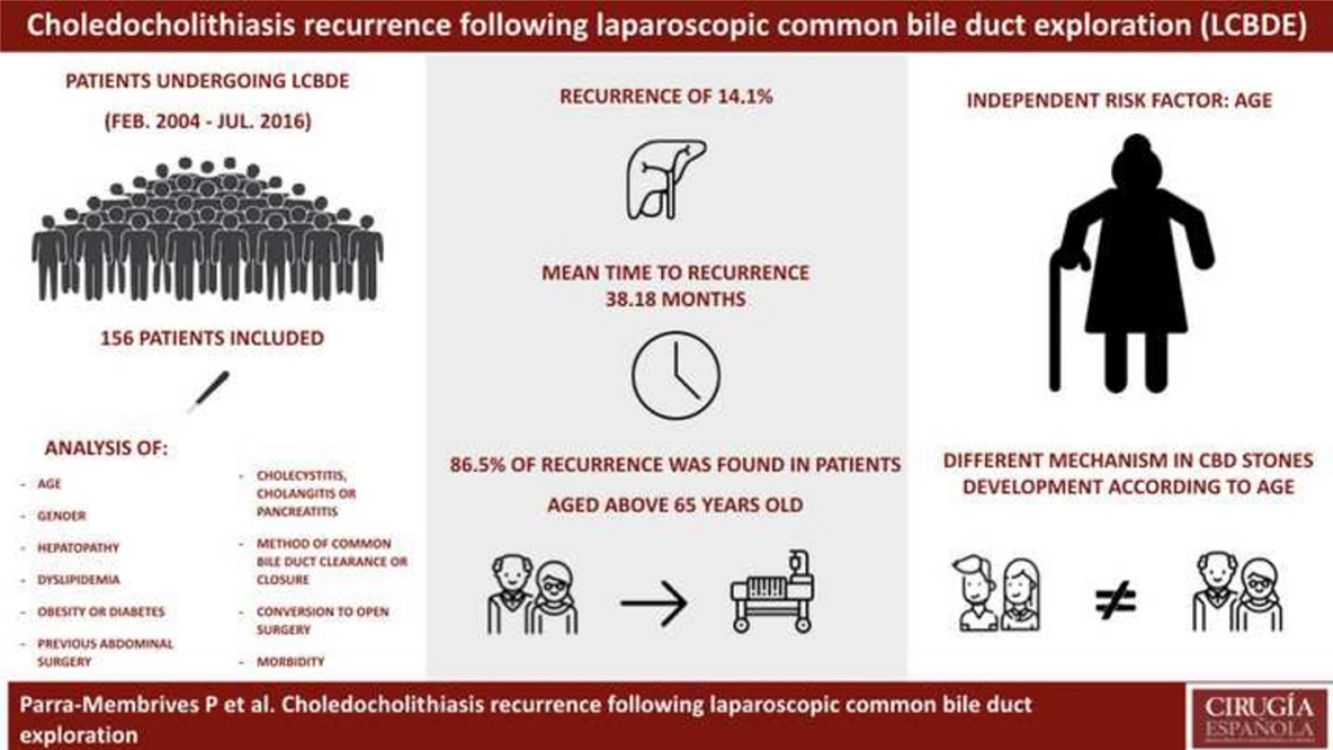
Choledocholithiasis may be treated following an endoscopic approach or by laparoscopic common bile duct exploration (LCBDE). Stone recurrence following endoscopic management has been extensively investigated. We analyze the risk factors associated with stone recurrence following LCBDE.
MethodsPatients who underwent LCBDE from February 2004 to July 2016 were examined in an univariate and multivariate analysis to assess the association of stone recurrence with the following variables: gender; age; hepatopathy; dyslipidemia, obesity or diabetes mellitus; previous abdominal surgery; presence of cholecystitis, cholangitis or pancreatitis; preoperative liver function tests, number of retrieved stones; method of common bile duct clearance and closure; presence of impacted or intrahepatic stones; conversion to open surgery and postoperative morbidity.
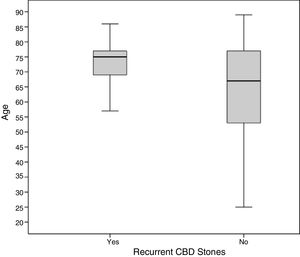
ResultsA total of 156 patients were included. Recurrence rate for choledocholithiasis was 14.1% with a mean time to recurrence of 38.18 month. Age was the only independent risk factor for stone recurrence at univariate and multivariate analysis. No patient aged under 55 years developed new common bile duct stones, and 86.4% of the recurrences occurred in patients aged above 65.
