 (82.1) | 17 (70.8) | 241 (81.1) |
| Previous surgical procedures | |||
| Yes | 199 (72.9) | 14 (58.3) | 213 (71.7) |
| No | 74 (27.1) | 10 (41.7) | 84 (28.3) |
| Body mass index | |||
| <30 | 200 (73.3) | 172 (70.8) | 217 (81.0) |
| ≥30 | 49 (17.9) | 2 (8.3) | 51 (17.2) |
| Not available | 24 (8.8) | 5 (20.8) | 29 (9.8) |
| Anesthetic risk | |||
| ASA I–II | 265 (97.1) | 23 (95.8) | 288 (97.0) |
| ASA III–V | 8 (2.9) | 1 (4.2) | 9 (3.0) |
| Type of surgery | |||
| Cholecystectomy | 171 (62.6) | 10 (41.7) | 181 (60.9) |
| Gynecological surgery | 102 (37.4) | 14 (58.3) | 116 (39.1) |
Distribution of cases studied according to the reason for surgery (CIE-9).
| Surgical procedure | Cases | (%) |
|---|---|---|
| Cholecystectomy | 181 | 60.9 |
| Laparoscopic marsupialization of an ovarian cyst | 23 | 7.7 |
| FNA ovary | 1 | 0.3 |
| Local excision or destruction of ovarian tissue | 5 | 1.7 |
| Unilateral oophorectomy | 1 | 0.3 |
| Destruction or obstruction of unilateral Fallopian tube | 3 | 1.0 |
| Destruction or obstruction of bilateral Fallopian tubes | 27 | 9.1 |
| Unilateral salpingo-oophorectomy | 19 | 6.4 |
| Bilateral salpingo-oophorectomy | 27 | 9.1 |
| Uterine myomectomy | 1 | 0.3 |
| Laparoscopic abdominal subtotal hysterectomy | 3 | 1.0 |
| Abdominal total hysterectomy | 1 | 0.3 |
| Radical abdominal hysterectomy | 1 | 0.3 |
| Excision or elimination of peritoneal tissue | 1 | 0.3 |
| Other diagnostic procedures (exploratory LPS) | 3 | 1.0 |
| Total | 297 | 100 |
Distribution of patients according to anesthetic risk (ASA classification).
| Anesthetic risk | Males | Females | All |
|---|---|---|---|
| N (%) | N (%) | N (%) | |
| ASA I | 30 (53.6) | 126 (52.3) | 156 (52.5) |
| ASA II | 24 (42.9) | 108 (44.8) | 132 (44.4) |
| ASA III | 2 (3.6) | 6 (2.5) | 8 (2.7) |
| ASA IV | 0 (0.0) | 1 (0.4) | 1 (0.3) |
| ASA V | 0 (0.0) | 0 (0.0) | 0 (0.0) |
To prevent postoperative pain, analgesics were used in 98.3% of the patients (mainly paracetamol, 75.6%), and NSAIDs were used in 84.9% (mainly dexketoprofen, 97.6%). Antiemetic drugs were used for PONV prophylaxis in 94.9%, especially ondansetron (4−8mg) plus dexamethasone (4−8mg) (66.2%). Other drugs were used in 64.5% of the cases, and the most widely used was pantoprazole (47.6%).
To establish of pneumoperitoneum, the most frequent number of trocars was 4 (95.3%), and the most frequently used method was Hasson’s (80.1%). The mean maximum pneumoperitoneum pressure was 14.9±1mmHg, and mean pressure was 11.7±1mmHg. The mean pneumoperitoneum time was 48.0±23minutes. Postoperative port infiltration with local anesthetics was performed in 77.0% of patients (0.2% ropivacaine in 91% of the cases). The mean duration of the procedures was 67.9±28minutes.
