Donor lung preservation at 10 °C appears to be an innovative and promising method that may improve transplant logistics by extending the cold ischemia time with excellent outcomes. We report the case of two lung transplants from two different donors involving the use of two different preservation methods, highlighting the benefits of using 10 °C lung storage.
La preservación pulmonar a 10 °C es una estrategia innovadora que podría mejorar la logística del trasplante pulmonar permitiendo prolongar el tiempo de isquemia fría de los injertos pulmonares con excelentes resultados. Presentamos el caso de dos trasplantes pulmonares de dos donantes diferentes empleando dos métodos de preservación distintos, recalcando los beneficios de utilizar este novedoso método de preservación a 10 °C.
Logistics are crucial to medium size lung transplant programs, especially in cases when two or more donors are offered at the same time. Depending on the availability of transplant teams, including surgeons, anesthesiologists and perfusionists, it is not normally possible to perform simultaneously two lung transplantations, especially overnight.
Current studies are clinically exploring the feasibility of prolonged pulmonary preservation at 10 °C instead of the standard cold storage on ice at 4 °C bringing benefits to both patients and health care teams1. Extending the cold ischemia time may have an important impact in logistics of lung transplantation (LTx) by avoiding nighttime or intentionally delaying the surgery.
Herein we present the case of two lung transplants (LTx) from two different donors which became available at the same time, and we were able to carry out consecutively thanks to this novel method of preservation at 10 °C.
Surgical techniqueWe report two cases of LTx from two different donors offered simultaneously but submitted to different preservation protocols.