ConclusionsAge is the only independent risk factor associated to choledocholithiasis recurrence following LCBDE. Different mechanism in common bile duct stone development may be present for younger and older patients.
La coledocolitiasis puede tratarse mediante abordaje endoscópico por colangiopancreatografía endoscópica retrógrada o realizando una exploración laparoscópica de la vía biliar principal (ELVBP) durante la colecistectomía. La recurrencia de la coledocolitiasis y sus factores de riesgo tras extracción endoscópica han sido ampliamente investigados. Nuestro objetivo es analizar los factores de riesgo asociados con la recurrencia de cálculos en la vía biliar principal después de una ELVBP.
MétodosLos pacientes que se sometieron a ELVBP desde febrero de 2004 a julio de 2016 fueron examinados en un análisis univariante y multivariante para estudiar la asociación de recurrencia de coledocolitiasis con las siguientes variables: sexo; edad; presencia de hepatopatía; dislipemia, obesidad, o diabetes mellitus; cirugía abdominal previa; presencia de colecistitis, colangitis o pancreatitis al diagnóstico; pruebas de función hepática preoperatorias, número de cálculos recuperados; método de limpieza y cierre del conducto biliar común; presencia de litiasis coledocianas impactadas o intrahepáticas; conversión a cirugía abierta y morbilidad postoperatoria.
ResultadosSe incluyeron 156 pacientes. La tasa de recurrencia de la coledocolitiasis fue del 14,1%, con un tiempo medio de recurrencia de 38,18 meses. La edad fue el único factor de riesgo independiente para la recurrencia de cálculos en el análisis univariante y multivariante. Ningún paciente menor de 55 años desarrolló nuevos cálculos en la vía biliar principal, y el 86,4% de las recurrencias se produjo en pacientes mayores de 65 años.
ConclusionesLa edad es el único factor de riesgo independiente asociado a la recurrencia de coledocolitiasis después de ELVBP. Diferentes mecanismos en el desarrollo de cálculos en la vía biliar principal pueden estar presentes para pacientes más jóvenes y de edad más avanzada.
Common bile duct (CBD) stones are a frequent problem, which quoted prevalence lies around 10% of the patients with symptomatic gallstones.1–3 At present, there are mainly two methods available to deal with choledocholithiasis: the two-stage approach with endoscopic retrograde cholangiopancreatography plus endoscopic sphincterotomy (ERCP+ES) and deferred laparoscopic cholecystectomy and the single stage approach involving laparoscopic common bile duct exploration (LCBDE) and cholecystectomy during the same procedure. Despite the endoscopic approach has been widely popularized, many clinical trials4–10 and several meta-analysis1,11–14 have stated that both methods are equally effective in terms of common bile duct stones clearance and that they share similar morbidity and mortality rates. It is difficult to find reliable information about the long-term outcomes of CBD stones treatment, since most patients become free of symptoms and leave medical institution and consequently are lost for follow-up. Yet, independently of the method chosen for choledocholithiasis management, recurrence of CBD stones may occur. A part of this group of patients reveal actually stones that were not able to be retrieved or were inadvertently left behind during the first procedure, but furthermost of them may present stones that develop de novo in the biliary tree. The literature reveals how incidence of long-term CBD stones recurrence is slightly higher following the two-stage approach ranging from 4% to 21% of the treated patients compared to the 2.1% to 8% ratio after LCBDE.10,11,15–22 Risk factors for recurrent stones in the patients that had undergone an ERCP plus ES have been extensively analyzed. The presence of CBD dilatation or angulation, the existence of a periampulary diverticulum and prior biliary surgery have both shown to favor recurrent CBD stone development.15–17,23–25 In addition, inflammation of the bile duct because of chronic reflux of the duodenal contents after sphincterotomy and papillary stenosis are also suggested causes for choledocholithiasis recurrence subsequent to the endoscopic treatment.16,26,27 Yet, this factor cannot play a relevant role after the single stage approach, since the standard surgical procedure do not alter the function of the sphincter of Oddi.16,27 Moreover, few reports have addressed the issue of risk factors associated with CBD stones recurrence following LCBDE. The aim of the study was to examine the rate and risk factors that may influence long term CBD stones recurrence development following laparoscopic choledocholithotomy.
