Median arcuate ligament syndrome is caused by compression at the origin of the celiac trunk by the arcuate ligament, a fibrous band that joins the 2 crura of the diaphragm. Although the stenosis is usually asymptomatic, when it interrupts the pancreaticoduodenal arterial arcades (as in pancreaticoduodenectomy), it may lead to visceral ischaemia.
We present the case of a 74-year-old man who was admitted for further study of epigastric pain, general malaise and jaundice. Work-up showed a total Br of 5.50 and GPT of 615. Abdominal ultrasound reported dilatation of the intrahepatic bile duct and the common bile duct of 15mm, with no observable cause.
CT demonstrated a mass in the uncinate process of the pancreas, which caused an important dilatation of the bile duct and main pancreatic duct. Results of endoscopic ultrasound-guided FNA were compatible with adenocarcinoma, and it was necessary to insert a plastic stent by ERCP.
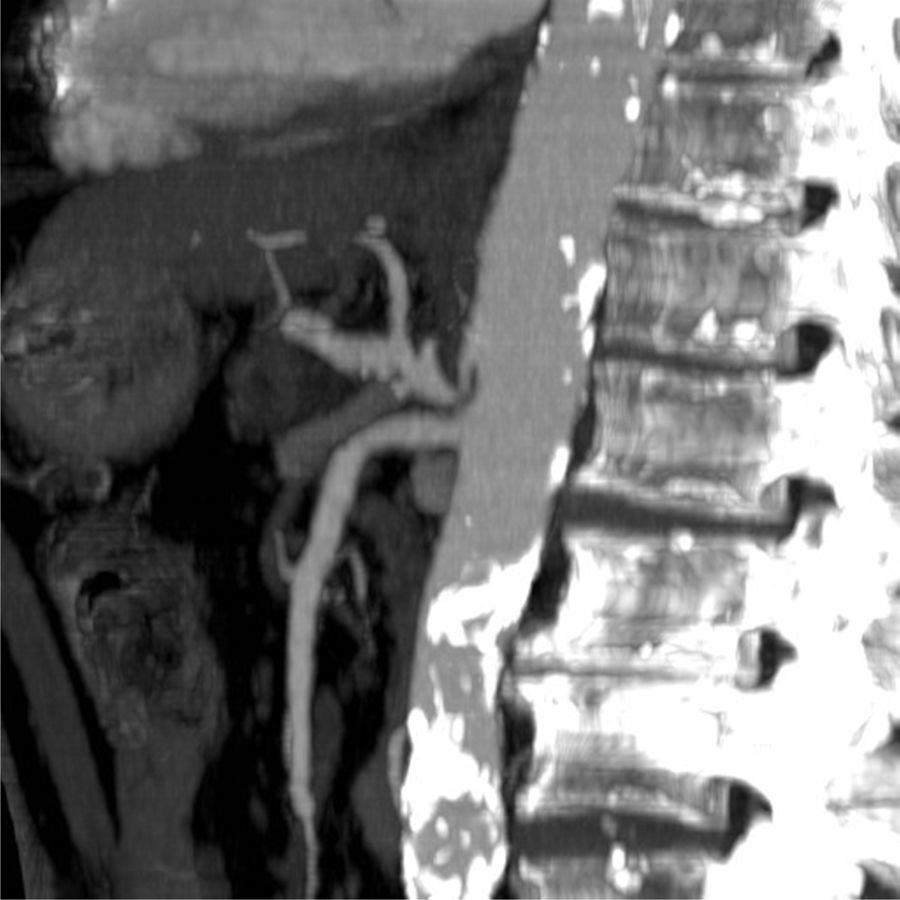
Likewise, an important amount of stenosis was observed at the origin of the celiac trunk (Fig. 1) with post-stenotic dilatation and partial thrombosis of the lumen, suggestive of median arcuate ligament syndrome. The study was completed with abdominal aortography, which confirmed the stenosis at the origin of the celiac trunk that was causing a delay in contrast velocity through the common hepatic artery, with preferential filling of the hepatic artery from the superior mesenteric artery. The degree of stenosis was modified with respiratory movements, becoming normalised on inspiration and more accentuated on forced expiration, which suggested the presence of an arcuate ligament as the extrinsic cause of the stenosis. The involvement of the vascular lumen at rest was around 50% and there was pathologic pressure gradient.
