The aim of this narrative review is to define the clinical–pathological characteristics and to clarify the management of right colonic diverticular disease. It is rare in Europe, USA, and Australia and more common in Asia. In the recent years its incidence has increased in the West, with various distributions among populations. Many studies have reported that it is difficult to differentiate the presenting symptoms of this disease from those of appendicitis before surgery, because the signs and symptoms are similar, so misdiagnosis is not infrequent. With accurate imaging studies it is possible to reach a precise preoperative diagnosis, in order to assess an accurate treatment strategy. Currently the management of this disease is not well defined, no clear guidelines have been proposed and it is not known whether the guidelines for left colonic diverticular disease can also be applied for it. Several authors have stated that conservative management is the best approach, even in case of recurrence, and surgery should be indicated in selected cases.
El objetivo de esta revisión es definir las características clínico-patológicas y aclarar el tratamiento de la enfermedad diverticular del colon derecho. Es poco frecuente en Europa, Estados Unidos y Australia, y más común en Asia. Durante los últimos años, su incidencia ha aumentado en Occidente, con diferentes distribuciones entre poblaciones. Muchos estudios han mostrado que es difícil diferenciar antes de la cirugía los síntomas de presentación de esta enfermedad de los de la apendicitis, ya que los síntomas y signos son similares, por lo que no es infrecuente encontrarse con un diagnóstico incorrecto. Con estudios de diagnóstico por la imagen exactos es posible establecer un diagnóstico preoperatorio preciso a fin de evaluar una estrategia de tratamiento adecuada. Actualmente, el tratamiento de esta enfermedad no está bien definido, no se han propuesto recomendaciones claras y no se sabe si también se pueden aplicar las recomendaciones para la enfermedad diverticular del colon izquierdo. Varios autores han señalado que el tratamiento conservador es el mejor enfoque, incluso en caso de reincidencia, y que la cirugía solo estaría indicada en determinados casos.
Colonic diverticulosis is a disease characterized by the existence of multiple diverticula in the intestinal wall. If symptoms or complications arise, this is the onset of diverticular disease. The most frequent symptoms are abdominal pain, meteorism, and changes in normal bowel habits.1 Uncomplicated diverticular disease is defined as mild but frequent abdominal pain. Uncomplicated diverticular disease is frequently confused with other conditions, such as inflammatory bowel disease.2,3 Complications may sometimes be observed, including inflammation, bleeding, and perforation of the diverticula, all with different levels of severity. This situation is called diverticulitis and may be characterized by a chronic or acute course. The presentation of diverticulitis can range from mild abdominal pain with contained perforation to free perforation and acute peritonitis.1 Fortunately, 80%–85% of patients with diverticulosis remain asymptomatic and the symptoms are not always severe. Only a small percentage develops diverticulitis with severe symptomatic disease, which can cause complications. The development of this process is not well understood, although it is probably related to altered bowel motility and changes in the colonic microflora.4
Diverticular disease is more frequent in European, North American, and Australian (Western) populations, although its prevalence has also increased in Asia (Eastern countries)5 in recent years. In Western populations, it mainly affects the left colon, especially the sigmoid colon, whereas in Asians it primarily appears in the right colon.6 However, due to increased migration, right-sided diverticulitis (RSD) is being more frequently detected in the West.7 Although treatment parameters have been established for the management of left-sided diverticular disease (LSD),8 there are no clear recommendations for RSD. It is not clear whether it is possible to apply LSD recommendations to RSD.9 In addition, it is necessary to distinguish between two different clinical situations in diagnosis and treatment: right diverticular disease and cecal diverticulitis.
The objective of this review is to specifically study the epidemiology, clinical features, and therapeutic approach of RSD and cecal diverticulitis, which could improve the treatment of this disease.
MethodologyFor the purposes of the present study, 2 different authors carried out a bibliographic search using the keywords “right colon * diverticul *” in the PubMed database of articles published in English between 2000 and 2016. This present review has included 74 articles, 15 of which are mainly about RSD, and describes their general characteristics, clinical presentation, diagnosis, and treatment.
