The incidence of inflammatory bowel disease (IBD) is increasing in Spain but there is little information on the availability of multidisciplinary care. This study aims to assess surgeon's opinions on the current situation of surgery for IBD in Spain.
MethodsAn electronic closed survey was sent to members of the Spanish Association of Surgeons (AEC) from January to March 2015. This was a 52-item anonymised questionnaire with questions about how the treatment of IBD patients is organized in each center, the existence of specific units, the management strategy in IBD patients, and the opinion of colorectal, general and trainee surgeons about the surgical treatment of IBD in their center and in Spain.
ResultsOne hundred and ninety-two surgeons responded. Most participants work in tertiary hospitals (45%), most of them from different hospitals, some from the same hospital. Only 50% of hospitals have multidisciplinary teams for IBD. The initial approach is laparoscopic in 56% of cases, and 80% of participants in centers with multidisciplinary teams consider the timing of surgery to be appropriate. The annual number of IBD surgeries in tertiary hospitals is higher than in secondary hospitals in ulcerative colitis (57% vs 24% 10–15 patients/year, P<.001) and Crohn's disease (68% vs 28% 3–5 patients/month, P<.001). Most centers operate less than 10 ulcerative colitis patients per year, even larger centers (67%) and they perform ≤3J-pouches/month (ulcerative colitis and other indications) (P<.001). Ninety-five percent of surgeons consider that centralization of complex cases in specialized units and the creation of national registries should be developed. The majority of participants (70%) believe that there is a deficit in research and educational activities in IBD surgery in Spain.
ConclusionThis survey suggests that most Spanish hospitals have a low volume of IBD surgery, even large tertiary hospitals, and many centers do not have a multidisciplinary team dedicated to IBD patients. Most survey participants believe it is necessary to develop registries and increase training and research in IBD surgery in Spain.
La incidencia de la enfermedad inflamatoria intestinal (EII) está aumentando en España, pero existe poca información sobre su abordaje multidisciplinar, en particular sobre su manejo quirúrgico. El objetivo de este estudio es evaluar la opinión de los cirujanos españoles sobre la situación actual de la cirugía de la EII en nuestro país.
MétodosSe realizó un estudio descriptivo del tipo encuesta cerrada que se envió a través de correo electrónico a los miembros de la Asociación Española de Cirujanos (AEC) durante los meses de enero a marzo de 2015. El cuestionario constaba de 52 ítems con preguntas sobre estructura y proceso, sobre el tratamiento quirúrgico y sobre la opinión de los cirujanos acerca de la calidad, satisfacción e investigación sobre la EII en su centro y en España.
ResultadosUn total de 192 cirujanos respondieron a la encuesta, la mayoría procedentes de hospitales de tercer nivel (45%), la mayoría de diferentes hospitales, algunos del mismo centro. Solo el 48,5% de los hospitales tienen equipos multidisciplinares de EII. El planteamiento quirúrgico inicial es laparoscópico en el 56,1% de los casos y el 80% de los participantes en los centros con equipos multidisciplinares considera el timing apropiado. El número de intervenciones anuales de EII en hospitales de tercer nivel es más alto que en hospitales de segundo nivel tanto en colitis ulcerosa (57 vs 24% operan 10-15 pacientes/año, p < 0,001) como en enfermedad de Crohn (68 vs 28% operan 3-5 pacientes/mes, p < 0,001). La mayoría de los centros, incluso los grandes hospitales, operan a menos de 10 pacientes con colitis ulcerosa al año y realizan ≤3 reservorios en J o pouch al año (por colitis ulcerosa y otras indicaciones) (p < 0,001). El 95% de los cirujanos considera que debe promoverse la centralización de casos complejos en unidades especializadas y la creación de registros nacionales.
ConclusionesSegún esta encuesta, parece que el volumen de cirugías de EII en España por centro no es elevado, ni siquiera en grandes hospitales, y muchos centros no cuentan con un equipo multidisciplinar de EII. No existen protocolos claros de derivación quirúrgica a centros de referencia o especializados. La mayoría de los participantes creen necesario el desarrollo de registros y aumentar la formación y la investigación en la cirugía de la EII en nuestro país.
Chronic inflammatory bowel disease (IBD) is a recurrent disease requiring long-term treatment for both intestinal and extraintestinal manifestations, including psychological ones. Crohn's disease (CD) and ulcerative colitis (UC) have a substantial impact on the physical health, social development, and quality of life of patients.1–3 In their lifetimes, about 20% of patients with UC will require surgery, and up to 80% of individuals with CD will be treated with some type of surgical intervention.2–9
In chronic diseases such as IBD, long-term outcomes can be substantially improved through the implementation of disease management programs. The multidisciplinary treatment of these patients by specialized professionals has been shown to reduce morbidity, need for surgery, and even mortality in patients with IBD.10–13 A recent consensus led by Spanish gastroenterologists2 determined that a specialized IBD unit should include at least: nursing staff specialized in IBD, gastroenterologists, radiologists, surgeons, endoscopists and stomal therapists. These multidisciplinary teams (MDT) should be able to offer individualized treatment, both during hospitalization and on an outpatient basis, without breaking the continuity of care. However, there is little information on the actual application of these units in Spain. Several multicenter studies have been conducted in other countries on the surgical management of IBD,13 and data on medical treatment and quality of life perceived by the patient have been published in our country.14–17 To date, no studies have been published on the surgical treatment of IBD in Spain.
A recent consensus led by Spanish gastroenterologists2 determined that a specialized IBD unit should include at least: nursing staff specialized in IBD, gastroenterologists, radiologists, surgeons, endoscopists and stomal therapists. These multidisciplinary teams (MDT) should be able to offer individualized treatment, both during the hospitalization period and on an outpatient basis, without breaking the continuity of care. However, there is little information on the actual application of these units in Spain. Several multicenter studies have been conducted in other countries about the surgical management of IBD,13 and in our setting data have been published about the medical treatment and quality of life perceived by the patient.14–17 To date, no studies have been published on the surgical treatment of IBD in Spain.
The main objective of this study is to determine the opinion of Spanish surgeons on the reality of surgical treatment for IBD in Spain and its management from a structural and organizational point of view. Other objectives include a description of the most common surgical procedures, and resources available to patients and surgeons interested in IBD.
