Approximately 70%–75% of traumatic haemothorax can be managed with chest tubes.1 Only 15% of blunt trauma injuries require emergency surgery.2
The estimated incidence of diaphragm injury is 5% in patients who are hospitalised with blunt thoracoabdominal trauma, and some 50% of these cases go unnoticed during the initial examination at admittance. Up to 8% of patients who undergo urgent thoracotomy after blunt trauma present a diaphragm lesion that had initially gone undetected.3
Almost all cases diagnosed in the acute phase are associated with one or several organ lesions that are life-threatening. Rapid assessment of the patient's clinical situation is necessary, along with meticulous observation of chest radiographs. This is especially true in the case of penetrating wounds in blunt chest trauma, as in the case we present.
Case ReportA 50-year-old male was treated in the Emergency Department due to thoracic pain and dyspnoea after thoracoabdominal trauma that occurred when getting out of the bathtub. The patient reported no cranial trauma or injuries to other areas. Prior to the accident, the patient had been healthy and had no medical history of interest. He smoked 2 packs/day and had no other toxic habits.
At admittance, the patient was conscious and oriented (Glasgow 15); blood pressure (BP) was 114/68mmHg, heart rate 98bpm, baseline SO2 95 and glycemia 112mg/dL.
Physical examination showed a permeable airway and sharp pain in the ribs during inspiration, with crepitation of the left ribcage and no observed flail chest. Cardiorespiratory auscultation was normal with audible vesicular murmur.
Lab work showed: haemoglobin (Hb) 170g/L and 17.84×109leukocytes/L. On chest radiography, unipolar fractures were observed in the left ribs (5th–9th) with no consolidations, collections or signs of pneumothorax. Thoracoabdominal CT scan with intravenous contrast confirmed these rib fractures and that the 5th, 6th and 7th were displaced. Mild oedema and emphysema of the wall were observed with minimal left pleural effusion. There were no images of pneumothorax, signs of laceration or important foci of pulmonary contusion. There were also no abdominal findings of interest.
The patient was hospitalised for further monitoring and analgesia. After 72h, the patient started to sit up. There was a fall of 25g/L in Hb compared to the levels at admittance. The patient had episodes of severe hypotension and bradycardia of up to 45lpm, which initially responded to fluids and Trendelenburg position. Auscultation showed abolition of the vesicular murmur in the lower two-thirds of the left hemithorax. Chest radiograph showed evidence of moderate-severe pleural effusion (Fig. 1). A chest drain tube was placed in the 5th intercostal space on the anterior axillary midline according to the standard technique, and 1700cc of blood were immediately collected. Simultaneously, the patient had another hypotensive episode, which he overcame with fluid therapy. Another chest radiograph verified the correct placement of the chest drain but no lung re-expansion. Blood work showed Hb 70g/L, which was a drop of 100g/L since hospitalisation. Given these findings and the haemodynamic instability of the patient, urgent exploratory thoracotomy was indicated when the drained content had already reached 2100cc.