MethodsPatientsWe performed a retrospective analysis of the prospectively collected database of all the patients who underwent a LCBDE at our center from February 2004 to July 2016. All patients provided informed consent prior to surgery. The institutional review board approved the study. The management strategy of our institution for CBD stones involves LCBDE for all the patients that are diagnosed with choledocholithiasis. The endoscopic approach is only indicated in those patients without a dilated common bile duct (<9mm) or those that are not fit for surgery because of a poor performance status. At last, open surgery is only offered to patients not suitable for the laparoscopic approach, who had undergone an unsuccessful attempt of endoscopic CBD removal. Choledocholithiasis was diagnosed either preoperatively by abdominal ultrasonography and/or magnetic resonance cholangiopancreatography (MRCP) or intraoperatively at cholangiography (IOC).
Operative TechniqueThe four surgeons of the Hepato-Bilio-Pancreatic Surgery Unit at our center performed all the procedures. Abdominal access was granted using five trocars (three 5-mm trocars and two 10-mm trocars). Exposure of the bile duct was facilitated by upward and some lateral retraction of the gallbladder. The cystic duct was milked upwards to the gallbladder and clipped at the beginning of the procedure to avoid the passage of stones to the CBD during manipulation. A supraduodenal longitudinal choledochotomy was the preferred method for CBD exploration. The bile duct was explored directly if the patient had undergone a recent MRCP demonstrating a large stone or the presence of several stones. Else an IOC was performed prior to choledochotomy to discard a spontaneous passage of the stones throughout the papilla prior to surgery. A combination of saline irrigation, Dormia basket or balloon extraction technique was employed to remove CBD stones under flexible choledochoscopic guidance. Bile duct clearance was than guaranteed by intraoperative fiber-choledochoscopy or cholangiography performance. The choledochotomy closure was completed leaving a T-tube in the early cases. From year 2006 to 2013 we routinely performed antegrade stenting for biliary decompression before bile duct closure. Recently, since mid-2013, most patients underwent a primary choledochorraphy without stenting. To finish surgery, the gallbladder was removed on a standard fashion. Failed bile duct clearance was defined as the inability to clear diagnosed choledocholithiasis during surgery requiring further procedures. All CBD stones that were evidenced from the first postoperative day to six month following surgery, including those that appeared during the postoperative trans-Kehr cholangiography, were assumed as retained stones.
Hospital Discharge and Follow-up ScheduleAsymptomatic patients with primary CBD closure or antegrade stenting were discharged from hospital 24 to 48h after surgery if correct oral intake was achieved. The patients that received a T-tube were delivered after a trans-Kehr cholangiography proved no residual stones and successful tube clamping was achieved.
Postoperative follow-up visits were scheduled one and six months after surgery to check the clinical status of the patients and obtain liver function laboratory tests to exclude cholestasis. Asymptomatic patients with normal biliary tests received no further appointments but were advised to return if they developed symptomatic at any time. Patients with unusual findings underwent ultrasound examinations and/or a MRCP to rule out the presence of retained stones.
For the purpose of this study, any postoperative contact of the patients with the institution in which the surgical procedure was conducted or with the other Hospitals of the Public Health System that assist the complete population of the town was checked out reviewing the available electronic clinical registries and charts and any data about new diagnosis of CBD stones was recorded. The date of the last contact of the patient with any institution was employed to calculate de surveillance period.