MethodsA descriptive study of a closed survey type was designed and sent via email to request the participation of the members of the Spanish Association of Surgeons (AEC) from January to March 2015.
For the preparation of the survey, a form was used from this website: https://www.google.es/intl/es/forms.
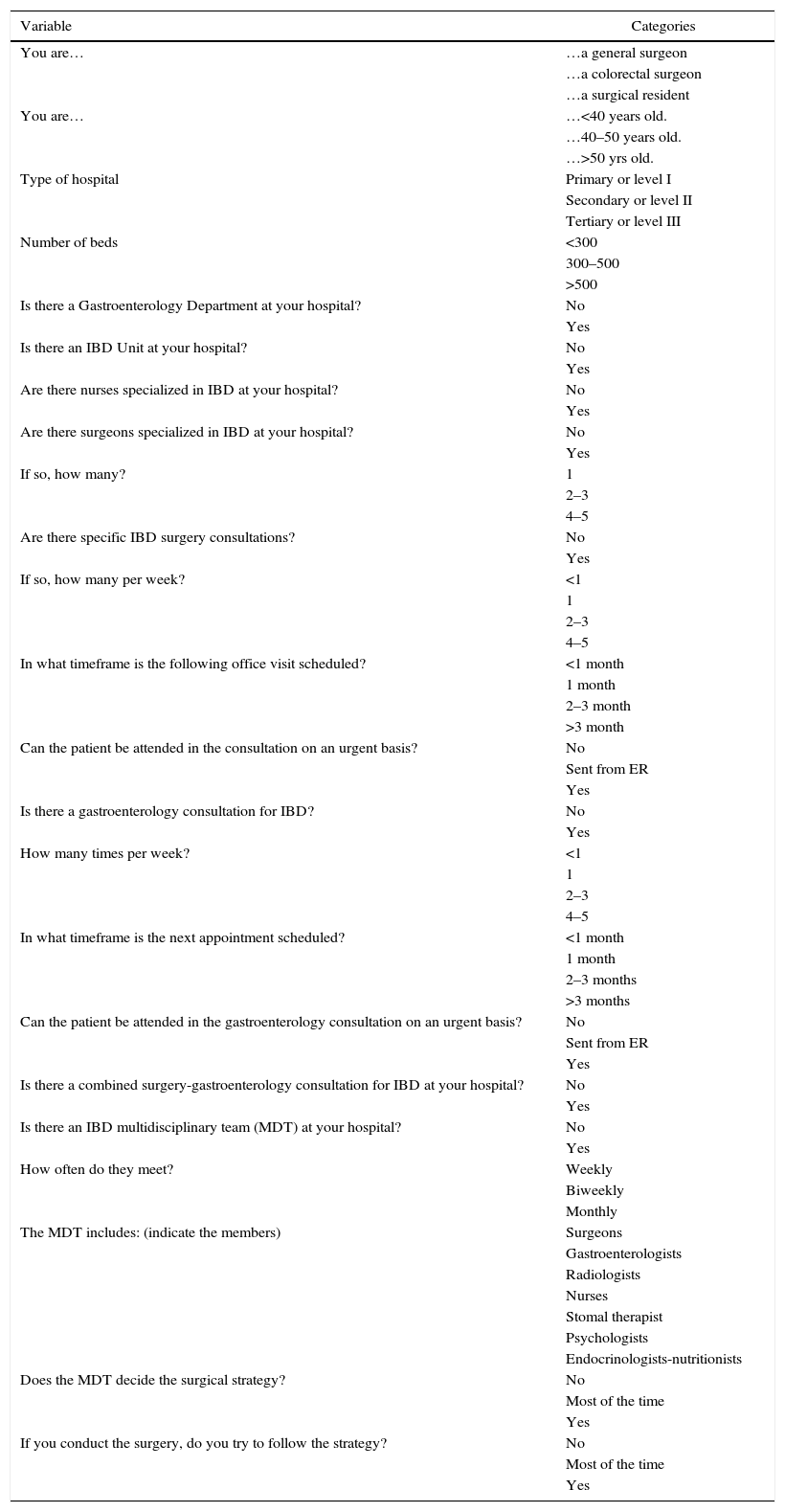
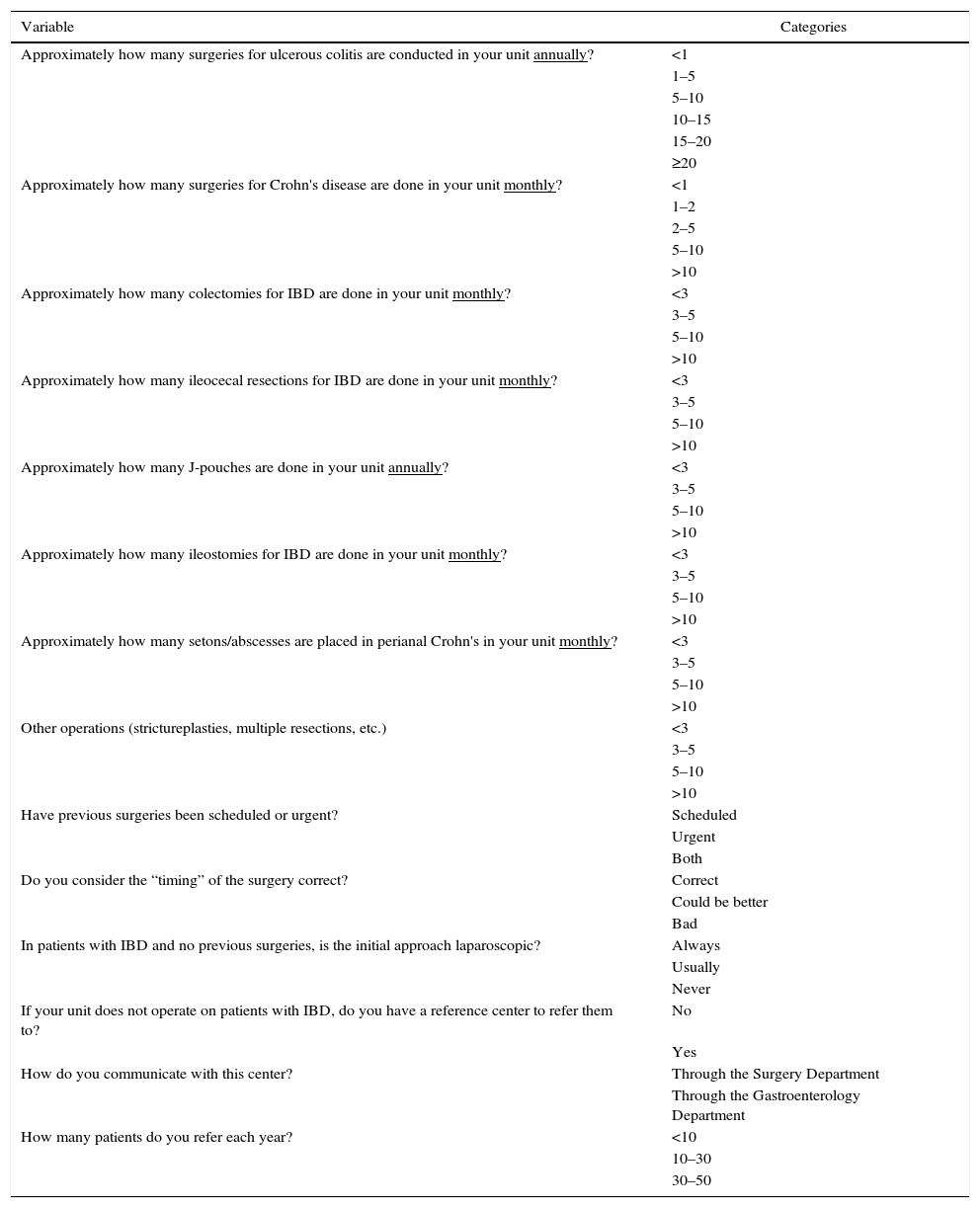
The survey consisted of a questionnaire with 52 items: 23 are compiled in Table 1 with questions on structure and process, the organization of IBD patient treatment at each hospital, multidisciplinary management and continuity of care; and, 29 items are shown in Tables 2 and 3, which are about surgical treatment and surgeon opinion on quality, satisfaction and research on IBD at his/her hospital and in Spain. Colorectal surgeons were considered those who belong to a Specialized Colorectal Surgery Unit within a General Surgery and Digestive System Department, since there is no recognized, certified coloproctology training program in our country today. Those who do not belong to a Coloproctology Unit were considered general surgeons. The surgeons in training were residents of General Surgery and the Digestive System of any year. Hospitals were divided into 3 groups: first level or level I hospitals (without an Intensive Care Unit), second level or level II hospitals (without subspecialty referral units) and third level or level III hospitals (with specialized reference units).
Survey Sent to the Participants to Evaluate the Configuration of the IBD Units in Spain.
| Variable | Categories |
|---|---|
| You are… | …a general surgeon |
| …a colorectal surgeon | |
| …a surgical resident | |
| You are… | …<40 years old. |
| …40–50 years old. | |
| …>50 yrs old. | |
| Type of hospital | Primary or level I |
| Secondary or level II | |
| Tertiary or level III | |
| Number of beds | <300 |
| 300–500 | |
| >500 | |
| Is there a Gastroenterology Department at your hospital? | No |
| Yes | |
| Is there an IBD Unit at your hospital? | No |
| Yes | |
| Are there nurses specialized in IBD at your hospital? | No |
| Yes | |
| Are there surgeons specialized in IBD at your hospital? | No |
| Yes | |
| If so, how many? | 1 |
| 2–3 | |
| 4–5 | |
| Are there specific IBD surgery consultations? | No |
| Yes | |
| If so, how many per week? | <1 |
| 1 | |
| 2–3 | |
| 4–5 | |
| In what timeframe is the following office visit scheduled? | <1 month |
| 1 month | |
| 2–3 month | |
| >3 month | |
| Can the patient be attended in the consultation on an urgent basis? | No |
| Sent from ER | |
| Yes | |
| Is there a gastroenterology consultation for IBD? | No |
| Yes | |
| How many times per week? | <1 |