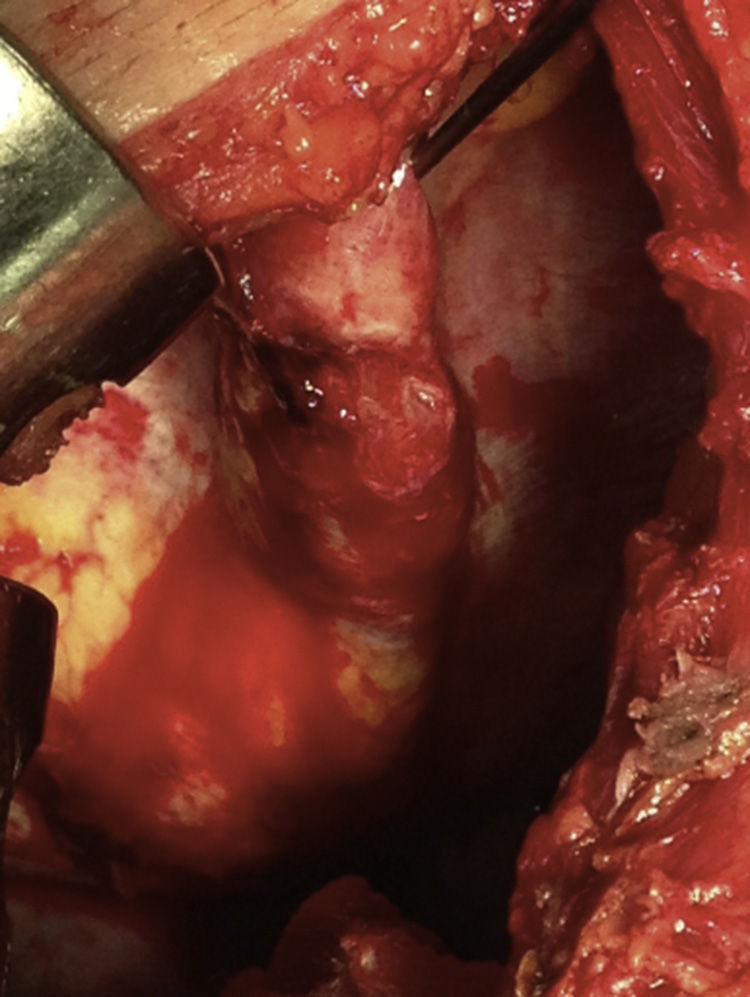
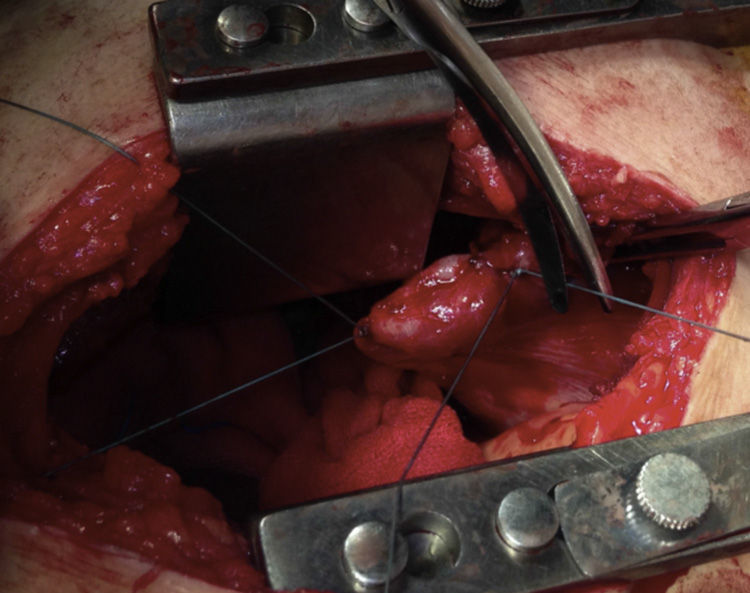
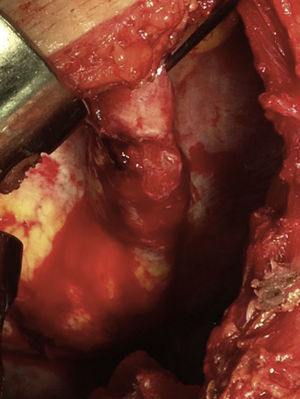
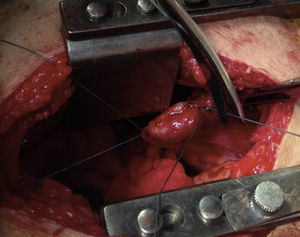
Lateral thoracotomy was performed in the 5th intercostal space, and a massive haemothorax was evacuated (1500cc) with abundant lavage. We confirmed displaced fractures of the 5th to 7th ribs. The 7th had splintered edges, with one of the edges aimed towards the diaphragm and laceration of its corresponding dome measuring 4cm, which was bleeding profusely (Fig. 2). Haemostasis was achieved by means of a diaphragm transfixion suture and continuous suture of the tear with PremiCron® 0 (Fig. 3), followed by abundant lavage. We inspected the lung and found no injury. The rib edges were trimmed and smoothed. Chest wall closure was performed with the insertion of 2 chest drains.