Epidemiology and PhysiopathologyRSD is a common disease in Asian countries, where 20% of patients with diverticular disease and 75% of cases of diverticulitis present right diverticulosis; meanwhile, in Western countries, RSD accounts for only 1%–2%.10 At the global level, the highest incidence of diverticular disease occurs in the West and affects 50% of the population over 60 years of age, with a prevalence of 15%–35%11,12 (90%–99% of cases affect the left colon13). The prevalence in Asia is 8%–25%,14,15 reaches a peak between 40 and 50 years, and affects the right colon in 70%–98% of cases.15,16
In Western countries, which are characterized by a heterogeneous population that has migrated from Eastern countries, the incidence of RSD could increase considerably in the future, which is an important factor. In fact, some authors have affirmed that there is a genetic predisposition to develop this disease.17 Some studies have informed that the incidence of RSD may increase in some Western populations, but none of the studies has shown a leveling in the incidence between immigrants and the native population.7,18 Faucheron et al. have reported a prevalence of RSD in France of 20% in the population over the age of 70, which demonstrates that its incidence in the West is not so rare.19 RSD is more frequent in the younger population, especially between the ages of 20 and 50,9 and in men.20
Two important clinical situations must be differentiated: diverticular disease located in the proximal colon and isolated diverticula of the right colon, often with a solitary cecal manifestation. If numerous, these lesions are usually acquired pseudodiverticula; if solitary, they are usually congenital and true diverticula. In the Asian population, true diverticula are abundant, especially in the right colon21 because of the congenital weakness of the intestinal wall. Although it was initially thought that right diverticula in Western populations were congenital and true compared to left diverticula, one study has revealed that, in the Western population, there may be pseudodiverticula even in the right colon. Thus, perhaps there is a different pathophysiology between diverticular disease in Eastern and Western populations.22
Certain factors are associated with this disease, such as a non-fiber diet or the absence of physical activity. In addition, genetic factors are involved in the pathogenesis, especially in RSD. In fact, cases of diverticular disease have been found in patients who are affected by genetic disorders, such as muscular diseases, colon abnormalities, connective tissue diseases or neurological abnormalities.23–27 Solitary congenital diverticula arise as a saccular projection during the sixth week of embryonic development.28 On rare occasions, angiodysplasia has been reported in association with solitary cecal diverticula.29 Radhi et al. have indicated that the existence of thick anomalous vessels causes hemodynamic or local pressure changes, perhaps the basis of a diverticular disease process.26 Another study has analyzed the morphology of the myenteric plexuses and ganglion cells and shows the differences between bowel segments. There were more plexuses in the colon segments with diverticula, but less ganglion cells than in the segments without diverticula.30 However, it is difficult to investigate these aspects due to the intense inflammation that exists in the case of true diverticula.26
Symptoms and DiagnosisAlthough it is still unclear whether the pathophysiology of RSD and LSD are different, their clinical histories are not the same.31 It is not easy to define a clear clinical presentation of RSD. Several authors have indicated that, in many instances, its presentation may be confused with appendicitis, especially in the acute phase with lower right abdominal pain and in the case of isolated cecal diverticulitis.22,32 In the article by Cristaudo et al., right abdominal pain was present in 84.6% of patients. The abdominal pain was similar to that of appendicitis, but nonspecific in description and longer in duration (from 5 to 7 days). The pain is often more cranial than McBurney's point and milder.7 Some studies have concluded that more than 70% of patients with cecal diverticulitis had undergone surgery with a preoperative diagnosis of appendicitis.33–35