Data Collection and DefinitionsThe surgical clearance of CBD stones was considered successful if the surgery finished with the removal of all preoperatively known choledocholithiasis. Retained common bile duct stones were defined as choledocholithiasis that were not known to have been left behind during surgery at the end of the surgical procedure but diagnosed in the first 6 postoperative month. As previously described in the literature by many authors, recurrence of choledocholithiasis was defined as the development of stones since 6 month after the complete removal of the initial CBD stones.15,16,26,28 Timing of the development of the recurrent stones and level of alkaline phosphatase at diagnosis were recorded. We analyzed the association of recurrent CBD stones occurrence with the following variables: gender; age; previous hepatopathy; metabolic syndrome defined as the presence of dyslipidemia, obesity or diabetes mellitus; American Society of Anesthesiologists (ASA) score; preoperative presence of either cholecystitis, cholangitis or pancreatitis; preoperative laboratory tests including total bilirubin (TB), gamma-glutamyl-transpeptidase (GGT), aspartate-aminotransferase (AST) and alkaline phosphatase (AP) serum levels; postoperative level of AP between 6 and 12 month after surgery, preoperative diameter of the CBD; number of CBD stones identified intraoperatively; method employed for CBD clearance and for CBD closure; presence of impacted stones at the papilla or intrahepatic stones; conversion to open surgery and postoperative complications following the validated classification system by Dindo–Clavien.29,30
StatisticsAll quantitative values were expressed as the mean±the standard deviation. Categorical variables were presented as values and percentages. The relationship between recurrent CBD stones development and all the variables of the study was analyzed employing the Chi-square test and the Mann–Whitney U test as appropriate. Binary logistic regression was used for performing multivariate analysis, which determines significant risk factors predicting choledocholithiasis recurrence. An inclusion criterion of P<.2 was adopted for multivariable analysis in our study. P values <.05 were considered statistically significant. Statistical analysis was performed using the SPSS for Mac v.20 software program.