| 1 | |
| 2–3 | |
| 4–5 | |
| In what timeframe is the next appointment scheduled? | <1 month |
| 1 month | |
| 2–3 months | |
| >3 months | |
| Can the patient be attended in the gastroenterology consultation on an urgent basis? | No |
| Sent from ER | |
| Yes | |
| Is there a combined surgery-gastroenterology consultation for IBD at your hospital? | No |
| Yes | |
| Is there an IBD multidisciplinary team (MDT) at your hospital? | No |
| Yes | |
| How often do they meet? | Weekly |
| Biweekly | |
| Monthly | |
| The MDT includes: (indicate the members) | Surgeons |
| Gastroenterologists | |
| Radiologists | |
| Nurses | |
| Stomal therapist | |
| Psychologists | |
| Endocrinologists-nutritionists | |
| Does the MDT decide the surgical strategy? | No |
| Most of the time | |
| Yes | |
| If you conduct the surgery, do you try to follow the strategy? | No |
| Most of the time | |
| Yes |
IBD: inflammatory bowel disease.
Survey Sent to the Participants to Evaluate the Number of IBD Surgeries in Spain.
| Variable | Categories |
|---|---|
| Approximately how many surgeries for ulcerous colitis are conducted in your unit annually? | <1 |
| 1–5 | |
| 5–10 | |
| 10–15 | |
| 15–20 | |
| ≥20 | |
| Approximately how many surgeries for Crohn's disease are done in your unit monthly? | <1 |
| 1–2 | |
| 2–5 | |
| 5–10 | |
| >10 | |
| Approximately how many colectomies for IBD are done in your unit monthly? | <3 |
| 3–5 | |
| 5–10 | |
| >10 | |
| Approximately how many ileocecal resections for IBD are done in your unit monthly? | <3 |
| 3–5 | |
| 5–10 | |
| >10 | |
| Approximately how many J-pouches are done in your unit annually? | <3 |
| 3–5 | |
| 5–10 | |
| >10 | |
| Approximately how many ileostomies for IBD are done in your unit monthly? | <3 |
| 3–5 | |
| 5–10 | |
| >10 | |
| Approximately how many setons/abscesses are placed in perianal Crohn's in your unit monthly? | <3 |
| 3–5 | |
| 5–10 | |
| >10 | |
| Other operations (strictureplasties, multiple resections, etc.) | <3 |
| 3–5 | |
| 5–10 | |
| >10 | |
| Have previous surgeries been scheduled or urgent? | Scheduled |
| Urgent | |
| Both | |
| Do you consider the “timing” of the surgery correct? | Correct |
| Could be better | |
| Bad | |
| In patients with IBD and no previous surgeries, is the initial approach laparoscopic? | Always |
| Usually | |
| Never | |
| If your unit does not operate on patients with IBD, do you have a reference center to refer them to? | No |
| Yes | |
| How do you communicate with this center? | Through the Surgery Department |
| Through the Gastroenterology Department | |
| How many patients do you refer each year? | <10 |
| 10–30 | |
| 30–50 |
IBD: inflammatory bowel disease.
