Familial amyloid polyneuropathy (FAP) is a dominant autosomal disease that is progressive and fatal. It is characterised by deposits of transthyretin (TTR), a protein that is predominantly synthesised in the liver,1,2 and clinical manifestations depend on the type of organ involved.3 Cardiac involvement presents as a restrictive cardiomyopathy, which is the main cause of morbidity and mortality.4,5
The only effective treatment is liver transplantation (LT); meanwhile, in patients who present important cardiac involvement, lung and heart transplantation are indicated.4,5We present our experience with 2 cases of simultaneous heart and liver transplantation due to FAP.
Case 1The patient is a 61-year-old woman from the Canary Islands with a family history of FAP diagnosis. In 2002, her symptoms began with weight loss and paraesthesia. A genetic study demonstrated the presence of the Glu89Lys mutation, which provided the diagnosis of FAP. Echocardiogram detected restrictive cardiomyopathy. Abdominal CT and ultrasound were normal. Serology was negative.
In January 2005, heart transplantation was performed by means of the Lower–Shumway–Barnard technique, which was followed by LT using the inferior vena cava preservation technique, without bypass. In addition, a domino transplantation was carried out without incident. The pathology study of the heart reported primary amyloidosis. Postoperative evolution was favourable. The postoperative echocardiogram demonstrated left and right ventricles that were not dilated and preserved systolic function. The patient was discharged 24 days post-transplantation.
Currently, the patient is alive and continues to have adequate hepatic and cardiac function 9 years after the combined transplantation. Her mobility is reduced to an armchair-to-bed range due to the advanced stage of her disease at the time of transplantation.
Case 2The patient is a 62-year-old man from the Canary Islands, with no prior history of interest. In May 2006, he was diagnosed with cardiomyopathy and moderate dysfunction of the left ventricle. Genetic studies demonstrated the presence of the Val122lle mutation. He was diagnosed with FAP, biventricular cardiac involvement and sensorimotor polyneuropathy. Physical examination revealed systolic murmur III/VI and mild hepatomegaly. Echocardiogram showed the left ventricle with acute concentric hypertrophy and signs of moderate pulmonary hypertension. Abdominal ultrasound revealed mild hepatomegaly and ascites, attributed to fluid overload.
In September 2007, the patient received an orthotopic heart transplant using the Lower–Shumway–Barnard technique. Afterwards, orthotopic LT was performed using the inferior vena cava preservation technique, without bypass. A subcapsular wedge of the liver was analysed, which showed no alterations, so it was used for domino transplantation. The patient was discharged 17 days post-transplantation and showed good progress. Histologic analysis of the endomyocardial biopsy demonstrated transthyretin-positive amyloid deposits.
Seven years after heart/liver transplantation, the patient has good hepatic and cardiac function, no signs of neurologic progression and LV with normal systolic function (LVEF 74%).
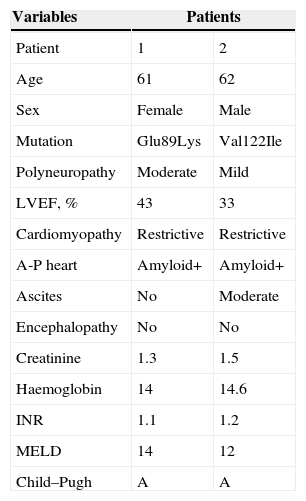
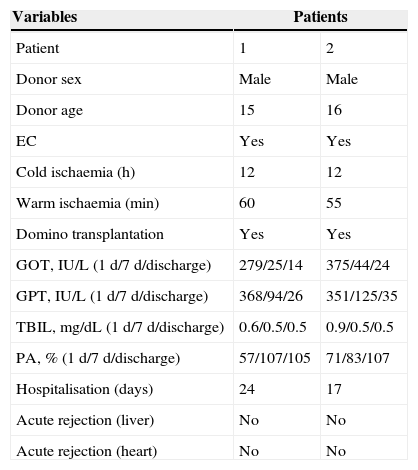
Tables 1 and 2 show the clinical, demographic and perioperative characteristics of the patients in our series who underwent simultaneous heart and liver transplantation.