ResultsA total of 156 patients underwent elective LCBDE for choledocholithiasis during the study period. Mean age was 65.35±15.68 years (range 25–89 years). There were 88 women (56.4%) and 68 men (43.6%). All the patients received a choledochotomy as previously described. Sixteen (10.3%) patients had to be converted to open surgery due to severe adhesions, to the presence of impacted stones at the papilla that could not be retrieved or to the presence of Mirizzi syndrome that made laparoscopic dissection dangerous. The absence of residual stones was ruled out by intraoperative fiber-choledochoscope exploration in 93.3% of the patients whereas an intraoperative cholangiography was performed in further 14.7% of the cases. The surgical clearance of CBD stones was successful in 154 patients (98.7%). Ten patients (6.4%) revealed to have retained choledocholithiasis following the referred diagnostic criteria.
One hundred nine patients (69.9%) experienced no morbidity following LCBDE and 17.3% of the patients developed only low-grade problems (Dindo–Clavien grade 1 and 2). Furthermore, 12.8% of the patients had Dindo–Clavien grade 3 complications or superior. There were no mortality cases directly related to surgery, but one patient whose LCBDE failed underwent an ERCP for bile duct clearance and developed a sever pancreatitis that finally caused her decease.
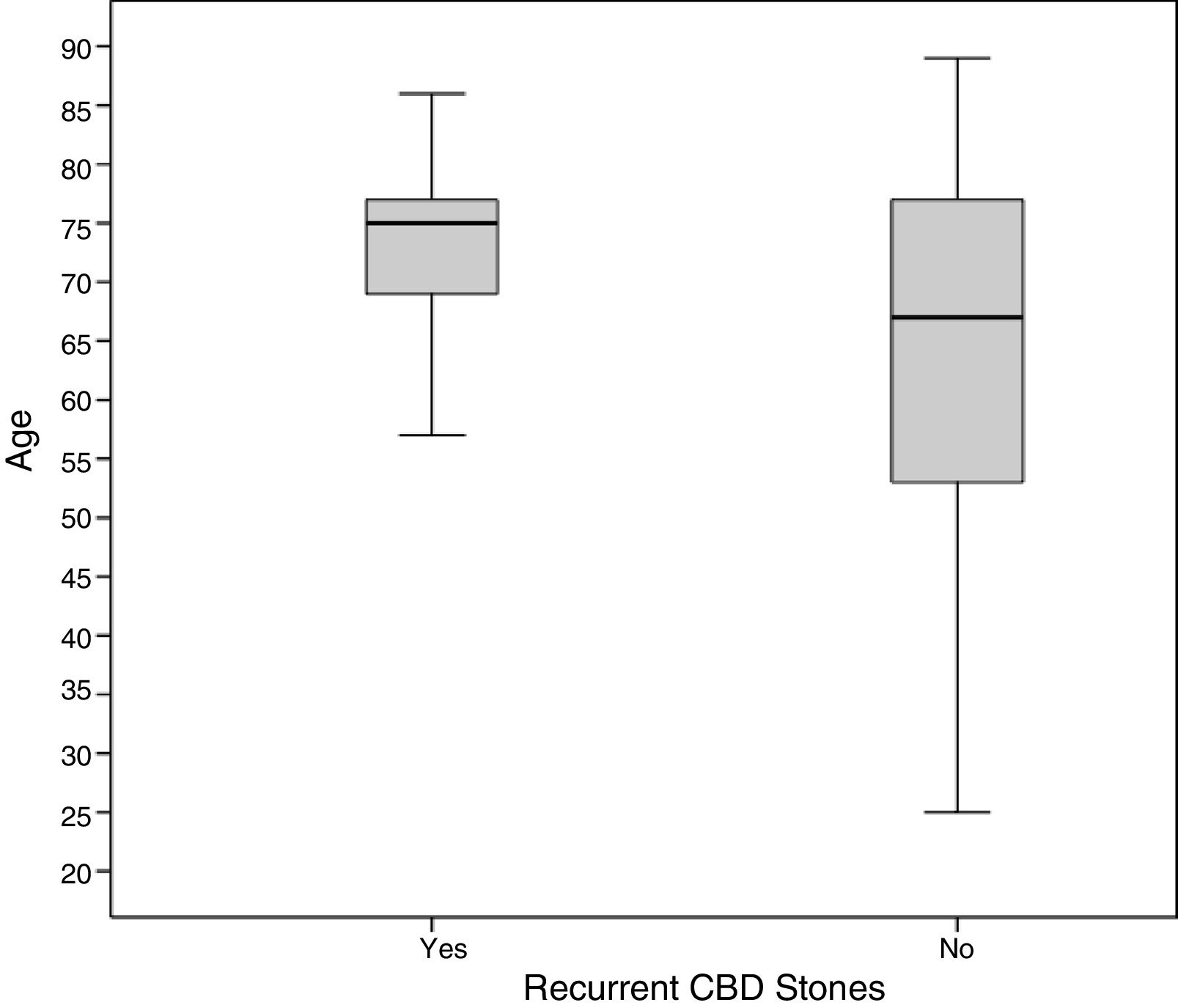
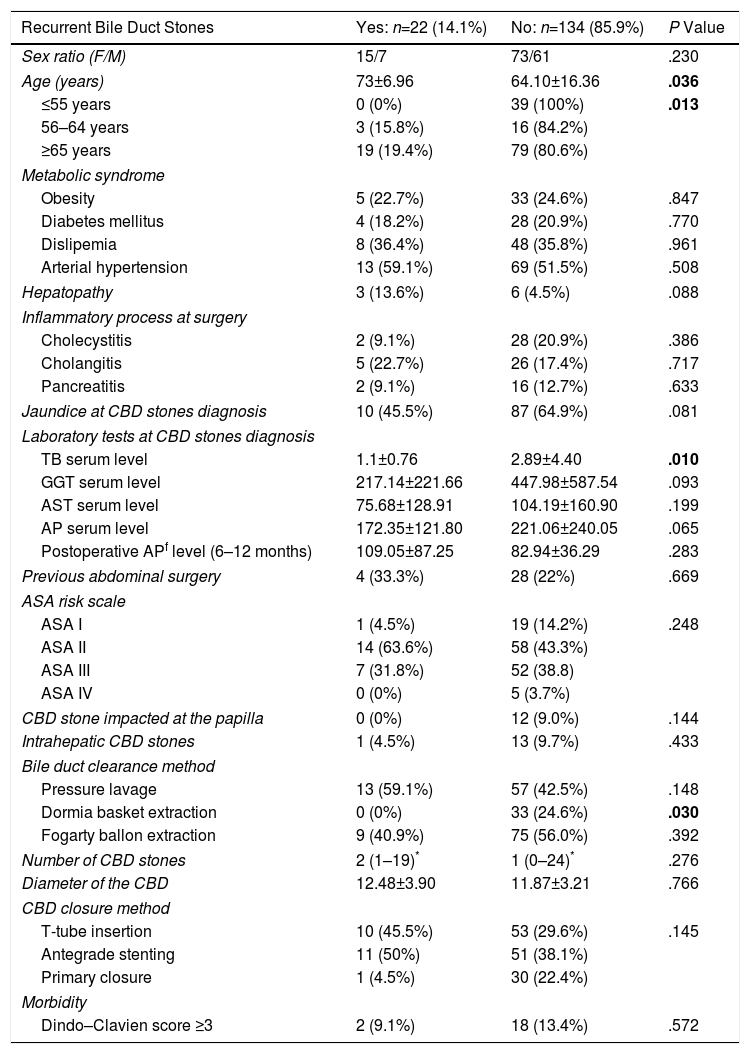
The mean surveillance period was 77.08±42.20 month. The recurrence rate for CBD stones was 14.1% (22 of 156 patients). Mean time until symptomatic recurrence of choledocholithiasis was 38.18 month (median of 27.50 and range 8–103 month). Age and preoperative level of serum bilirubin were the only variables statistically associated to stone recurrence at the univariate analysis as listed in Table 1. However, only age remained an independent risk factor for choledocholithiasis recurrence in the multivariate analysis (P=.022). Remarkably, all the patients that later suffered a new episode of choledocholithiasis were aged over 55 years at the moment of surgery and 86.4% of these patients were 65 or older (Fig. 1 and Table 1).
