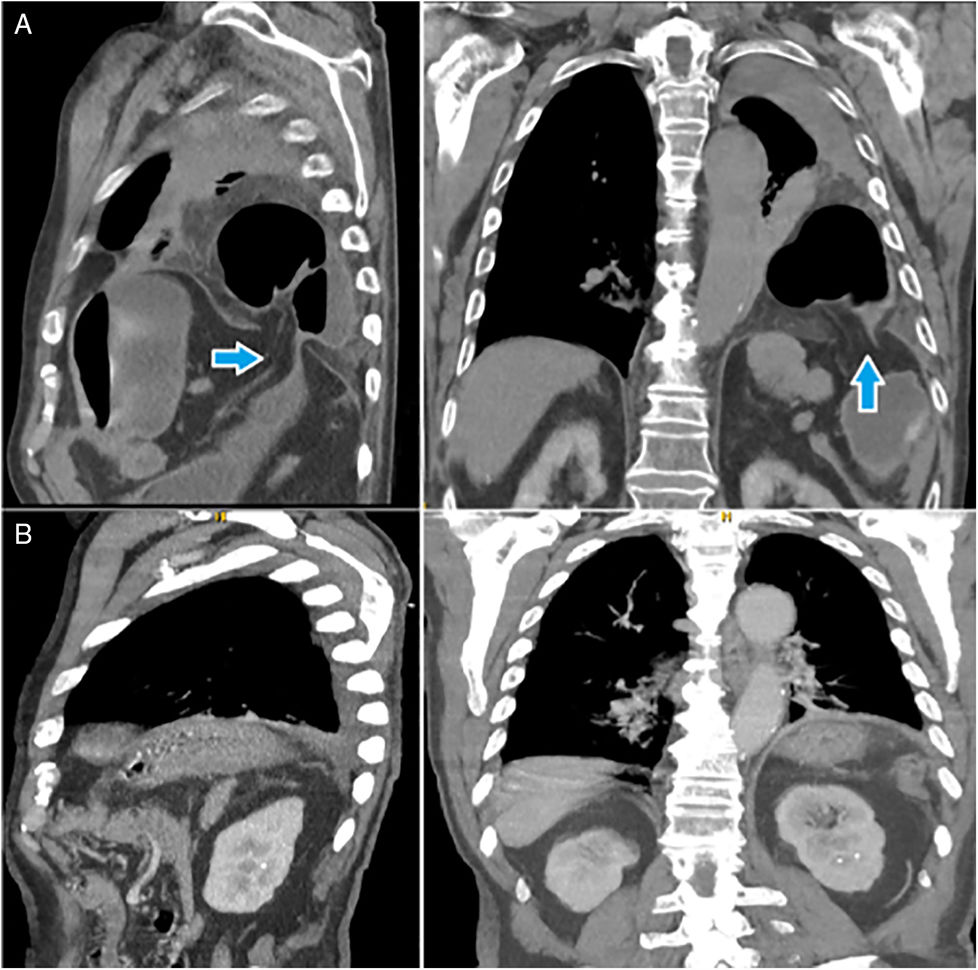
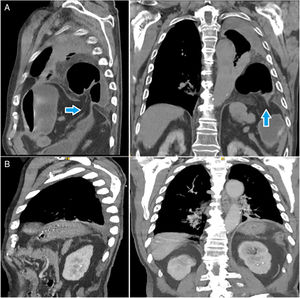
The patient is an 87-year-old man with a hearing impairment and no history of severe trauma, who came to the emergency department for severe abdominal pain, enteric vomiting and abdominal distension. On physical examination, he was afebrile, hemodynamically stable and presented guarding and a tympanitic left hypochondrium. The analysis showed leukocytosis (33400/L), left deviation and C-reactive protein: 226mg/L. Computed tomography (Fig. 1A) indicated urgent exploratory laparotomy, which confirmed the existence of a left diaphragmatic hernia located in the pars tendinosa. The hernia sac contained the splenic flexure of the colon, spleen, and greater omentum, causing symptoms of occlusion with proximal ischemia of the colon. We conducted subtotal colectomy, splenectomy, partial resection of the greater omentum, terminal ileostomy and closure of the diaphragmatic orifice. Postoperative morbidities included vomiting, confusion syndrome, and surgical site infection. The patient was discharged on the fifteenth day. Postoperative computed tomography was performed (Fig. 1B).
Please cite this article as: Díaz Candelas DA, de la Plaza Llamas R, Arteaga Peralta V, Ramia JM. Hernia diafragmática complicada. Cir Esp. 2020;98:238.