This was a common situation years ago, when imaging techniques were not as advanced. In the evaluation of the clinical history, an adequate description is essential, particularly whether that patient has had diarrhea or not, which appears in only 18% of appendicitis cases.36 Other differences with appendicitis include low incidence of nausea, vomiting, and anorexia associated with abdominal pain, as well as the varying point of maximum sensitivity to palpation on abdominal examination.37 Other authors have indicated less systemic inflammatory response, nausea, and vomiting than appendicitis.38,39 According to Lee et al., symptoms that could be suggestive of cecal diverticulitis include leukocytosis and diarrhea, with no systemic signs, accompanied by lateralized pain in the lower right quadrant that migrates. These studies concur that RSD and cecal diverticulitis are difficult to differentiate from appendicitis, but there was generally less systemic inflammation, which could be an important differentiating factor. RSD could also be confused with other diseases, such as cholecystitis, gastritis or peptic ulcer, although less frequently.41 Another important symptom is bleeding, which is frequent in the case of RSD. The article by Faucheron et al. observed that 65.2% of patients admitted for diverticular hemorrhage had RSD. Therefore, the authors concluded that diverticula of the right colon are more likely to bleed, but the bleeding is more likely to stop spontaneously.19 One of the most important problems in these cases is recurrent bleeding, with an incidence of 10% during the first year and 50% within 10 years. In general, about 3%–15% of patients who are affected by colonic diverticulosis will present with gastrointestinal bleeding.42,43
Due to its peculiar clinical history, a correct diagnosis is essential to avoid unnecessary surgical interventions. Years ago, the diagnosis was often made intraoperatively, and an incorrect preoperative diagnoses of appendicitis was generally established in 50% of patients with RSD.34 After proper physical examination and blood work, which may not be sufficient for correct diagnosis, the first radiological study that is usually ordered is abdominal ultrasound, with a sensitivity of 75%–90% and a specificity of 86%–100% for the diagnosis of acute appendicitis.44 Some studies have reported the use of barium enema, but the risk of perforation must be considered, especially during the initial acute episode, so this diagnostic technique is currently not accepted.6,20,45 In contrast, ultrasound has several advantages as it is easily available, does not use X-rays and is found in all hospitals. When conducted by an experienced radiologist, this technique reaches a confirmed sensitivity of 99.8% and specificity of 91.3% for RSD.46,47 Another diagnostic imaging technique used in cases of suspected diverticulitis is computed tomography (CT). In some hospitals, it has become the diagnostic technique of choice in the case of diverticular disease or right abdominal pain with suspected appendicitis.32 It has been reported that CT scans have a specificity of 90%–95%, but in some cases it may establish an incorrect diagnosis and confuse RSD with an appendicular abscess, Crohn's disease, omental infarction, or colon cancer.46 Ultrasound and CT have some limitations. The reliability of ultrasound is variable and depends on the technician's experience. CT scanning uses ionizing radiation, which could be a contraindication for young or pregnant patients.48 For these reasons, the use of magnetic resonance imaging (MRI) has been proposed.
In a study by Cobben et al., MRI was used for the diagnosis of RSD. In the study, not one patient was misdiagnosed with right diverticulitis using MRI, so the authors concluded that MRI is a useful imaging technique for the diagnosis of RSD. Another factor to be considered is the possible existence of an underlying carcinoma, which may mimic the tomographic features of diverticulitis. Therefore, in uncertain cases, colonoscopy is indicated after the symptoms have disappeared.49
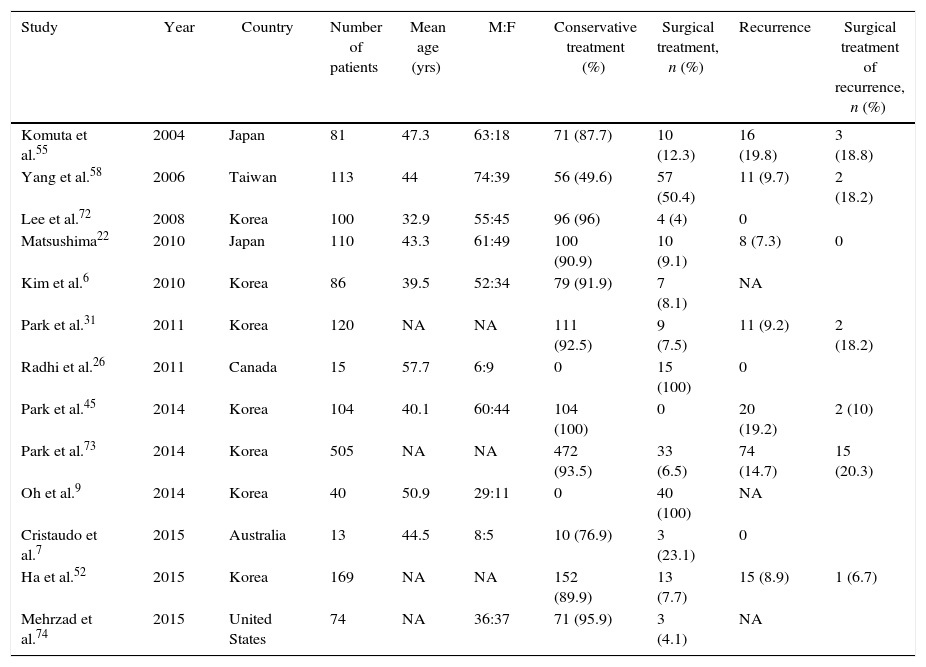
TreatmentTable 1 presents the results of the main recent studies about the treatment of patients with right-sided colon diverticulitis.