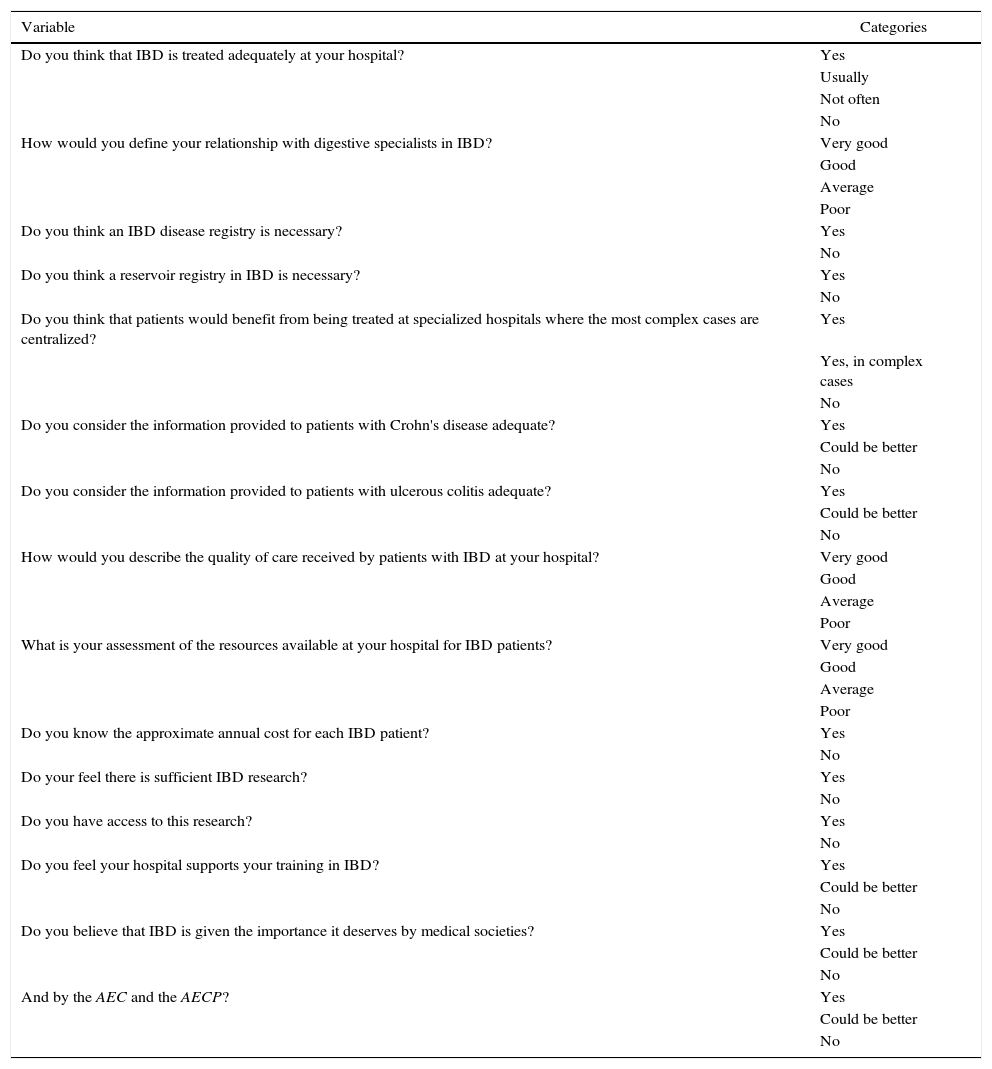
Questionnaire Sent to the Participants to Evaluate the Opinion of the Surgeons About IBD Surgery in Spain.
| Variable | Categories |
|---|---|
| Do you think that IBD is treated adequately at your hospital? | Yes |
| Usually | |
| Not often | |
| No | |
| How would you define your relationship with digestive specialists in IBD? | Very good |
| Good | |
| Average | |
| Poor | |
| Do you think an IBD disease registry is necessary? | Yes |
| No | |
| Do you think a reservoir registry in IBD is necessary? | Yes |
| No | |
| Do you think that patients would benefit from being treated at specialized hospitals where the most complex cases are centralized? | Yes |
| Yes, in complex cases | |
| No | |
| Do you consider the information provided to patients with Crohn's disease adequate? | Yes |
| Could be better | |
| No | |
| Do you consider the information provided to patients with ulcerous colitis adequate? | Yes |
| Could be better | |
| No | |
| How would you describe the quality of care received by patients with IBD at your hospital? | Very good |
| Good | |
| Average | |
| Poor | |
| What is your assessment of the resources available at your hospital for IBD patients? | Very good |
| Good | |
| Average | |
| Poor | |
| Do you know the approximate annual cost for each IBD patient? | Yes |
| No | |
| Do your feel there is sufficient IBD research? | Yes |
| No | |
| Do you have access to this research? | Yes |
| No | |
| Do you feel your hospital supports your training in IBD? | Yes |
| Could be better | |
| No | |
| Do you believe that IBD is given the importance it deserves by medical societies? | Yes |
| Could be better | |
| No | |
| And by the AEC and the AECP? | Yes |
| Could be better | |
| No |
AEC: Spanish Association of Surgeons; AECP: Spanish Association for Coloproctology; IBD: inflammatory bowel disease.
The differences in the responses were evaluated with the two-tailed Fisher's exact test for the categorical variables, using SPSS version 19.0 software (SPSS, Inc., Chicago, IL, USA).