Univariate Analysis of Risk Factors for Recurrent Bile Duct Stones Following LCBDE.
| Recurrent Bile Duct Stones | Yes: n=22 (14.1%) | No: n=134 (85.9%) | P Value |
|---|---|---|---|
| Sex ratio (F/M) | 15/7 | 73/61 | .230 |
| Age (years) | 73±6.96 | 64.10±16.36 | .036 |
| ≤55 years | 0 (0%) | 39 (100%) | .013 |
| 56–64 years | 3 (15.8%) | 16 (84.2%) | |
| ≥65 years | 19 (19.4%) | 79 (80.6%) | |
| Metabolic syndrome | |||
| Obesity | 5 (22.7%) | 33 (24.6%) | .847 |
| Diabetes mellitus | 4 (18.2%) | 28 (20.9%) | .770 |
| Dislipemia | 8 (36.4%) | 48 (35.8%) | .961 |
| Arterial hypertension | 13 (59.1%) | 69 (51.5%) | .508 |
| Hepatopathy | 3 (13.6%) | 6 (4.5%) | .088 |
| Inflammatory process at surgery | |||
| Cholecystitis | 2 (9.1%) | 28 (20.9%) | .386 |
| Cholangitis | 5 (22.7%) | 26 (17.4%) | .717 |
| Pancreatitis | 2 (9.1%) | 16 (12.7%) | .633 |
| Jaundice at CBD stones diagnosis | 10 (45.5%) | 87 (64.9%) | .081 |
| Laboratory tests at CBD stones diagnosis | |||
| TB serum level | 1.1±0.76 | 2.89±4.40 | .010 |
| GGT serum level | 217.14±221.66 | 447.98±587.54 | .093 |
| AST serum level | 75.68±128.91 | 104.19±160.90 | .199 |
| AP serum level | 172.35±121.80 | 221.06±240.05 | .065 |
| Postoperative APf level (6–12 months) | 109.05±87.25 | 82.94±36.29 | .283 |
| Previous abdominal surgery | 4 (33.3%) | 28 (22%) | .669 |
| ASA risk scale | |||
| ASA I | 1 (4.5%) | 19 (14.2%) | .248 |
| ASA II | 14 (63.6%) | 58 (43.3%) | |
| ASA III | 7 (31.8%) | 52 (38.8) | |
| ASA IV | 0 (0%) | 5 (3.7%) | |
| CBD stone impacted at the papilla | 0 (0%) | 12 (9.0%) | .144 |
| Intrahepatic CBD stones | 1 (4.5%) | 13 (9.7%) | .433 |
| Bile duct clearance method | |||
| Pressure lavage | 13 (59.1%) | 57 (42.5%) | .148 |
| Dormia basket extraction | 0 (0%) | 33 (24.6%) | .030 |
| Fogarty ballon extraction | 9 (40.9%) | 75 (56.0%) | .392 |
| Number of CBD stones | 2 (1–19)* | 1 (0–24)* | .276 |
| Diameter of the CBD | 12.48±3.90 | 11.87±3.21 | .766 |
| CBD closure method | |||
| T-tube insertion | 10 (45.5%) | 53 (29.6%) | .145 |
| Antegrade stenting | 11 (50%) | 51 (38.1%) | |
| Primary closure | 1 (4.5%) | 30 (22.4%) | |
| Morbidity | |||
| Dindo–Clavien score ≥3 | 2 (9.1%) | 18 (13.4%) | .572 |
AP, alkaline phospathase serum level; AST, aspartate aminotransferase serum level; GGT, gamma-glutamyl-transpeptidase serum level; TB, total bilirrubin serum level.
In bold, results statistically significant.