Main Recent Studies About the Treatment of Right Colonic Diverticulitis.
| Study | Year | Country | Number of patients | Mean age (yrs) | M:F | Conservative treatment (%) | Surgical treatment, n (%) | Recurrence | Surgical treatment of recurrence, n (%) |
|---|---|---|---|---|---|---|---|---|---|
| Komuta et al.55 | 2004 | Japan | 81 | 47.3 | 63:18 | 71 (87.7) | 10 (12.3) | 16 (19.8) | 3 (18.8) |
| Yang et al.58 | 2006 | Taiwan | 113 | 44 | 74:39 | 56 (49.6) | 57 (50.4) | 11 (9.7) | 2 (18.2) |
| Lee et al.72 | 2008 | Korea | 100 | 32.9 | 55:45 | 96 (96) | 4 (4) | 0 | |
| Matsushima22 | 2010 | Japan | 110 | 43.3 | 61:49 | 100 (90.9) | 10 (9.1) | 8 (7.3) | 0 |
| Kim et al.6 | 2010 | Korea | 86 | 39.5 | 52:34 | 79 (91.9) | 7 (8.1) | NA | |
| Park et al.31 | 2011 | Korea | 120 | NA | NA | 111 (92.5) | 9 (7.5) | 11 (9.2) | 2 (18.2) |
| Radhi et al.26 | 2011 | Canada | 15 | 57.7 | 6:9 | 0 | 15 (100) | 0 | |
| Park et al.45 | 2014 | Korea | 104 | 40.1 | 60:44 | 104 (100) | 0 | 20 (19.2) | 2 (10) |
| Park et al.73 | 2014 | Korea | 505 | NA | NA | 472 (93.5) | 33 (6.5) | 74 (14.7) | 15 (20.3) |
| Oh et al.9 | 2014 | Korea | 40 | 50.9 | 29:11 | 0 | 40 (100) | NA | |
| Cristaudo et al.7 | 2015 | Australia | 13 | 44.5 | 8:5 | 10 (76.9) | 3 (23.1) | 0 | |
| Ha et al.52 | 2015 | Korea | 169 | NA | NA | 152 (89.9) | 13 (7.7) | 15 (8.9) | 1 (6.7) |
| Mehrzad et al.74 | 2015 | United States | 74 | NA | 36:37 | 71 (95.9) | 3 (4.1) | NA |
NA, not available.
There are no established guidelines for the treatment of RSD, and current recommendations usually refer to the left colon.50,51 The incidence of complicated RSD during the first episode is low, and conservative treatment may be effective in cases of uncomplicated RSD.52 According to the recommendations of the American Society of Colon and Rectal Surgeons,8 the initial treatment of uncomplicated left diverticulitis is digestive rest and broad-spectrum antibiotics. RSD has been reported to have a low rate of complications, and recurrent cases could be managed with conservative treatment, although there are few data about specific aspects, such as the duration of antibiotic treatment or the frequency and type of follow-up, especially in uncomplicated cases.36,53 This is especially true in the case of cecal diverticulitis.7 The duration of treatment with intravenous antibiotics may vary and depends on the physician's preference and the patient's clinical condition; treatment can be administered in hospital or in the outpatient setting.
Acute symptoms usually last 2–4 days, so Park et al. proposed that these patients be given antibiotic therapy for at least 4 days, followed by oral antibiotics after discharge, when symptoms have diminished.31 Shug-Pass et al. also proposed this type of approach for patients without complications.54 Hospital management requires treatment with intravenous antibiotics. The most frequently used regimens are ampicillin (1g every 6h), metronidazole (500mg every 8h) plus gentamicin (4–7mg per kg). In patients with penicillin allergy, ceftriaxone may be considered. Subsequent outpatient treatment without digestive rest could be a useful option in uncomplicated patients. For outpatients, frequent treatments are amoxicillin and clavulanic acid (875mg/125mg) every 12 or 8h.7 Komuta et al. have indicated that this type of treatment could be useful both in the first episode of diverticulitis and in recurrence without complications.55 If the disease presents with gastrointestinal bleeding, the initial treatment is conservative, including hemodynamic support, since 75% of the episodes have spontaneous resolution. If bleeding continues, colonoscopy should be performed.39,40
Non-Conservative TreatmentWhen a complication occurs, such as a perforation or the formation of an abscess, or even if the endoscopy does not resolve the bleeding, the treatment cannot be conservative.39,40 A localized abscess can be drained percutaneously.56,57 It has been described that the complication rate of an episode of diverticulitis reaches 10%.58,59 In general, the complication rate in the first episode of RSD is very low, indicating a conservative approach as the appropriate treatment in most cases.52 It is not easy to standardize the treatment, because sometimes patients present severe symptoms that require resection during the first episode, and other times conservative treatment may be the best option even in cases of recurrent episodes.60,61 The problem is reinforced because this disease normally has a benign evolution and spontaneous resolution, while in some cases it may be fulminant. Although it is not frequent, if the disease presents with obvious perforation, or in the case of clinically unstable patients, urgent surgery is required.32
Surgical TreatmentFour main surgical strategies can be considered: appendectomy with postoperative antibiotic treatment, right hemicolectomy, diverticulectomy with appendectomy and ileocecal resection.62 Chiu et al. have treated 30 patients with unperforated right-side colonic diverticulitis with appendectomy and intravenous antibiotics without diverticulectomy, which has provided satisfactory results.63 Nonetheless, some authors advocate a more aggressive strategy and emphasize that the clinical history and evolution of this disease are still not well understood.
