Patients who have undergone bariatric surgery and later present diseases of the hepatobiliary area are difficult to diagnose and treat due to their anatomical and pathophysiological alterations.
We present the case of a 57-year-old woman who underwent laparoscopic Roux-en-Y gastric bypass (RYGB) for morbid obesity 12 years ago, with a 150cm Roux limb and a 60cm biliopancreatic limb (BPL). Her BMI at that time was 31.95kg/m2. She came to the emergency room due to pruritus that had progressed for a week. On physical examination, she presented a non-painful palpable gallbladder, suggestive of the Courvoisier-Terrier sign. Lab work showed predominantly direct hyperbilirubinemia (total bilirubin 6.83mg/dL and direct bilirubin 4.91mg/dL), elevated cholestasis enzymes and Ca 19.9 tumor marker 117.6U/mL.
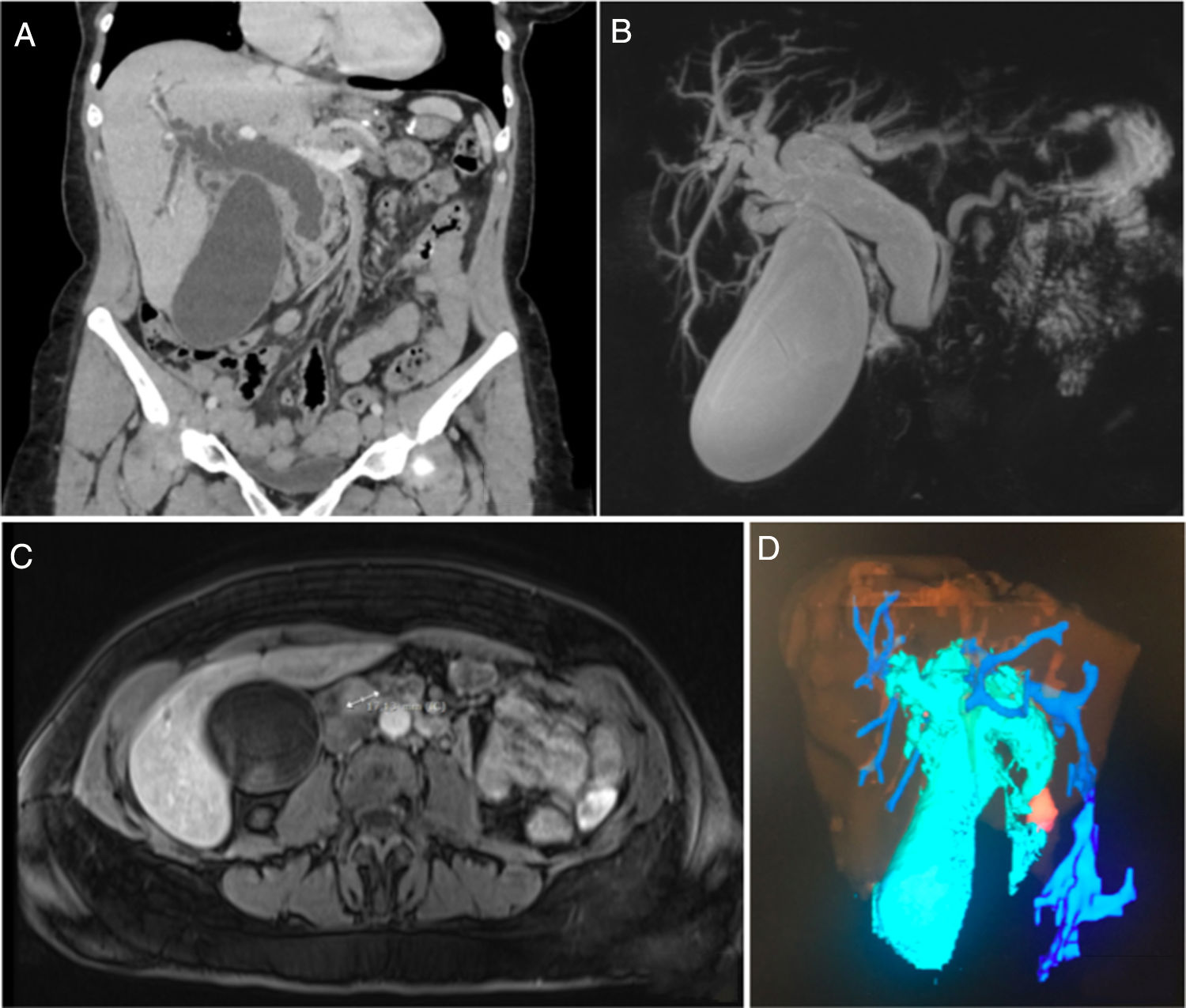
Abdominal computed tomography (CT) scan (Fig. 1a) revealed a hydropic gallbladder and dilation of the intrahepatic bile duct and common bile duct (23mm), with a sudden change in caliber at the papilla of Vater, with homogeneous increase in soft tissue.