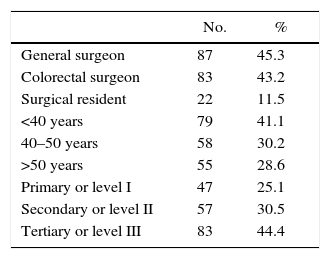
ResultsA total of 192 surgeons answered the questionnaire, which was sent to the AEC members’ e-mail addresses on record and included surgeons from all surgical subspecialties (4950 members in total, 630 in the coloproctology division). The study was completed by 100% of the participants who had started it. The first response was received on January 28, 2015 and the last on April 6, 2015, although the survey remained open until April 15, 2015.
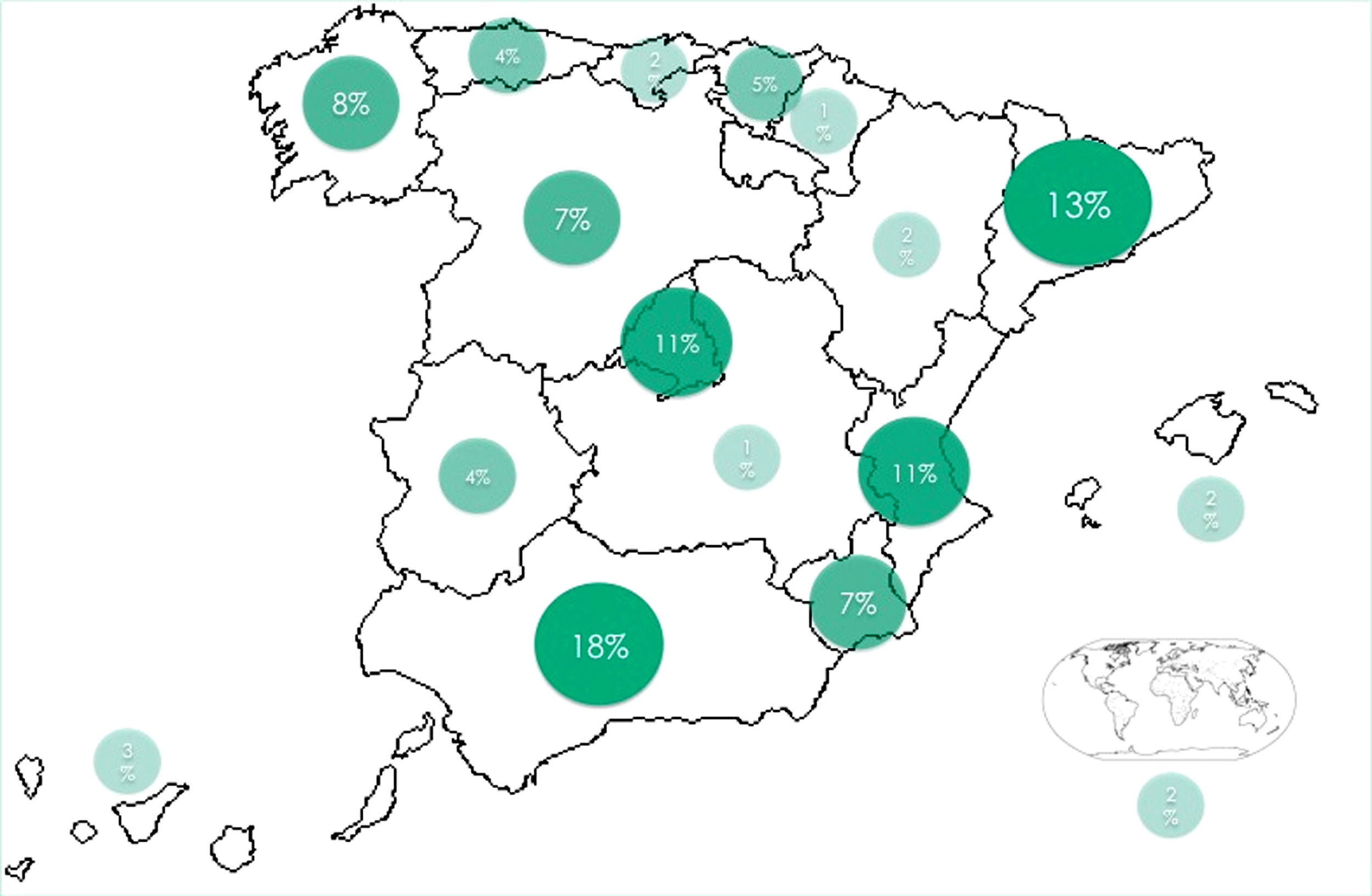
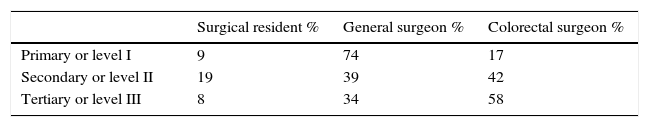
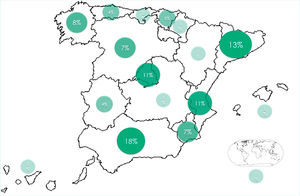
The demographic data of the participants are shown in Tables 4 and 5, and the geographical distribution by Autonomous Communities are in Fig. 1. Most of the respondents were general surgeons (45.3%) or colorectal surgeons (43.2%) from third-level hospitals (44.5%) with more than 500 beds. Although the survey was anonymous, the data reflected that most surgeons belonged to different hospitals. In those cases where the province and the type of hospital coincided, a correlation was found in the responses of 85%. Most hospitals had a Gastroenterology Department (96.2%) with endoscopists, and in 78.1% there were one or more specific IBD consultations, although only 32.4% had a dedicated IBD nurse. The scheduled patient follow-up at these consultations was variable (36.2% monthly, 35.1% every 2–3 months).
The responses revealed that 42% of hospitals did not have a specific IBD surgeon, and only 19.9% of hospitals had a specific surgery consultation for IBD. As for the frequency of follow-up, 34.7% of the surgeons routinely scheduled follow-up of these patients every 2–3 months, and 17.3% at longer intervals.