Anesthesia complications (bronchospasm, difficult intubation, allergic reaction) appeared in 3.0%, while surgical complications (surgery greater than expected, gallbladder perforation, bleeding) appeared in 11.1%, requiring conversion to laparotomy in 2 cases (0.7%) due to surgery that was greater than expected. Intraabdominal drain tubes were placed in 2.4% of patients (7 patients, 5 of which corresponded to gynecological surgery). After completing the intervention, 81.0% of the patients were admitted to the DSU and 19.0% to the post-anesthesia recovery unit.
During their stay in the DSU, 24.9% had nausea, 2.4% vomiting, 49.1% pain with intensity of ≥4 on a scale of 0–10, and 8.1% other complications (urinary retention, flatulence and hemodynamic abnormalities) The mean time elapsed from arrival at the DSU until discharge from said unit was 387.7minutes (SD: 170.0), and the median was 355.0. In the cases of general surgery, the mean was 409.4minutes (SD: 169.1), and in patients with gynecological surgery it was 350.4minutes (SD: 165.8).
After laparoscopic surgery, 8.1% of the patients required hospital admission (95% CI: 4.8–11.3). After discharge, the proportion of patients who required unforeseen medical assistance (emergency department) in the 7 days following discharge from the DSU was 9.4% (28 patients), and hospitalization was required in 3 cases for: pancreatitis, surgical site infection, and retinal detachment.
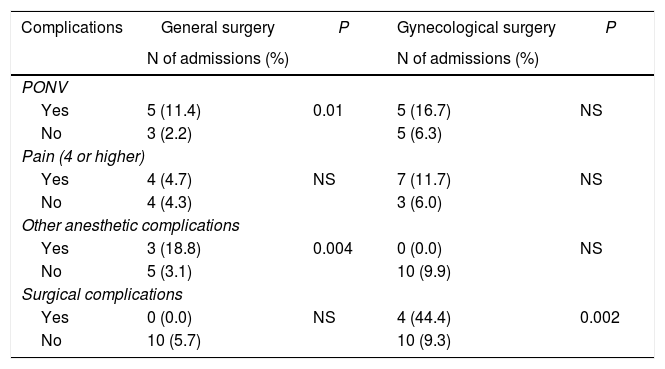
There were no differences in the rate of admissions in patients with different sex or age, however this proportion was significantly higher in gynecological patients compared to LC (12.1% vs. 5.5%; P=.04), in ASA II and III patients compared to ASA I patients (12.1% vs. 4.5%; P=.017), and in smokers versus non-smokers (13.9% vs. 6.2%; P=.03). Table 4 shows the proportion of patients admitted due to surgical and anesthetic complications according to the type of surgery.
Proportion of patients hospitalized, related to their surgical and anesthetic complications.
| Complications | General surgery | P | Gynecological surgery | P |
|---|---|---|---|---|
| N of admissions (%) | N of admissions (%) | |||
| PONV | ||||
| Yes | 5 (11.4) | 0.01 | 5 (16.7) | NS |
| No | 3 (2.2) | 5 (6.3) | ||
| Pain (4 or higher) | ||||
| Yes | 4 (4.7) | NS | 7 (11.7) | NS |
| No | 4 (4.3) | 3 (6.0) | ||
| Other anesthetic complications | ||||
| Yes | 3 (18.8) | 0.004 | 0 (0.0) | NS |
| No | 5 (3.1) | 10 (9.9) | ||
| Surgical complications | ||||
| Yes | 0 (0.0) | NS | 4 (44.4) | 0.002 |
| No | 10 (5.7) | 10 (9.3) | ||
NS: difference is not significant.
There were more admissions among the patients with prolonged pneumoperitoneum time. The difference was statistically significant when it was greater than 45minutes (11.7% vs. 4.7%; P=.02) and very significant when it was greater than 100 minutes (55.6% vs. 5.7%; P<.001). The proportion of admissions was not related to the maximum or mean pneumoperitoneum pressure values. The total time of the procedure was higher among patients who were admitted compared to those who were not (85.3minutes±62.7 SD vs. 66.5minutes±23.6 SD; P=.003).
