Fibroadenomas are the most frequent benign tumors of the breast. They are a benign proliferation of the mesenchymal and epithelial component of the breast that are variable in size, although usually smaller than 2cm. In general, these tumors are mobile and well defined, cause no pain and preferentially develop in young women between the second and third decades of life. On rare occasions, fibroadenomas are associated with the development of carcinomas, which generally appear in the fifth decade of life, some 20 years after the peak incidence of simple fibroadenomas. We present the case of invasive ductal carcinoma in the context of a breast fibroadenoma that was diagnosed after having presenting axillary lymph node metastasis.
The patient is a 48-year-old premenopausal woman with no prior pregnancies who had been monitored for the previous 10 years due to a fibroadenoma of the right breast. On the latest mammogram, changes were observed in the image of the fibroadenoma compared with previous studies; suspected malignant axillary lymphadenopathies were also detected. Specifically, at the junction between the upper quadrants of the right breast, mammography demonstrated a dense nodular mass that was partially defined and had coarse calcifications as well as more nonspecific pinpoint interior calcifications, with a suspected diagnosis of fibroadenoma (BI-RADS 0). Nonetheless, as there were atypical changes compared with previous mammograms, ultrasound study and biopsy of the lesion were ordered.
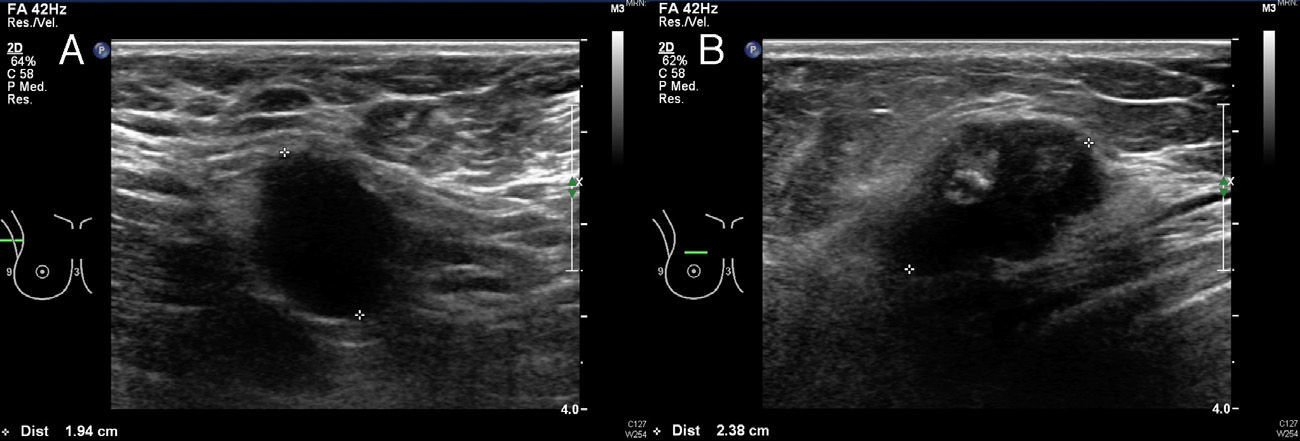
Ultrasound detected an irregular, poorly defined nodule measuring 2.6cm×1.6cm at the junction of the upper right breast quadrant, category BI-RADS IV, and 2 lymphadenopathies measuring 19 and 10mm in the right axillary prolongation, with loss of fatty hilum and an malignant appearance (Fig. 1). The study was completed with ultrasound-guided core needle biopsy of the nodule and fine needle aspiration (FNA) of an axillary lymphadenopathy. The histology results reported tissue with characteristics of fibroadenoma, but the ducts were covered by several layers of atypical cells that were suspicious of ductal carcinoma. FNA of the axillary lymphadenopathy confirmed metastatic carcinoma.
The extension study was negative. Tumorectomy was performed at the junction of the upper quadrants of the right breast using round-block mammoplasty with standard right axillary lymphadenectomy. Intraoperative study of the surgical specimens demonstrated fibroadenoma with in situ and infiltrating carcinoma and tumor-free margins.