The incidence of silent CBD stones diagnosed in patients who are referred for laparoscopic cholecystectomy have been established around 10%.2 When choledocholithiasis is identified in patients that have their gallbladder still present, passage of the stones throughout the cystic duct into the CBD is assumed and, as a principle, all stones are considered secondary migrated stones. However, CBD stones also develop in patients long after they have undergone a cholecystectomy. A recent study stated a median time of 4 years for cholecystectomized patients to present with symptomatic choledocholithiasis.31 Nevertheless, mean or median time to choledocholithiasis recurrence following any CBD clearance procedure is not very different from the published data for CBD stones diagnosis after simple laparoscopic cholecystectomy ranging from 1.4 to 4 years.16,21,32–34
Since it is difficult to distinguish accurately between migrated stones that were left in situ during surgery and stones that were formed de novo in the CBD postoperatively, most studies made an arbitrary classification of retained and recurrent stones based on the timing of appearance starting from the last therapeutic procedure. The rules of 6-month, 12 month or even of two years have been widely employed to define recurrent stones.15,16,21,26,28 As many other authors before, we used the timing of 6 month to define recurrent stones. This may have affected to our slightly higher recurrence rate when compared to the few studies that highlight this issue. There are mainly two ways in which CBD stones may be left behind during any therapeutic technique. First, the presence of cystic duct lithiasis that may migrate into de CBD duct after the surgical procedure. Even if milked upwards during laparoscopic cholecystectomy, some stones may persist. Complete cystic clearance may be difficult to assure during trans-choledochal choledochoscopy, and, in addition, balloon extraction of choledocholithiasis during either the endoscopic or surgical approach may introduce CBD stones into the cystic duct and may be left behind by this way. Second, false-negative cholangiographic or fiber-choledochoscopic examinations may also misdiagnose the presence of CBD stones. In opinion of the authors, these mechanisms of stone retrieval failure may be responsible for the early cases of stone recurrence, and should therefore better be stated as retained stones, but may hardly cause symptomatic CBD stones after 6 month or many years after. However, the true incidence of retained or recurrent stones is always difficult to assure. Due to the retrospective nature of our study, some asymptomatic CBD stones may not have been diagnosed, particularly if spontaneous passage of CBD stones in 12%–26% of the affected patients is assumed.35,36
Remarkably, most of the studies that analyze the long-term results of ERCP+ES have reported a higher incidence of recurrent stones than after surgery alone.10,15–18,20,21 A recent meta-analysis comparing the single and the two stage approach has also found statistical differences that favor the LCBDE as charged with fewer choledocholithiasis recurrence.11 Thus, different factors may affect new stone development following one or another therapeutic approach. We did not find any relationship with CBD diameter, presence of jaundice or number of stones as suggested in other studies analyzing risk factors for recurrence following the endoscopic treatment.15,16 In our study, only age was associated as an independent risk factor for recurrent stone development. In fact, age has been previously related to stone recurrence, and may be a factor for stone formation itself.15,37 From this point of view, choledocholithiasis seems to be a different disease in young and older patients. Whereas younger patients may have gallbladder migrated stones at diagnosis and maybe therefore cured by simple cholecystectomy and CBD stone extraction without recurrence, older patients that presents with choledocholithiasis may have a greater risk of new CBD stone development. Some kind of bile duct or papilla malfunction maybe present and simple bile duct clearance may not prevent recurrence. This may explain our results revealing that all patients with recurrent CBD stones were aged over 55 and most of them over 65. In this setting, optimal approach for choledocholithiasis management in older patient should be still clarified. Most studies comparing the endoscopic and surgical approach for choledocholithiasis management do not stratify the treatment strategy by age and few of them analyze long term results so as to determine stone recurrence. Whether an endoscopic sphincterotomy facilitating bile duct emptying, even if causing permanent biliary reflux, could be a better treatment option than only surgical stone extraction in aging patients in order to prevent recurrence, should be investigated.
Authorship / collaboratorsThe five authors contributed substantially to the design of the study, the acquisition of data and the subsequent analysis. The final work was also critically reviewed and the final version was approved by the five authors listed.
Conflict of InterestsThe authors declare that they have no conflicts of interest.
Please cite this article as: Parra-Membrives P, Martínez-Baena D, Lorente-Herce JM, Jiménez-Riera G, Sánchez-Gálvez MÁ. Recurrencia de coledocolitiasis tras exploración laparoscópica de la vía biliar principal. Cir Esp. 2019;97:336–342.