The proportion of admissions was also significantly higher in the event of anesthetic complications (44.4% vs. 7.0%; P=.003) or surgical complications (36.4% vs 4.6%; P<.001) or due to the need for conversion to laparotomy (100% vs. 7.5%; P=.006). Lastly, the proportion of admitted patients was significantly higher when the patients presented postoperative nausea (13.5% vs. 3.7%; P=.003) or vomiting (42.9% vs. 5.3%; P=.006). In contrast, the percentage of hospitalized patients was not related to the presence of pain or other postoperative complications or to hemodynamic variables.
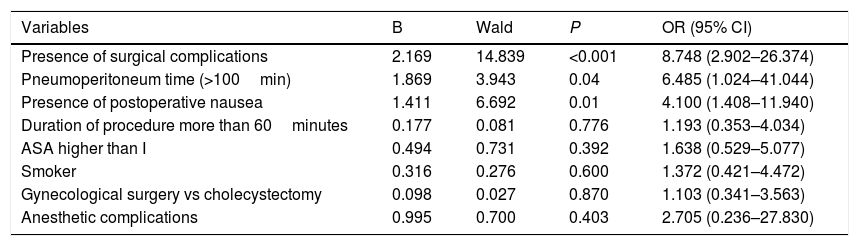
The variables that were associated by logistic regression with the need for hospital admission are shown in Table 5.
Variables introduced in the logistic regression model whose variable was the need for hospital admission.
| Variables | B | Wald | P | OR (95% CI) |
|---|---|---|---|---|
| Presence of surgical complications | 2.169 | 14.839 | <0.001 | 8.748 (2.902–26.374) |
| Pneumoperitoneum time (>100min) | 1.869 | 3.943 | 0.04 | 6.485 (1.024–41.044) |
| Presence of postoperative nausea | 1.411 | 6.692 | 0.01 | 4.100 (1.408–11.940) |
| Duration of procedure more than 60minutes | 0.177 | 0.081 | 0.776 | 1.193 (0.353–4.034) |
| ASA higher than I | 0.494 | 0.731 | 0.392 | 1.638 (0.529–5.077) |
| Smoker | 0.316 | 0.276 | 0.600 | 1.372 (0.421–4.472) |
| Gynecological surgery vs cholecystectomy | 0.098 | 0.027 | 0.870 | 1.103 (0.341–3.563) |
| Anesthetic complications | 0.995 | 0.700 | 0.403 | 2.705 (0.236–27.830) |
After laparoscopic surgery, 8.1% of the patients required hospital admission. This rate was significantly higher in patients who underwent gynecological surgery, in those who had presented complications in previous surgeries, in patients with higher ASA, and in smokers. Likewise, patients with a pneumoperitoneum time greater than 45minutes had a higher rate of unexpected hospital admission, with the total duration of the procedures being higher among those who required admission. The percentage of admissions was also higher among patients with anesthesia or surgical complications. Finally, hospitalization was significantly higher among patients who presented PONV.
The unplanned hospitalization rate is one of the most commonly used factors to analyze day surgery results. It is an indicator that detects problems such as poor patient selection or inappropriate complexity of a procedure. In our patient series, the rate was 8.1%, which is within the range reported in the literature (0.09%–16%),9 and it was significantly higher in gynecological patients.
A recent meta-analysis of 13 clinical trials evaluating the outcome of ambulatory LC described an unplanned admission rate of 13.1% (0%–35%).10 Regarding gynecological surgery, the unplanned admission rate varies depending on the type of intervention. In a 2012 study of 128634 patients who underwent laparoscopic hysterectomy, the unexpected admission rate was 4.0%.11 The study by Maheux-Lacroix et al. describes the percentage of ambulatory laparoscopic total hysterectomy of 62%.5 For adnexal disease (diagnosis or for treatment of infertility), Houllier et al. reported an unexpected admission rate of 37%.12
The history of previous laparoscopic surgery is associated with a higher rate of unplanned admission in our patient series. The presence of procedures in the abdominal cavity favors the development of adhesions and fibrosis, making the surgical technique difficult and decreasing abdominal compliance.13 For years, a history of previous abdominal surgery has not been considered a contraindication in laparoscopic surgery, although it may affect the results. In a publication on 1,638 laparoscopies, the existence of previous abdominal surgery was associated with a greater need for adhesiolysis, higher conversion rate, prolonged intervention time and a longer postoperative stay.14 This antecedent may prolong the intraoperative time, worsening postoperative symptoms, lengthening recovery time and, finally, increasing the risk of admission.