(a) Abdominal CT with intravenous contrast (coronal plane reconstruction). Hydropic gallbladder and dilation of the intrahepatic bile duct and common bile duct (23mm), with a sudden change in caliber at the level of the papilla of Vater; (b and c) MRCP showing a markedly dilated bile duct with an abrupt change in caliber in the distal-prepapillary common bile duct, coinciding with the presence of a nodular lesion measuring 17mm that was enhanced after the administration of contrast that could correspond with ampullary cancer (b: coronal MIP reconstruction and c: axial T1-FS image with iv contrast in arterial phase); (d) reconstruction using Myrian® software from Intrasense® showing the enlarged gallbladder and dilated bile duct in light blue and the ampullary lesion in orange.
Magnetic resonance cholangiopancreatography (MRCP) (Fig. 1b) revealed a markedly dilated bile duct with an abrupt change in caliber in the distal/pre-papillary common bile duct, coinciding with the presence of a nodular lesion measuring 17mm that was isointense on T1 and T2-weighted sequences, showing restriction in diffusion sequences, and which was slightly enhanced after the administration of intravenous contrast (Fig. 1c and d), as well as a lymphadenopathy in the bifurcation of the celiac trunk. The differential diagnosis included ampullary carcinoma, impacted lithiasis, biliary cast, pancreatic head cancer, or papillitis.
The case was discussed in the multidisciplinary committee, at which time we decided to drain the bile duct by means of percutaneous transhepatic cholangiography (PTHC), and biopsies were taken. The PTHC detected a large dilation of the intra- and extrahepatic bile duct with obstruction at the papilla; past the obstruction, an 8 F internal–external biliary drain tube was placed, and the bile discharge was clean. A biopsy was taken, which was not conclusive as the sample consisted of fibromuscular tissue and glands without cytoarchitectural atypia.
The patient evolved favorably, with improved pruritus and jaundice, as well as lower bilirubin levels on follow-up studies. We decided to try double-balloon enteroscopy for another biopsy, but this was unsuccessful given the inability to reach the papilla endoscopically as a consequence of the previous of RYGB.
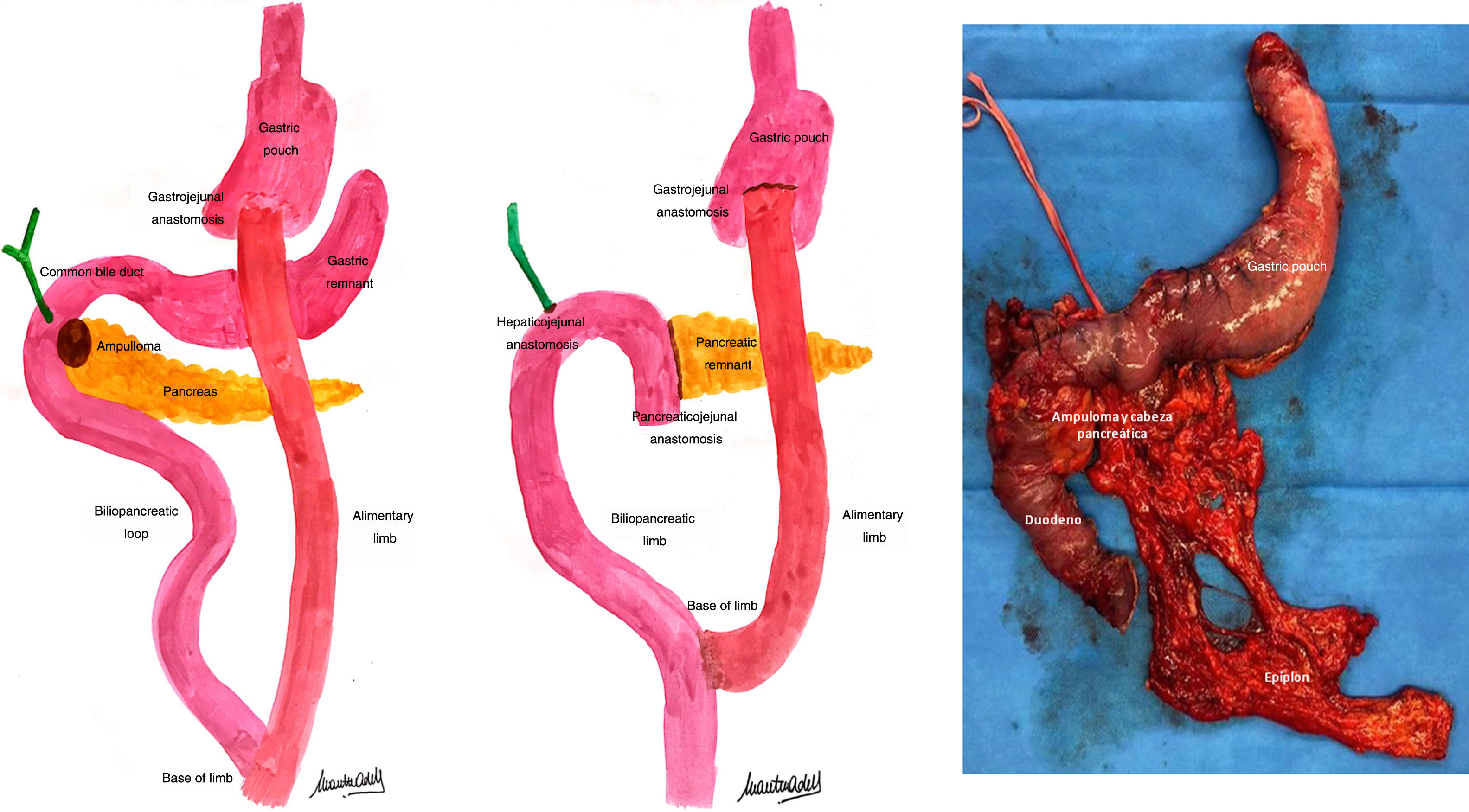
As it was impossible to rule out the presence of neoplasia, and we had performed all the preoperative tests available at our hospital, pancreaticoduodenectomy (PD) was proposed to the patient. Thus, PD was performed with an end-to-side duct-to-mucosa pancreaticojejunal anastomosis following the Blumgart technique and an end-to-side hepaticojejunal anastomosis (using the distal segment of the old biliopancreatic limb from the RYGB in both cases) as well as gastrectomy of the gastric remnant (Fig. 2). During the postoperative period, the patient presented infection of the surgical wound, which required drainage and antibiotic therapy; she was discharged on the 12th postoperative day. The pathological study reported an infiltrating intestinal-type adenocarcinoma of ampullary-ductal origin (G2 pT3bN0). Currently under treatment with capecitabine, the patient has had no evidence of disease 3 months after surgery.