Nearly half of the hospitals (48.5%) did not have an IBD MDT. Hospitals that did have MDT meetings most frequently met monthly (23.1%). In 50.9%, surgical strategies were decided upon during these meetings, and, in 77.4% of the cases, this consensual strategy was maintained during surgery.
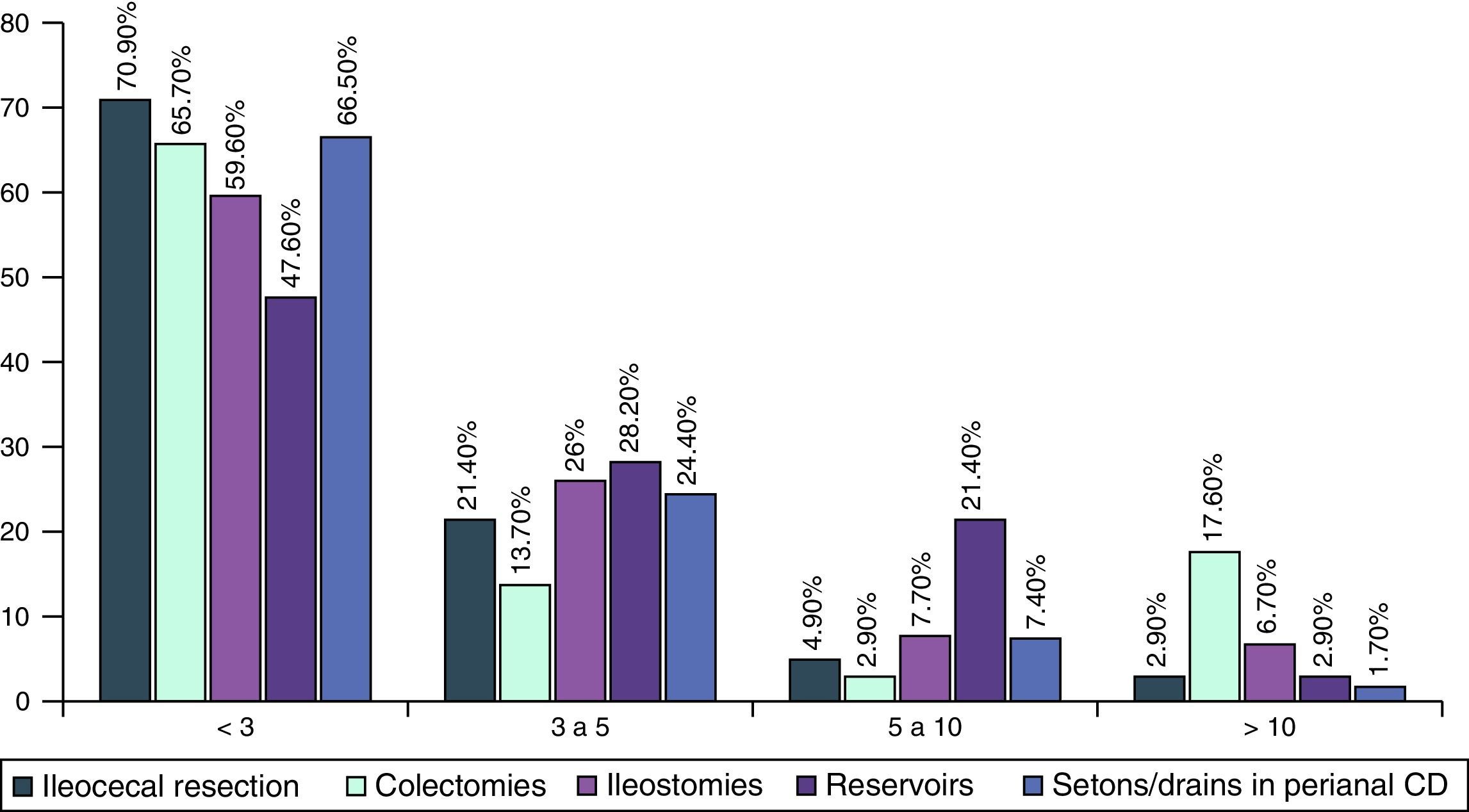
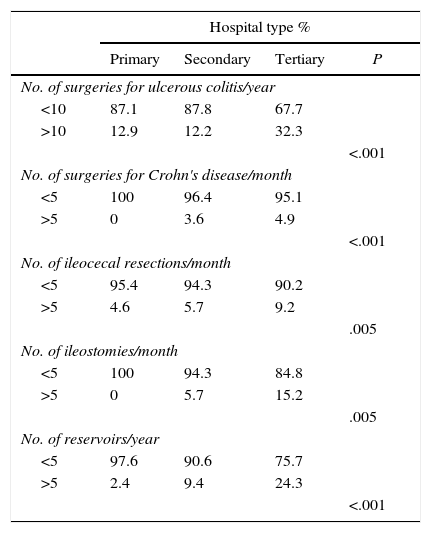
In CD surgeries, there was a significant difference between level III and II hospitals in the number of monthly surgeries (4.9% vs 3.6% performed ≥5 CD surgeries per month, P<.001). There were also significant differences in the number of surgeries between level I and level III hospitals for ileocecal resections in CD, colectomies and ileostomies (Table 6).
Differences in the Number of Procedures According to Hospital Type.
| Hospital type % | ||||
|---|---|---|---|---|
| Primary | Secondary | Tertiary | P | |
| No. of surgeries for ulcerous colitis/year | ||||
| <10 | 87.1 | 87.8 | 67.7 | |
| >10 | 12.9 | 12.2 | 32.3 | |
| <.001 | ||||
| No. of surgeries for Crohn's disease/month | ||||
| <5 | 100 | 96.4 | 95.1 | |
| >5 | 0 | 3.6 | 4.9 | |
| <.001 | ||||
| No. of ileocecal resections/month | ||||
| <5 | 95.4 | 94.3 | 90.2 | |
| >5 | 4.6 | 5.7 | 9.2 | |
| .005 | ||||
| No. of ileostomies/month | ||||
| <5 | 100 | 94.3 | 84.8 | |
| >5 | 0 | 5.7 | 15.2 | |
| .005 | ||||
| No. of reservoirs/year | ||||
| <5 | 97.6 | 90.6 | 75.7 | |
| >5 | 2.4 | 9.4 | 24.3 | |
| <.001 | ||||
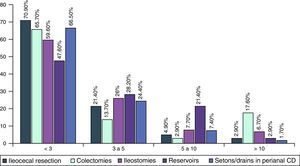
82% of surgeons reported performing fewer than 3 CD procedures per month. Even when we analyzed the hospitals with surgeons dedicated to IBD, the number of procedures was low (Fig. 2).