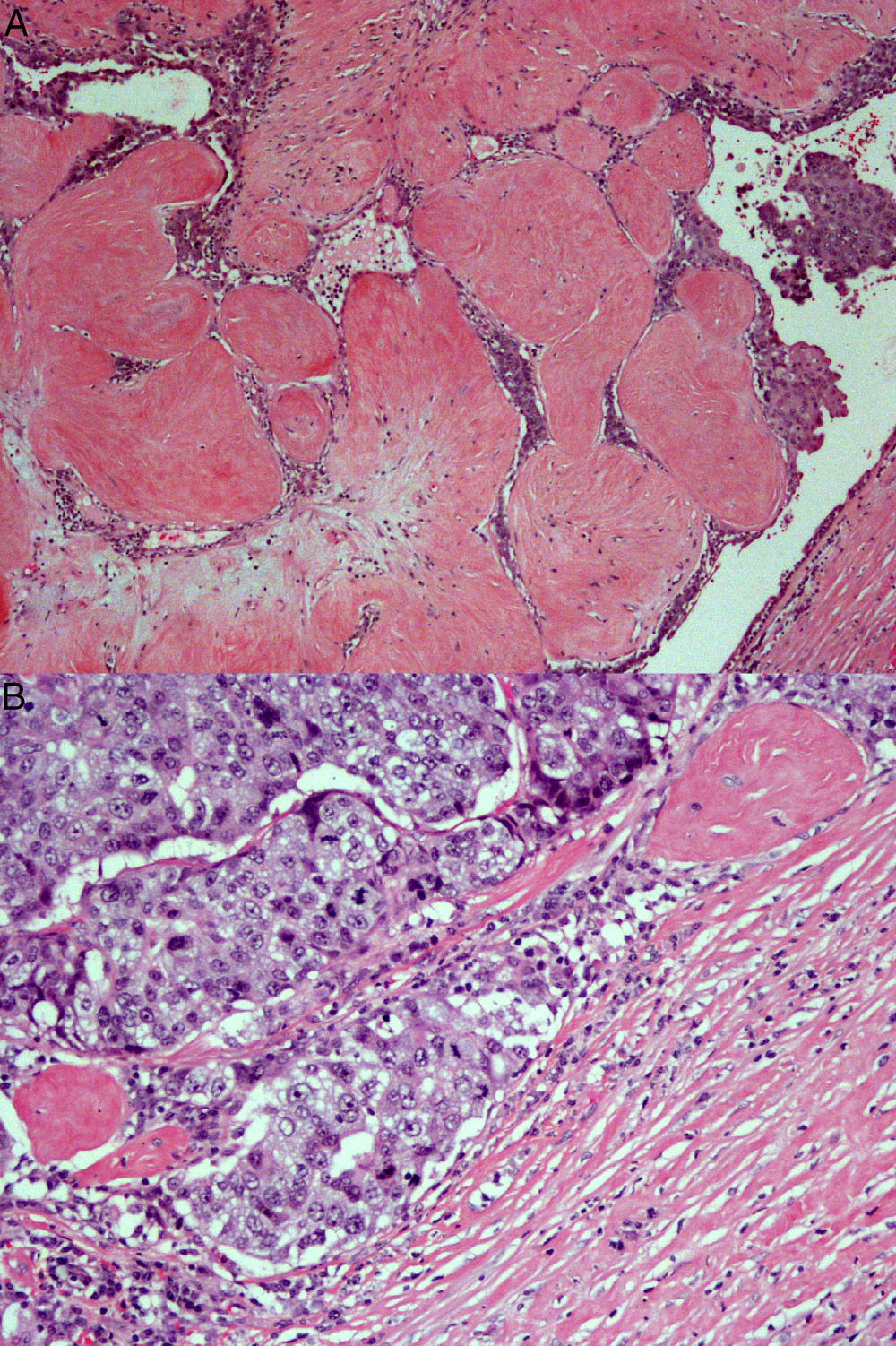
The definitive histopathology study was of poorly differentiated invasive ductal carcinoma at 2 invasive foci (the larger measuring 0.7cm×0.5cm) over an extensive high nuclear grade ductal carcinoma with necrosis. Both the infiltrating and ductal lesions focally affected the surrounding breast tissue and were situated within a fibroadenoma (Fig. 2). The surgical margins were free. There was vascular invasion and 2 lymph nodes out of the 18 that had been resected presented with metastasis, with no evidence of capsular rupture (pT1b pN1a). Immunohistochemistry showed: RE +++, RPg +++, Ki67 20%, HER-2 negative. We decided to complete treatment with polychemotherapy, radiotherapy and hormone therapy.
The progression of the epithelial component to in situ and invasive carcinoma has been described in the literature; it is usually an incidental finding after the resection of the fibroadenoma.1–4 The first to report a carcinoma in the context of a fibroadenoma were Cheatle and Cutler in 1931,5 and to date some 200 cases have been reported.
The incidence of carcinoma within a fibroadenoma is 0.1%–0.3%, with a peak incidence between the ages of 42 to 44.3,6–8 Most carcinomas that arise from a fibroadenoma are in situ neoplasms, and the lobular type is the most frequent.7 Cases of invasive ductal carcinoma, as in our patient, are extremely rare.7,8 It is therefore exceptional to find a case similar to ours, in which we highlight the clinical manifestation with axillary involvement.
Complex fibroadenomas and the proliferative diseases adjacent to fibroadenomas are associated with a mild increase in the risk for breast cancer.7 In spite of the low incidence of carcinomas in the interior of fibroadenomas, surgeons should keep this rare clinical entity in mind during the follow-up of women over the age of 35 who present atypical changes in solid, well-defined breast tumors. Clinical and radiological criteria should help us identify possible malignization, and, consequently, biopsies should be taken.9 From a clinical standpoint, suspicious signs for fibroadenoma malignization include increased size on physical examination, the presence of imprecise edges and attachment to surrounding tissue. Furthermore, radiological signs that merit further attention are growth, irregular shape and the presence of grouped microcalcifications.6,10
With regard to treatment, the number of cases reported in the literature is not sufficient to make conclusions about therapeutic decisions. As an exceptional circumstance, other carcinomas have been reported in association with the primary tumor, which have been either adjacent or in the contralateral breast.6 Thus, detailed studies of both breasts are recommended to avoid other lesions going unnoticed during surgery, and treatment (tumorectomy or more extensive surgery) should be designed according to the results of preoperative studies. The biological behavior of carcinomas that arise from a fibroadenoma is the same as that of a breast carcinoma that is unrelated with the fibroadenoma; therefore, the recommendation is to follow the general principles of in situ or invasive breast cancer.
Please cite this article as: Arencibia Pérez B, Vega Benítez V, Hernández Hernández JR, Alfonso Martín JL, López-Tomassetti Fernández E. Adenopatía axilar como debut de un carcinoma en el seno de un fibroadenoma. Cir Esp. 2015;93:e77–e79.