Metamizole is the second most widely used analgesic in Spain1 and rarely causes agranulocytosis (<10000),2 which is potentially fatal. We present a case of agranulocytosis associated with metamizole that led to the later development of deep cervical abscesses, which were treated with vacuum-assisted closure (VAC) therapy.
Case ReportThe patient is a 61-year-old woman from London with no known drug allergies. She had been treated for ophthalmic postherpetic neuralgia with paracetamol at 1g/8h, pregabalin at 150mg/8h and metamizole at 575mg/8h for 45 days.
She came to our Emergency Department after 4 days of fever (39°C) and odynophagia. In the previous 24h, the patient had had diarrhoea with no blood, mucous or abdominal pain. She came to the ER after the presentation of nausea, hypotension and diaphoresis.
The patient was conscious and coherent, with good colouring although dehydrated. The pharynx was hyperaemic with tonsillar hypertrophy, no pultaceous tonsillitis, and lateral cervical lymphadenopathies, predominantly on the left side. She was eupneic with SO2 96% in spite of oxygen therapy with a Venturi® mask at 35%. Severe haemodynamic instability required noradrenalin at 5ml/h (0.25mcg/kg/min), with persistent hypotension and tachycardia.
Blood work showed pancytopenia 2.3×106/mm3 erythrocytes, 89000×103/mm3 platelets, 1200×103/mm3 leukocytes, and absolute neutropenia (0%). Biochemistry revealed kidney failure (creatinine: 3.6mg/dL).
We arrived at the diagnosis of severe sepsis of unknown origin and grade IV neutropenia with a possible haematologic origin or agranulocytosis due to metamizole.
Empirical treatment with imipenem was initiated, and noradrenaline was increased to 14ml/h (0.71mcg/kg/min).
Blood cultures and pharyngeal/anal swab studies were negative. Bone marrow aspiration confirmed the central origin of the pancytopenia, so granulocyte-colony stimulating factor was added to the treatment.
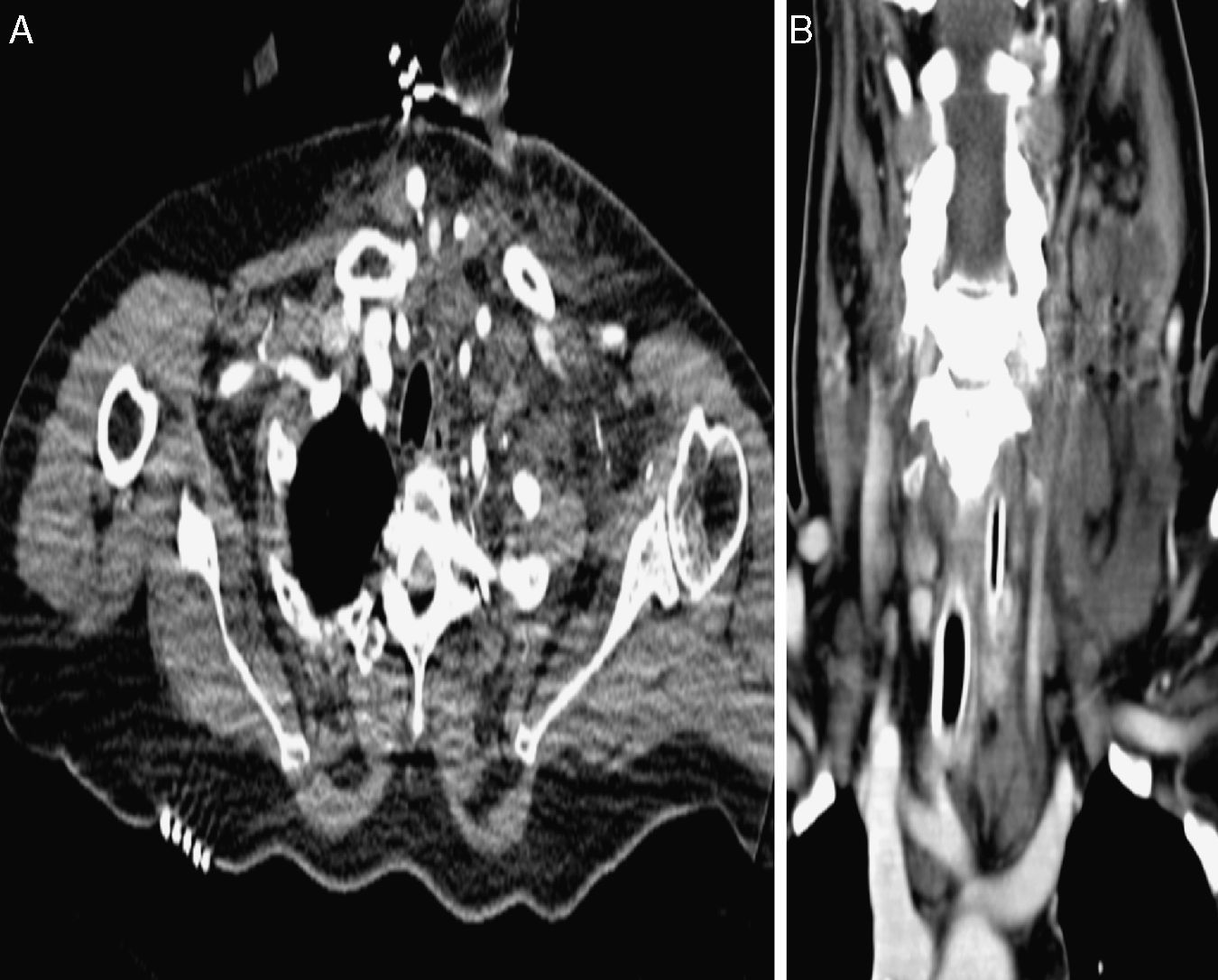
The lateral cervical lymphadenopathies then progressed to left lateral cervical cellulitis with extension towards the right, which CT showed to be fat stranding and oedema without collections (Fig. 1A).