Patients with a history of RYGB pose great difficulty in diagnosing biliopancreatic diseases. The presence of disease in the biliary limb may manifest abnormally because the intestinal tract has been modified. Moreover, the diagnosis of periampullary disease is also made difficult by the biliary limb,1 since it is necessary to initially reach the base of the loop during endoscopy, and later ascend through the biliopancreatic limb to the papilla, with the associated difficulties of the length and angles of the intestinal tract involved.
In our case, double-balloon ERCP was attempted, but the papilla could not be reached endoscopically. There are other diagnostic possibilities2 to consider, such as ERCP assisted by laparoscopy, transgastric or transjejunal, pediatric colonoscopes, fluoroscopy-guided percutaneous gastrostomy or endoscopic ultrasound-guided gastrogastrostomy.3 Furthermore, when considering surgical options, it is important to take into account the difficulty posed by the post-RYGB anatomy for the resection and reconstruction performed during PD. There are several technical options,4 but the evidence is limited, and there is no clear consensus. In our case, we opted to use the old BPL for the reconstruction of pancreatic and biliary drainage, which is a recommended technique5 if the length of the BPL is sufficient, since it avoids intestinal resections that would increase the possibility of postoperative malabsorption. The gastrectomy of the remnant avoids4 the need for additional anastomoses, with their possible associated complications, as well as the future appearance of gastric disease, both benign and malignant. In this case, initial ampullectomy was not considered because the lesion occupied the common bile duct, contraindicating this approach.
Due to their altered anatomy, patients who have previously undergone RYGB present significant difficulties both in the diagnosis and in the treatment of diseases of the hepatobiliary area. However, there are presently several minimally invasive diagnostic techniques that should be explored before subjecting these patients to a surgical procedure with high morbidity without a definitive diagnosis for a disease that could ultimately be benign.
FundingThis study has received no specific funding from public, private or non-profit organizations.
Please cite this article as: Curell A, Adell M, Gómez-Gavara C, Pando E, Merino X. Ampuloma en paciente con antecedente de bypass gastroyeyunal en Y de Roux. Cir Esp. 2020;98:634–636.