As for the procedures performed in patients with UC, the majority of medical centers operated on less than 10 patients with UC per year, even at the larger hospitals (67.7%). There was a significant difference between the level III and II hospitals in the annual number of UC surgeries (32.3% vs 12%, P<.0001) when more than 10 UC surgeries were performed per year (Table 6).
Fewer than 3J or pouch reservoirs were conducted annually by 45% of third-level hospitals, with significant differences between level II and level III hospitals (75.5% vs 44.9%; P<.001 in <3 reservoirs per year) (Table 6).
An initial laparoscopic surgical approach was more frequent in level III hospitals than in level I hospitals (85% usually or always vs 69.7%, although the differences were not significant: P=.166), as was the tendency to schedule surgery for IBD patients (39.5% vs 31.7% in first-level hospitals, where these procedures are performed more commonly by general surgeons and urgently).
The vast majority of surgeons at level I and level II hospitals had a reference IBD unit at a nearby third-level hospital (84.2% vs 55.2%, P<.001); however, the annual number of referred patients was low (less than 10 patients, 81.3% of primary hospitals and 94.4% of secondary hospitals).
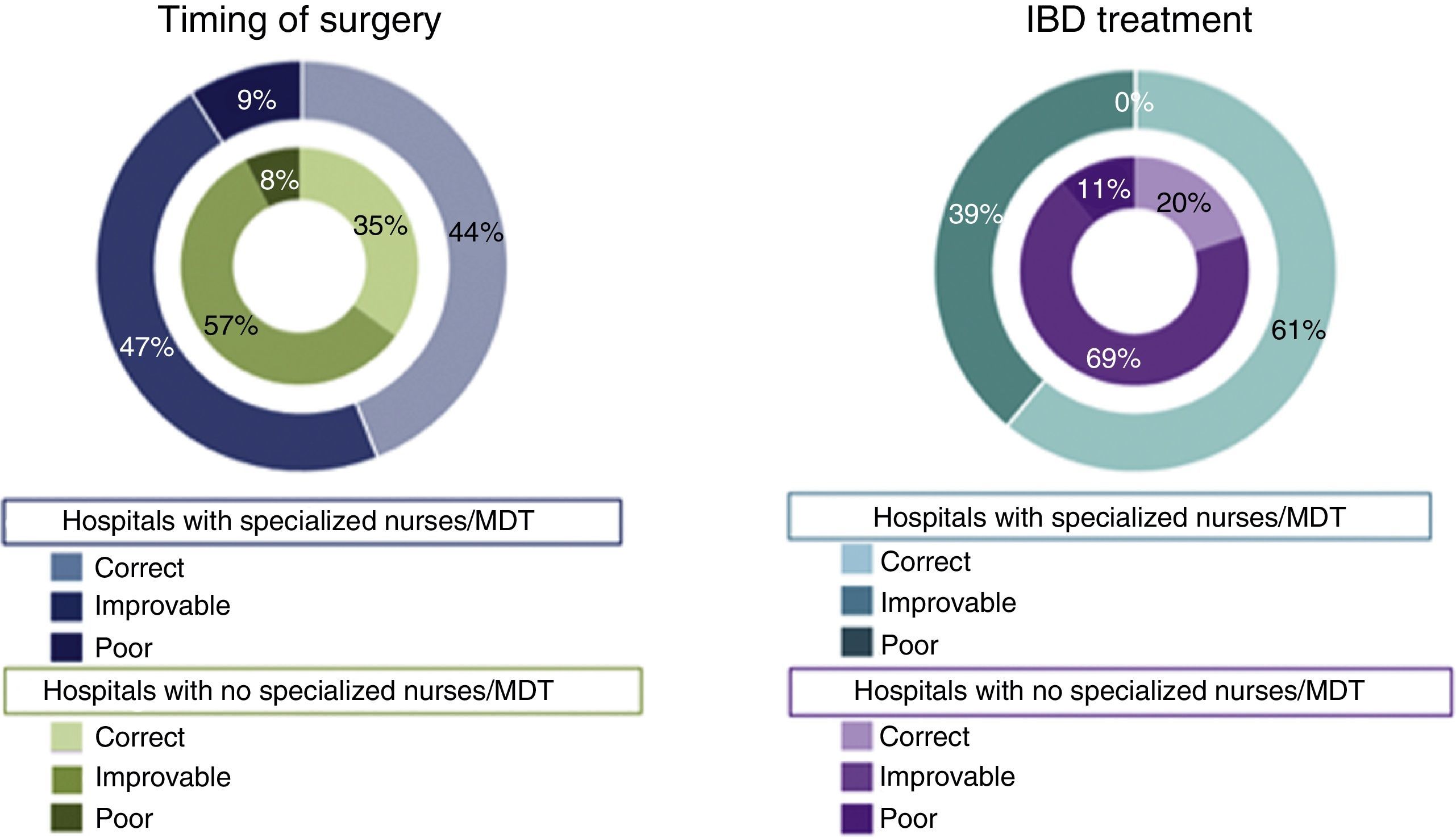
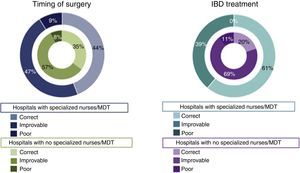
With regards to the opinion of surgeons on the quality of IBD treatment, we found significant differences. In centers with an MDT, 60.4% of surgeons believed that the treatment of IBD was appropriate, compared to only 20.2% in centers without an MDT (P<.001). There were also differences of opinion among the surgeons who worked at a hospital with specialized IBD nursing staff vs hospitals without it (61.4% vs 30.6%, P=.001, considered treatment correct) (Fig. 3).
Of the 192 respondents, 90 (52.3%) considered that the timing of the surgery could be improved: in hospitals with an MDT, 44% considered it appropriate compared to 35% in hospitals without an MDT (P<.001) (Fig. 3). 53.8% believed that patients would benefit from treatment at specialized medical centers, although 47.8% considered it necessary only in complex cases.