Current standard lung preservation at 4 °C consists in storing the lungs in an ice cooler from the donor retrieval until the recipient implant surgery, which is carried out immediately upon arrival to the hospital without intentionally extending the total preservation time.
Recently, the Toronto Lung Transplant Program (TLTP) has tested a new protocol for lung preservation at 10 °C. This change in the temperature for cold storage allows to safely prolong the cold ischemia time1. We adapted this protocol to our environment resulting in several benefits for the program, such us logistics of the procedure. After retrieval, the grafts were transported as usually on ice at 4 °C upon arrival to the hospital when they were transferred to a refrigerator set at 10 °C until be implanted (MYTEMP™65HC, Benchmark Scientific). This incubator provides a precise and uniform temperature.
Using this approach, our group was able to accept two simultaneous donors and perform both LTx delaying the most complex one to the next morning.
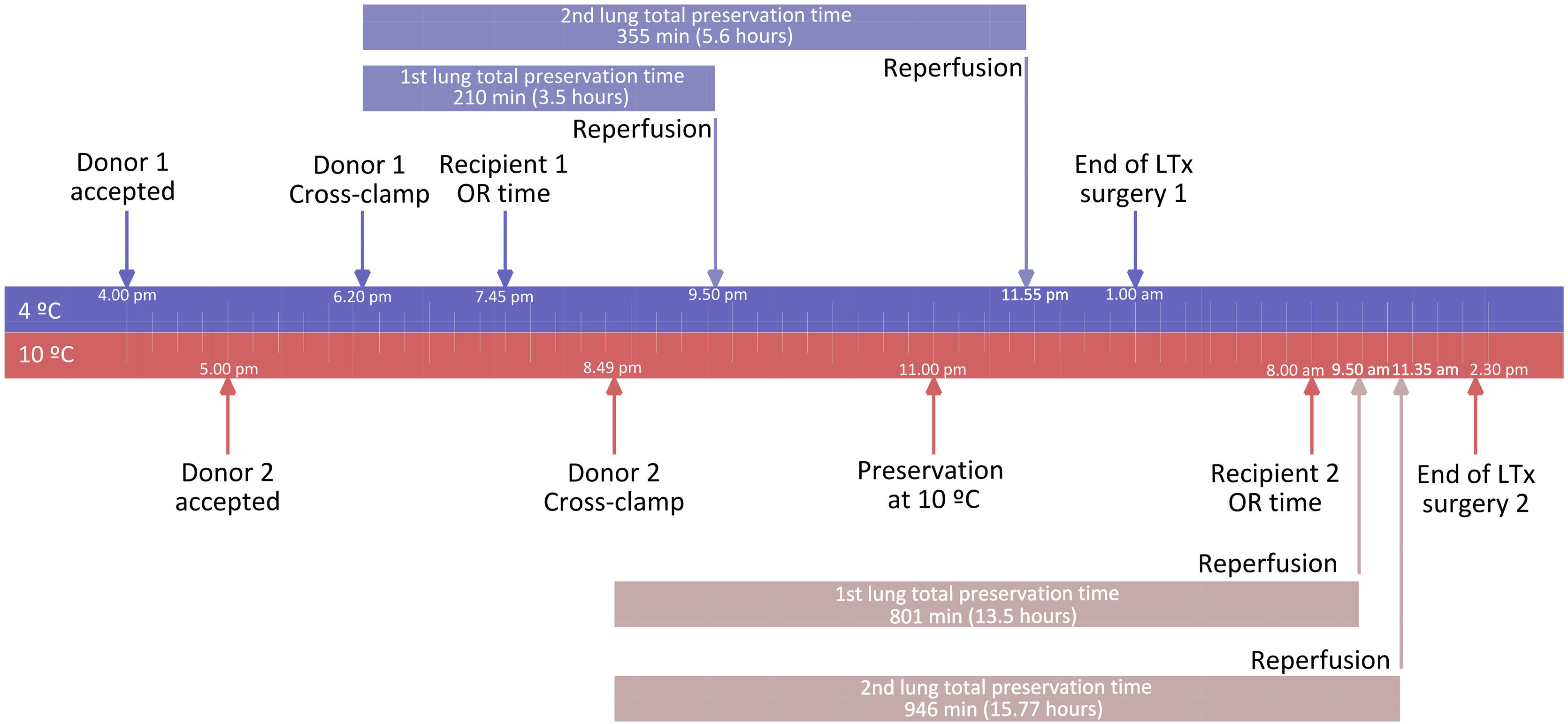
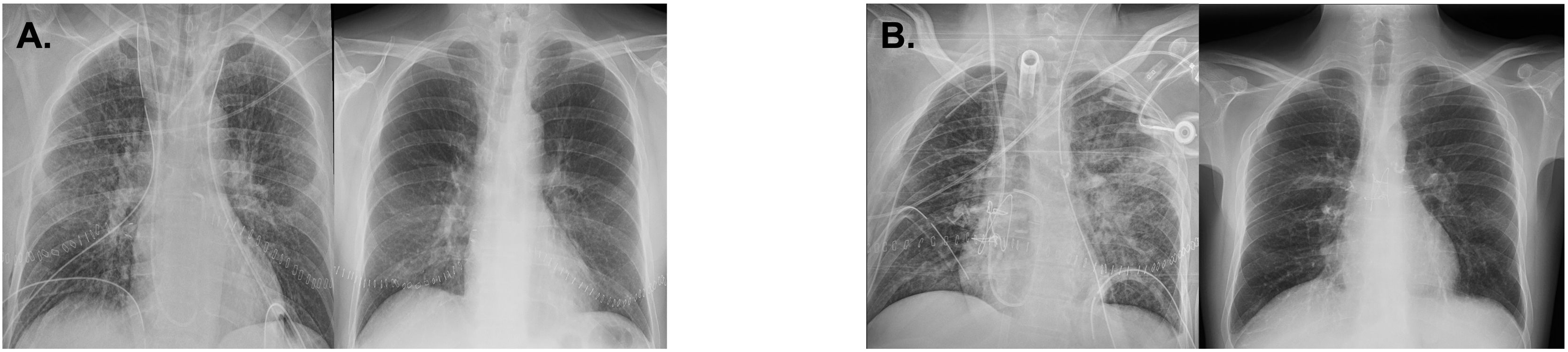
Fig. 1 shows the timeline for these two cases. The first available organs were from our hospital. Briefly, the donor was a 70-year-old male brain death donor (BDD). Arterial oxygen tension/inspired oxygen fraction (P/F) ratio was 468 and chest X-ray and bronchoscopy were normal. Cross-clamp time was at 6.20 pm. A standard procurement was carried out and the grafts were stored and transported in a regular ice-cooler at 4 °C. The recipient was 57-year-old male who suffered from chronic obstructive pulmonary disease (COPD) with no pulmonary hypertension. The recipient operating room (OR) time was 7.45 pm, and the double lung transplant was uneventful ending at 1 am with a total preservation time (including cold and warm ischemia times) of 210 min (3.5 h; first graft) and 335 min (5.6 h; second graft). The patient was extubated in the first 24 h, discharged from intensive care unit (ICU) on postoperative day (POD) 6 and from hospital on POD 35. Fig. 2A shows his radiographic progression.