Given the worsening symptoms and lab results, tachypnoea at 40 breaths per minute and increased oedema, the patient was transferred to the ICU, where oropharyngeal intubation was performed.
Dobutamine was initiated due to cardiac dysfunction (EF: 40%) as well as amiodarone and cardioversion for atrial flutter with bursts of VT leading to atrial fibrillation. The patient presented shock liver with altered coagulation and hypoalbuminaemia (2.5mg/dl). Fluconazole and linezolid were added for extended coverage.
Over the course of the following 2 weeks, the patient's condition improved favourably: the oedema diminished, kidney function was re-established and she recovered from neutropenia. CT detected parapharyngeal and paracarotid cervical abscesses that were compressing the internal jugular vein and extended towards the mediastinum (Fig. 1B).
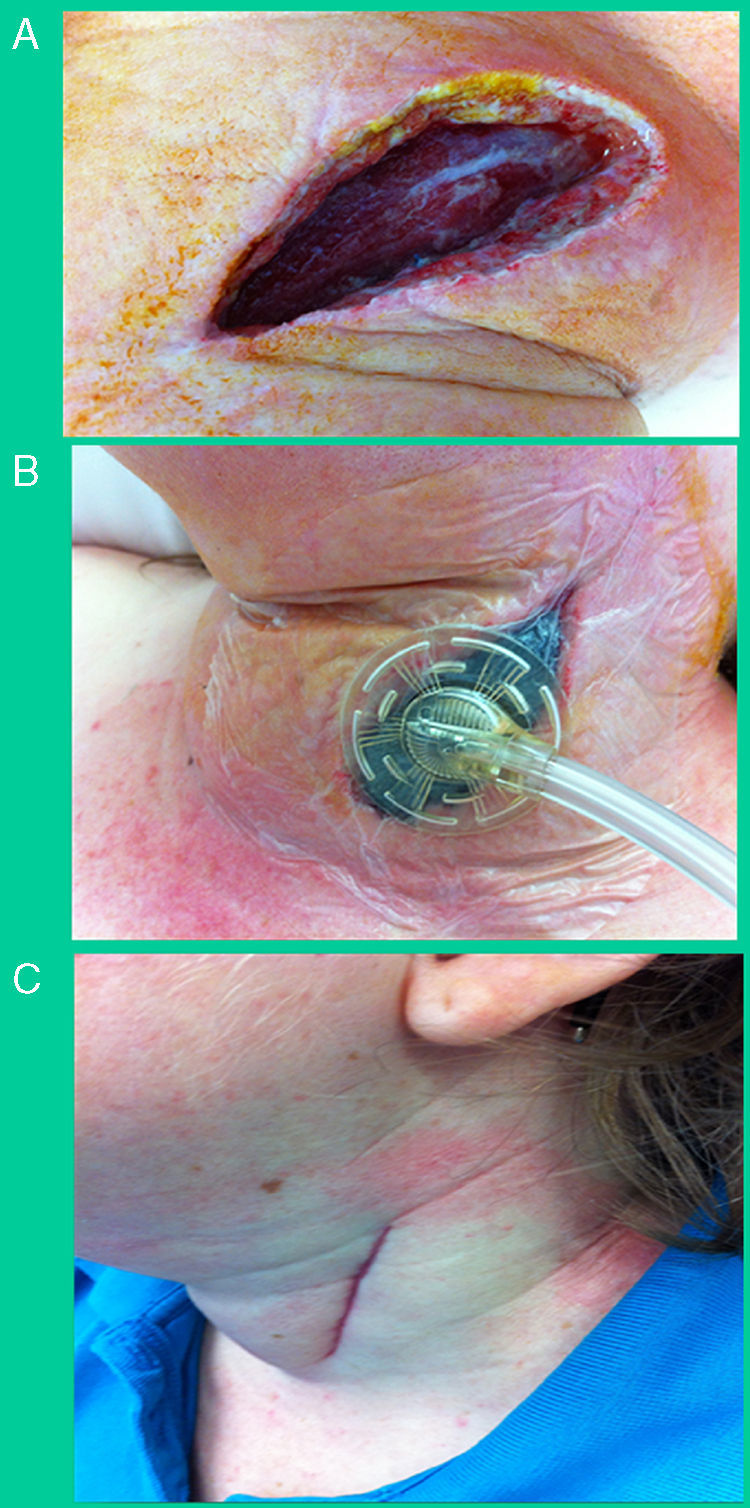
Left lateral cervical incision was used for debridement (Fig. 2A). Purulent exudate was drained, which was positive for imipenem-resistant P. aeruginosa, so treatment was changed to piperacillin/tazobactam. An intermittent negative pressure closure system (VAC® Therapy, KCI Inc., TX, USA) was applied to the wound and abscess cavity (Fig. 2B). The patient's progress was favourable and she was discharged 60 days after hospital admittance (24 days in ICU), with no permanent side effects (Fig. 2C).
(A) Debridement using a left oblique lateral cervical incision after drainage and evacuation; (B) application of vacuum-assisted closure therapy at the site of the cervical debridement, mid-way through treatment (day 7); (C) results 27 days after discharge and 3 months after hospital admittance.
Agranulocytosis associated with metamizole is rare but potentially fatal, supposedly determined by genetic immunological factors. There are geographical differences in incidence that are explained by variations in HLA alleles and the presence/absence of chromosomal aberrations.3 It is a hypersensitivity reaction, so, once sensitised, the severity of the reaction is not dose-dependent. Exposure over long periods at high doses increases the probability for sensitisation and later development of metamizole-related agranulocytosis.4