Almost all (94%) of the respondents agreed that national registries for IBD surgery are necessary, and 89% considered it to be especially important for ileoanal reservoirs.
On the other hand, most participants considered that the current health care provided to patients with IBD was adequate, but only 24.6% considered it to be very good. 47% believed that information for patients with IBD could improve. Most surgeons (85.2%) believed that their relationship with gastroenterologists was “good” or “very good”, but 88.6% did not know the annual cost of care for IBD patients.
The majority of surgeons (59.3%) thought that research in IBD surgery and educational activities are insufficient in Spain, and almost 70% do not have access to IBD research or other activities. Some 74% believe that Spanish scientific societies should increase surgical research and training activities in the surgical treatment of IBD.
DiscussionThis study shows that, in a survey of 192 surgeons, the general opinion is that IBD surgery in Spain could be improved. According to the respondents, less than half of Spanish hospitals (48.5%) have an MDT dedicated to IBD. The number of surgical procedures conducted at most hospitals is low and does not appear to be concentrated at specialized centers. Most surgeons agree with the need for developing surgical registries and for increasing research and training in IBD surgery.
Only 42.2% of Spanish hospitals have surgeons who are specially dedicated to patients with IBD. Several studies from other countries have demonstrated the importance of close, structured integration of medical and surgical treatment to determine the appropriate time for surgery and prevent postoperative complications.19,20 In the UK, the “IBD Standards Group” recommends that the surgery be performed by an experienced colorectal surgeon who specializes in IBD.20 It also recommends structured interaction between the gastroenterologist and the colorectal surgeon, and proposes that they have parallel or joint medical-surgical consultations in an IBD Unit. We have detected that, in Spain, there are very few specific surgical consultations for patients with IBD (19.2%) and that there are combined medical-surgical consultations in 14.2% of hospitals. Patient follow-up is variable: 2–3 months after intervention (34.7%) or within one month (20%), with no clear follow-up strategy. This finding is markedly different from treatment in the gastroenterology unit, with clear follow-up algorithms.21–23
There are a significant number of participating surgeons (48.5%) who do not have an MDT at their hospital. This demonstrates the lack of consensus and combined approach in these diseases at many Spanish hospitals, even though it has been shown that patient outcomes improve when they are treated by an MDI specialized in IBD.24 The recent recommendations of the European Crohn's and Colitis Organization (ECCO) establish the criteria for multidisciplinary units and the role of the surgeon as the main member of the team.5 In Spain, at hospitals that have an IBD MDT, monthly meetings are generally held, and surgical strategies are usually defined at these sessions. The ECCO guidelines also highlight the value of specialized IBD nurses, who provide these patients with better management and physical, emotional and educational support.18 The number of nurses specialized in IBD in Spain is low (32.4%) and quite far from the 62% recently reported in Europe.5
Wide variability is observed among the different hospitals in the volume of procedures, and there are very few with a high volume of surgeries, even third-level hospitals with more than 500 beds. 77% of the respondents perform less than 3 ileocecal resections per month, and 65.1% perform less than 3 ileoanal reservoirs per year (for UC as well as other indications). Although other factors are involved,25 there is a correlation between a higher rate of postoperative morbidity and longer hospitalization in hospitals with a lower volume of IBD surgery.19,26 IBD surgery can be very complex, and several studies have shown better results when performed by experienced surgeons, especially when dealing with complications in very specific procedures, such as ileoanal reservoirs.20 This survey shows that very few centers refer patients to more specialized hospitals and, although most of the smaller hospitals have a reference center, only 13.3% send more than 10 patients per year. Most surgical procedures are done at hospitals with a low volume of IBD surgeries.
The surgeons who responded to the survey most likely have a specific interest in IBD. When the survey was sent electronically to the e-mail addresses registered with the AEC, it is not known with certainty how many members actually received the document. Given the maximum number of possible recipients, the low response rate (15.5% of all AEC members and 30.5% of coloproctology division members) could have led to a degree of selection bias, whose magnitude is unquantifiable. The highest response rate was obtained from surgeons at level III hospitals (responses were received from 49 of the 78 third-level hospitals in Spain27) who were under the age of 50. Although the survey was anonymous, when we consider the respondents’ hospitals of origin (44.4% of third-level hospitals), it can be assumed that the majority are surgeons interested in IBD.
The creation of certified IBD reference units is the current challenge we face in the treatment of these patients. Although there is still a lack of evidence to establish the optimization of IBD units, particularly with regard to the composition of MDT, resources, training, documentation and patient support, a recent Spanish study has proposed minimum requirements for IBD units.2 In Spain, some hospitals may not have the resources to meet this ideal, and the authors propose that several hospitals should work together to improve the availability of specific resources.2 According to our study, 53.8% believe that patients would benefit from treatment at specialized centers, especially in complex cases, but the overall number of patients per year is low. These issues require further research and consensus.
As far as we are aware, this study is the first to evaluate the opinion of Spanish surgeons on the state of IBD surgery in Spain. It has been observed that the number and type of procedures performed in our country to treat IBD vary greatly from hospital to hospital, and there is a lack of guidelines for surgical treatment and specific training in IBD surgery compared to other European medical centers.5 The present study indicates the need to develop strategies to standardize surgical procedures and create registries in Spain, as well as to promote research and surgical training in IBD surgery. It is clear that there is much room for improvement in the quality of care that surgeons offer patients with IBD in our country, and this survey could be the basis for the creation of prospective studies and registries on IBD surgery in Spain.
Conflict of InterestsThe authors have no conflict of interest to declare related to the present study.
The authors would like to thank the Spanish Association of Surgeons (AEC) and the Spanish Association of Coloproctology (AECP) for their support of this initiative. We would also like to thank all the surgeons who participated in the survey, and especially Dr. José Luis Ramos for his assistance in the electronic mailing of the survey.
Please cite this article as: Sánchez-Guillén L, Blanco-Antona F, Millán-Scheiding M. Estado de la cirugía de la enfermedad inflamatoria en España. Resultado de una encuesta nacional. Cir Esp. 2016;94:560–568.
Presented as an oral communication at the ESCP Annual Meeting, Dublin, September 23–25, 2015.