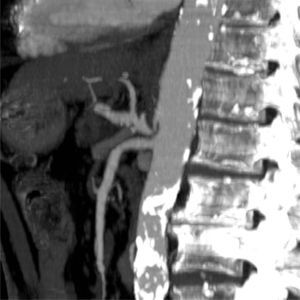
The patient had scheduled surgery under general anaesthesia. The arcuate ligament was completely dissected (Fig. 2). Intraoperatively, proper flow was confirmed in the celiac trunk and hepatic artery prior to clamping of the gastroduodenal vessel, without requiring further vascular treatment and concluding the surgery with pancreaticoduodenectomy and ducto-jejunostomy. The anatomic pathology study reported infiltrating ductal adenocarcinoma, G3 pT3 pN1 L1 V1 Pn1. The patient progressed favourably with no postoperative complications.
Pancreaticoduodenectomy is the treatment of choice for tumours of the pancreatic-duodenal junction. This procedure involves the interruption of the pancreaticoduodenal vessels, which is a key step in patients with stenosis of the celiac trunk. In these cases, collateral arcades are formed from the superior mesenteric artery, mainly from the inferior pancreaticoduodenal to the gastroduodenal artery, through the area of the head of the pancreas. The problem is in procedures like pancreaticoduodenectomy, in which all the collateral circulation is interrupted, with the risk for hepatic, gastric and splenic necrosis due to ischaemia.
Lateral aortic angiography is the gold standard method for diagnosis.1 Stenosis of the celiac trunk is present in 12.5%–49% of patients who undergo abdominal angiography2 and is considered significant when greater than 50% of the lumen. The most frequent cause of stenosis is extrinsic compression of the arcuate ligament, which is a connective tissue ligament that crosses both transversal and anterior to the vertebral bodies and the abdominal aorta, followed by arteriosclerosis; these two causes represent 90% of these stenoses. The main angiographic signs of compression by the arcuate ligament are stenosis of the celiac trunk in final expiratory and inspiratory phases,1 as in our case, confirming the aetiology and requiring no vascular procedure after the dissection of the ligament.
The largest series published is from the Beaujon Hospital, reported by Gaujoux et al.,3 which evaluated the existence of celiac trunk stenosis before pancreatic surgery in 545 patients. The series had an incidence of stenosis in the series of 11% and most cases were secondary to extrinsic compression by the arcuate ligament.
Muros et al.4 concluded that significant stenosis of the celiac trunk is a risk factor for severe complications after pancreaticoduodenectomy as well as pancreatic fistula, haemorrhage and re-operation. Nonetheless, in the study by Smith et al.,5 there was no evidence of an association between significant stenosis of the celiac trunk and increased postoperative complications.
Standard treatment is dissection of the arcuate ligament to release the pressure on the celiac trunk, and the arterial flow is later confirmed by palpation or Doppler ultrasound. The gastroduodenal artery occlusion test recommended by Bull et al.6 is done by palpating the pulse of the hepatic artery before and after clamping the gastroduodenal artery. Revascularisation of the celiac trunk should be considered when, after dissection of the ligament, perfusion either does not improve or is poor after gastroduodenal clamping and when the arterial wall is damaged after a long period of extrinsic compression. If direct anastomosis is not possible or reliable, a bypass is created with the saphenous vein, radial artery or prosthesis. Recent studies report the effectiveness of the use of arterial stents, although always in association with the surgical dissection of the ligament because their primary use is not well defined.7
Please cite this article as: del Hoyo Aretxabala I, Gómez García P, Cruz González MIC, Ruiz Carballo S, Iturburu Belmonte I. Estenosis del tronco celíaco por el ligamento arcuato, ¿un riesgo en la duodenopancreatectomía cefálica? Cir Esp. 2015;93:541–543.
This manuscript has not been presented at any medical conference.