The patient remained stable during surgery and required 1500cc crystalloids and the transfusion of 3 units of blood.
The patient stayed in the ICU for 24h, where he was haemodynamically stable. On the hospital ward, his condition continued to improve and the patient was discharged on the 4th day after surgery with normalised parameters. At the follow-up visit 1 month later, no complications were observed.
DiscussionMassive haemothorax involves the sudden accumulation of more than 1500cc of blood or one-third the patient's blood volume in the thoracic cavity.4 This condition, although more frequent in open trauma, can go unnoticed in blunt trauma and therefore requires a high index of suspicion.
Massive haemothorax also involves comprised respiratory function due to the deficient lung expansion that impedes adequate ventilation and hypoxaemia. This situation, together with the accompanying hypovolemic shock, is life-threatening.
During the examination of multiple trauma patients, haemodynamic instability associated with hypovolemic shock, accompanied by absence of vesicular murmur and dullness to percussion in the hemithorax, are diagnostic of massive haemothorax (all of which were present in this case).4 Chest radiography can confirm the initial diagnosis and provides early assessment of the correct placement of the chest tube as well as lung re-expansion once the haemothorax is drained. Measurement of Hb enables us to easily determine the estimated blood loss and it is a fundamental parameter that contributes to better blood volume replacement with transfusion of blood products, if necessary. The use of CT scans in massive haemothorax is excluded because of the patient instability with this condition.
Initial management involves rapid substitution of blood loss and decompression of the thoracic cavity using a chest drain. Drainage of more than 1500cc of blood or 200mL/h in 2–4h are criteria for urgent thoracotomy.4 In the case we report, there was an immediate evacuation of 1700cc after chest tube insertion, the imaging study confirmed the lack of lung re-expansion, and the haemodynamic instability of the patient all indicated emergency exploratory thoracotomy.
The selection of the surgical approach is essential in this situation and is defined by the initial suspicion of the injury and the understanding of the exposure offered by the incision.5 In our case, we theorised that the source of the haemorrhage could be the diaphragm lesion or the displaced rib fractures.
The approach we chose was lateral thoracotomy in the 5th intercostal space, which provided good visualisation of the diaphragm surface and rib fractures in order to control any bleeding and for stabilisation. It also enabled us to explore the entire chest cavity, parenchyma and hilum in order to rule out any concomitant injuries.
Cases of massive, late-onset and sudden haemothorax described in the literature are always associated with displaced lower rib fractures. The injury mechanism in diaphragm laceration caused by the stabbing action of a displaced rib has been described as a “penetrating injury in blunt trauma”.6 During blunt trauma, the increased intraabdominal pressure forces the diaphragm upwards, where it comes into contact with the fractured rib edge, which cuts the diaphragm like a knife. In the case we report, sitting up and moving led to increased intraabdominal pressure and an approximation of the diaphragm dome to the bone fracture, causing this “penetrating injury in the context of blunt trauma”.
We conclude that, in patients with multiple trauma injuries and displaced lower rib fractures,7 undetected diaphragm injuries can result in massive haemothorax, especially when the patient starts to move and the pain is disguised by the fractured rib pain.
It is essential to always monitor early signs of hypovolemic shock and maintain a high index of suspicion. The chest should be studied in detail, as the pain from the rib trauma can camouflage injury to the diaphragm. When faced with a situation of haemodynamic instability associated with compatible examination, drastic drop in Hb in a discharge of more than an initial 1500c or more than 200cc/h in 2–4h, urgent thoracotomy is indicated and should not be delayed.4,8
Please cite this article as: Segura Sampedro JJ, García Gómez F, Arroyo Pareja L, Pardo Prieto SL, Moreno Mata N. Hemotórax masivo tardío por laceración diafragmática asociado a fracturas costales inferiores. Una herida penetrante en el traumatismo cerrado. Cir Esp. 2015;93:e73–e75.