A prolonged pneumoperitoneum time could also be related with worse results.15 The use of high inflation pressures significantly affects cardiopulmonary function.16,17 Furthermore, the absorption of CO2 causes respiratory and hemodynamic problems during the intraoperative period.18 These are well-tolerated phenomena in healthy and/or ambulatory patients, but they can affect the immediate postoperative period, increasing the risk of unforeseen admission. In our results, a prolonged pneumoperitoneum time (greater than 100minutes) is significantly associated with a higher rate of unexpected admission.
The presence of intraoperative complications in abdominal laparoscopic surgery is rare. The intraoperative events in our series, related to anesthesia (3%) or surgery (11.1%), are similar to previous studies.19,20 In our series, the presence of anesthetic and/or surgical complications multiplied the probability of admission 6 and 9 times, respectively. There is still uncertainty about the frequency of complications in MOS. The study by Johnston et al. analyzed 1265 laparoscopic gynecological procedures: hysterectomy, pelvic floor repair, endometriosis surgery, adnexal surgery and adhesiolysis. Major complications related to intestinal, urological or large vessel injuries were rare (0.6%).19
In the case of LC, major complications are also rare21 and include bleeding (0.11%–1.97%), abscess (0.14%–0.30%), bile leakage (0.30%–0.90%), intestinal injury (0.14%–0.35%)22 and bile duct injury (0.26%–0.60%), which was the most frequent serious complication.23
PONV has been the most common reason for unexpected admission in MOS, accounting for some 50% of cases.24,25 Almost one-third of our patients required antiemetic treatment at DSU, although only 2 patients were admitted for PONV refractory to treatment. The factors associated with PONV were female sex, absence of prophylaxis, and long preoperative waiting time.
The limitations of this study include the lack of information for certain variables, which is attributable to the great variety of professionals involved. When interpreting the results, one must keep in mind that the procedures were performed by different units in the case of gynecological procedures, and that the comparison of the procedures performed by the general surgery team (liver unit) versus those performed by gynecology teams (infertility, endometriosis, oncology units) may have contributed to obtaining different results in terms of the rate of admissions. In addition, the predominance of the female sex in the sample must be considered, as symptomatic cholelithiasis is much more frequent in women and diseases of the female sex have been included in the study.
Other limitations could be indicated because it is an observational study, such as the lack of protocolization within the study for certain procedures (antiemetic or analgesic medication, placement of a nasogastric tube, recruitment maneuvers after pneumoperitoneum, etc.).
Lastly, bladder perforation and significant intraoperative bleeding were considered complications. Both processes can be found in the literature interpreted as both complications and intraoperative incidents.
More research is needed to identify interventions that help reduce the failure rate in outpatient management of laparoscopic surgery.
The proportion of patients admitted after outpatient laparoscopic surgery is only 8.1% (5.5% general surgery and 12.1% gynecological surgery). Factors related with failed ambulatory treatment included the presence of surgical complications, prolonged pneumoperitoneum time (more than 100minutes) and the appearance of postoperative nausea.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: López-Torres López J, Cifuentes García B, Fernández Ruipérez L, Rodeles Criado A, Alcántara Noalles MJ, Peiró García R, et al. Factores con valor predictivo de ingreso en cirugía laparoscópica ambulatoria. Cir Esp. 2021;99:140–146.