One hour after accepting the first case, another donor became available for a patient with emergency status. The donor was also a BDD. P/F ratio was 404, with no abnormal findings on chest X-ray or bronchoscopy. Cross-clamp time was at 8.49 pm and the lungs were recovered and stored on ice until arriving at our center. After 2 h and 11 min the grafts were transferred to a refrigerator set at 10 °C at 11 pm. At that time, the first transplant was still ongoing. The recipient was on awake peripheral veno-venous extracorporeal respiratory support (VV-ECMO) for six weeks due to cystic fibrosis aggravated by post-COVID acute respiratory syndrome. The patient was called to the OR at 8.00 am. The donor lungs were preserved at 10 °C for 10 h in the case of the first graft (from 11 pm to 9.15 am), and more than 12 h for the second graft (from 11 pm to 11.45 am). The total preservation time (including cold and warm ischemia times) was 801 min (13.35 h) and 946 min (15.77 h) for the first and second graft, respectively. Surgery was uneventful needing central cannulation for ECMO support. P/F ratio before closing was above 300. However, due to the long duration of the previous peripheral ECMO support, we decided to keep it in place preventively. The evolution of the graft gas exchange was excellent and the patient was weaned from VV-ECMO 48 h after transplant. No primary graft dysfunction (PGD) was observed at first 72 h. The patient had no other complications and was discharged from the ICU on POD 13 and from hospital on POD 54. Fig. 2B shows the chest X-ray progression.
After 6 months of follow up both patients made an excellent recovery without other significant complications.
DiscussionUsing the standard preservation on ice at 4 °C cold ischemic times over six hours have been directly related to a higher early mortality2. On the other hand, a few decades ago, 10 °C has been suggested to be the ideal temperature for lung preservation but this has never been translated to the clinical practice3.
Recent studies have been published by the TLTP in order to evaluate the safety and biological impact of prolonged storage at 10 °C in porcine and human lungs. Ali et al. described in an experimental animal model that 36 h-preservation at 10 °C offers better metabolomics and lung function profile than conventional preservation on ice after 12 h on normothermic EVLP evaluation. They applied this strategy to five patients who received lungs after a total preservation time up to 16.5 h showing no PGD grade 3 at 72 h1. This work focused on investigating the role of mitochondrial function in the ischemia-reperfusion injury, demonstrating higher concentrations of protective molecules such as itaconate when lungs are preserved at 10 °C1,4. Moreover, they have lately evaluated the impact of 10 °C in injured lung donors using pigs. Grafts preserved at 10 °C during 12 h maintained better oxygenation and less mitochondrial stress in comparison to those immediately implanted after standard preservation at 4 °C5. This group also recently published a clinical case in which two single transplants were successfully performed from the same donor. The first single LTx was performed directly using the standard cold preservation (ice cooler), and the second graft was kept in the 10 °C refrigerator for at least 10 h6. The total preservation time for this second graft was 15 h and 20 min.
Using this novel approach we were able not only to accept two simultaneous donors but also to delay the most complex of the two cases to day-time, avoiding doubling OR teams at nighttime. This idea of intentionally prolonging the cold ischemia time by using 10 °C for preservation is currently being tested in a multicenter clinical trial (ClinicalTrials.gov identifier: NCT04616365). Our institution adopted this protocol and recruited patients in this trial (Ethical Board approval code PI_118_21).
Preserving donor grafts at 10 °C may help in LTx logistics, as detailed here, with excellent outcomes for these two patients, being able to benefit as many recipients on the waiting list as possible. Preservation at 10 °C offers the advantage of prolonging the cold ischemia time, therefore allowing us to accept two simultaneous donors and avoiding two simultaneous OR teams at nighttime. Implementing this preservation technique throughout all lung transplant programs would mean not having to refuse any suitable donor due to the availability of transplant teams, avoid more nighttime procedures and potentially overcome other logistics challenges.
Conflict of interestThe authors have no conflict of interests to declare.
This study has been funded by several entities: Fundación Neumomadrid, Fundación SECT, Fundación SEPAR, Sociedad Madrileña de Trasplantes and Fundación Mutua Madrileña.