Preoperative Clinical and Demographic Characteristics of Patients who Received Simultaneous Heart and Liver Transplants.
| Variables | Patients | |
|---|---|---|
| Patient | 1 | 2 |
| Age | 61 | 62 |
| Sex | Female | Male |
| Mutation | Glu89Lys | Val122Ile |
| Polyneuropathy | Moderate | Mild |
| LVEF, % | 43 | 33 |
| Cardiomyopathy | Restrictive | Restrictive |
| A-P heart | Amyloid+ | Amyloid+ |
| Ascites | No | Moderate |
| Encephalopathy | No | No |
| Creatinine | 1.3 | 1.5 |
| Haemoglobin | 14 | 14.6 |
| INR | 1.1 | 1.2 |
| MELD | 14 | 12 |
| Child–Pugh | A | A |
Perioperative Characteristics in Simultaneous Heart and Liver Transplantation.
| Variables | Patients | |
|---|---|---|
| Patient | 1 | 2 |
| Donor sex | Male | Male |
| Donor age | 15 | 16 |
| EC | Yes | Yes |
| Cold ischaemia (h) | 12 | 12 |
| Warm ischaemia (min) | 60 | 55 |
| Domino transplantation | Yes | Yes |
| GOT, IU/L (1 d/7 d/discharge) | 279/25/14 | 375/44/24 |
| GPT, IU/L (1 d/7 d/discharge) | 368/94/26 | 351/125/35 |
| TBIL, mg/dL (1 d/7 d/discharge) | 0.6/0.5/0.5 | 0.9/0.5/0.5 |
| PA, % (1 d/7 d/discharge) | 57/107/105 | 71/83/107 |
| Hospitalisation (days) | 24 | 17 |
| Acute rejection (liver) | No | No |
| Acute rejection (heart) | No | No |
PA, prothrombin activity; TBIL, total bilirubin; EC, extracorporeal circulation; GOT, glutamic-oxaloacetic transaminase; GPT, glutamic pyruvic transaminase.
The first combined liver and heart transplantation was published in 1984 by Starzl et al.6,7 By 2013, 143 combined heart/liver transplantations had been reported, with operative mortality rates that ranged between 0 and 25%.8
The surgical options that are discussed in this procedure are the following: (1) heart transplantation and LT several months afterwards; (2) heart transplantation followed by LT within the same operation after chest closure; and (3) heart transplantation followed by LT while the heart is being reperfused in cardiopulmonary bypass.8
The sequential approach poses a risk for cardiac amyloid deposits while waiting for LT; in addition, the fact that the patient receives 2 grafts from different donors could lead to immunological problems.7 The simultaneous approach presents disadvantages such as bleeding, coagulopathy and prolonged surgical times.7 In fact, Shaw et al.9 reported that induced coagulopathy took several hours for reversal. In our series, the sequence of the combined technique was, first of all, heart transplantation with extracorporeal circulation (EC). After this procedure, EC was disconnected, heparin was neutralised and the chest was then closed; subsequently, LT was initiated. This type of approach provides adequate haemodynamic control after heart transplantation and, although it meant a significant increase in liver ischaemia time, this did not influence the recovery of graft function.
The presence of 2 organs in one recipient, whether or not they come from the same donor, poses special immunological problems. The liver seems to play a protective immunological role when the transplantation is done in combination with other organs, so there is a lower incidence of rejection and greater survival than in cases of solitary extrahepatic organs.7,10
In conclusion, combined heart/liver transplantation is indicated in patients who present severe cardiac dysfunction and FAP. The induction of the tolerance of the liver to other extrahepatic organs promotes a lower incidence of rejection and greater survival of transplanted hearts.
Please cite this article as: Marcacuzco Quinto AA, Manrique Municio A, Justo Alonso I, Caso Maestro Ó, Jiménez Romero LC, Moreno Gonzalez E. Trasplante hepático y cardiaco simultáneo en pacientes con polineuropatía amiloidótica familiar. Cir Esp. 2015;93:543–545.