Right hemicolectomy could be the preferred option in the case of patients with frequent episodes and multiple diverticula in the right colon. In these cases, surgical resection continues to be the only manner that the symptoms are resolved and the disease is definitively cured.62
Another option is diverticulectomy, which is a less widespread procedure that could resolve the problem. However, it is not always easy to separate the diverticulum from the surrounding tissue, especially in cases of extensive inflammation, and sometimes it is not simple to resect and close the base of the diverticulum, which may be too extensive.64 Diverticulectomy seems to result in a lower rate of complications and a similar recurrence rate compared with right hemicolectomy, but it should be recommended only in cases with a solitary diverticulum or for intraoperative diagnoses.65 This is the best option in cases of complicated cecal diverticulitis.7
In cases with multiple diverticula, resection of a diverticulum does not resolve the disease, so right hemicolectomy or ileocecal resection should be considered.62 Likewise, these procedures make it possible to establish a precise histological diagnosis and appropriate treatment in cases with suspected malignancy, which should always be contemplated. In fact, it has been reported that the incidence of malignancy reaches 5.8% in these patients.66 Ileocecal resection can be a good treatment, but, if there is suspected malignancy, right hemicolectomy will be the best treatment to respect oncology principles.
Last of all, in patients affected by multiple diverticula of the right colon and recurrent gastrointestinal bleeding who require continuous transfusions, scheduled right hemicolectomy should be considered.39,40 The disadvantage of the surgical treatment is the higher rate of morbidity and mortality, as well as the changes caused by the elimination of the ileocecal valve. If surgery is necessary, especially in young patients, scheduled laparoscopic resection is preferable in order to minimize complications, both in situations of scheduled surgery as well as in emergencies.67,68
RecurrenceWe still do not fully understand the predisposing factors or recurrence rates for RSD. A recent article has reported a rate of recurrence of 19% and a rate of re-recurrence after the primary recurrence of 26%. Predisposing factors for recurrence identified by the authors include the number and diffusion of the diverticula. It was found that the recurrence rate was higher in patients with diverticula extended throughout the colon compared with those who had diverticula limited to the right colon. The existence of multiple diverticula significantly increased the risk for recurrence.45 Similar to LSD, in RSD scheduled resection could be recommended after 2 or more uncomplicated recurrences.8 The objective of scheduled surgery is to prevent recurrence or complication. However, the decision for surgery should be assessed case by case. In reality there are no data to support the hypothesis that scheduled colectomy reduces the incidence of urgent surgery or the mortality rate.69 Furthermore, no correlation has been reported between the number of recurrences and response to medical treatment in RSD. It is also worthy of mention that the recurrence rate for RSD is lower than LSD.33,70
Currently, the age and frequency of episodes are not the main factors that indicate surgical treatment, since recurrences requiring surgery are uncommon. However, scheduled surgery should considered when the frequency of the episodes interferes with the normal activities of the patients’ daily lives.71
ConclusionsIn short, in cases of uncomplicated cecal or right-side diverticulitis, it seems that non-surgical treatments are the best approach, even in cases of recurrence. In patients with complicated diverticulitis or two or more episodes of relapse that are resistant to medical treatment or suspected of malignancy, and in cases in which a precise differential diagnosis could not be established (especially in case of cecal diverticulitis), surgery should be considered. Laparoscopy is the best surgical approach, especially in young patients. More studies are needed, above all in Western countries, to determine the exact incidence of this disease and to define an accurate treatment.
Authorship/CollaborationFrancesco Ferrara: study design, data acquisition, analysis, and interpretations of the results, composition of the manuscript. Jesús Bollo and Eduardo M. Targarona: critical review and approval of the final version of the manuscript. Letizia V. Vanni: data acquisition and composition of the manuscript.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Ferrara F, Bollo J, Vanni LV, Targarona EM. Diagnóstico y tratamiento de la enfermedad diverticular del colon derecho: revisión de conjunto. Cir Esp. 2016;94:553–559.