In the 1970s, this drug was prohibited in several countries, among them the United States, United Kingdom and Australia. It seems that agranulocytosis related with the use of metamizole is more frequent in British populations, so the administration of metamizole is not recommended in patients of this origin.
In suspected cases, the administration of this drug should be suspended and a series of blood tests is necessary. If confirmed, the use of wide-spectrum antibiotic therapy is recommended, which can be used in monotherapy (3rd generation cephalosporins, carbapenems or beta-lactams) or by combining 2 antibiotics (beta-lactams, anti-pseudomonas plus aminoglycoside). Recently, there have been published reports of Pseudomonas spp. resistance to carbapenems (up to 21% for imipenem); thus, in cases of acute nosocomial infections, another antipseudomonal antibiotic should be added.5 The administration of granulocyte-colony stimulating factor is also recommended, which accelerates recovery from neutropenia and shortens hospital stay.6
Deep cervical abscesses affect interfascial planes and can have multiple origins, the most frequent of which are upper respiratory infections, tonsillitis, acute otitis media and tooth extractions. The most frequently isolated germs are streptococci and staphylococci, and it is unusual to isolate Pseudomonas spp. after neutropenia.7 They cause systemic and local symptoms with dysfunction of the upper respiratory or digestive tract and can even lead to death due to airway obstruction, aspiration after fistulisation to the pharynx, erosion or thrombosis of the large vessels and extension to the mediastinum.8 High doses of wide-spectrum intravenous antibiotics are recommended along with surgical drainage of the collections.7
The application of VAC therapy for the treatment of cervical abscesses is innovative. It provides excellent results as it prevents dissemination of the infection, accelerates deep healing and reduces the need for reinterventions.9,10
Please cite this article as: Iskra MP, Membrilla E, Isbert F, Pañella C, Sancho J. Sepsis grave por absceso cervical profundo tras agranulocitosis por metamizol. Cir Esp. 2015;93:e83–e85.
Presented at the 3rd Conference of Infectious and Emergency Clinical Cases of the SOCMUE; awarded second prize for best oral presentation (previously unpublished)