To analyse the potential advantages and outcomes of the new Harmonic Focus™ (Focus) device compared to the Harmonic Scalpel™ ACS-14C in benign thyroid surgery.
MethodsA controlled randomised study was conducted in which the Focus was compared to former ACS-14C device in patients undergoing total thyroidectomy for multinodular goitre. The primary endpoint was time of surgery. The secondary endpoints were time of use of the device, number of ligatures, blood loss, hypocalcaemia, laryngeal nerve impairment, postoperative pain and quality of life.
ResultsTwo groups of patients were included, 26 patients in group I (ACS-14C) and 28 in group II (Focus). There was a 16% reduction in surgical time (78.7±22.01 vs 66±17.0min; P<.05) between group I and II, respectively. The Focus was used longer than the ACE-14S, both in absolute time (26.0±7.7 vs 10.0±3.5min; P<.05) and in relative time (40.7±11.8% vs 13.1±4.1%; P<.05), respectively.
A significant reduction in number of ligatures in Focus patients was also observed (0.3±0.8 vs 2.9±3.6; P<.05).
Budget impact analysis showed an additional average savings per procedure of 179.74€.
ConclusionsFocus ergonomics significantly improved the operation time in thyroidectomy causing a positive impact on the budget.
Focus also adds further benefits to those previously achieved by Harmonic technology, and it is by itself more cost-effective in total thyroidectomy than ACS-14C.
El bisturí armónico ha mejorado la cirugía tiroidea, cuando se compara con cirugía convencional, en términos de reducción del tiempo quirúrgico, número de ligaduras, dolor postoperatorio y uso de drenajes. Analizamos las posibles ventajas en reducción de tiempo quirúrgico y ahorro de recursos del terminal Focus en comparación con el terminal ACS-14C en la cirugía tiroidea benigna.
MétodosEstudio ciego, prospectivo y aleatorizado realizado desde 2009 hasta 2010.
Se compararon los resultados del ACS-14C (grupo i) con Focus (grupo ii) en pacientes con bocio multinodular operados de tiroidectomía total.
Se incluyó a pacientes entre 18 y 80 años que aceptaron participar en el estudio sin cirugía cervical previa, lesión del nervio recurrente laríngeo, tratamiento analgésico crónico, coagulopatía o problemas cognitivos. La variable principal fue el tiempo quirúrgico. Otras variables secundarias fueron: tiempo de uso del dispositivo durante el procedimiento, número de ligaduras, pérdida hemática, hipocalcemia, lesión del nervio recurrente faríngeo, dolor postoperatorio y análisis de calidad de vida.
ResultadosSe incluyó a 54 pacientes, 26 en el grupo i y 28 en el grupo ii. En el grupo de Focus hubo una reducción del tiempo quirúrgico de 16% (78,7±22,01 vs. 66±17,0min; p<0,05), del número de ligaduras (0,3±0,8 vs. 2,9±3,6; p<0,05) y un ahorro adicional de 179,74€ por procedimiento.
Focus se utilizó más tiermpo que ACE-14S tanto en valor absoluto (26,0±7,7 vs. 10,0±3,5min; p<0,05) como en valor relativo (40,7±11,8 vs. 13,1±4,1%; p<0,05).
ConclusionesFocus mejora el tiempo operatorio en la tiroidectomía, causando impacto positivo sobre el presupuesto. Su mayor utilización hace que sea una herramienta más coste-eficaz que el terminal ACS-14C.
The use of the harmonic scalpel (HS) has improved thyroid surgery by reducing operation times, postoperative pain, and the need for ligatures and drainage.1–4 Previous publications, including a study by Miccoli and Barczynsky, have evaluated the use of harmonic scalpels in minimally invasive thyroid surgeries.5,6 Despite the high costs associated with the adoption of cutting edge technologies, the HS has been rapidly incorporated into surgical routines without an objective study of cost-effectiveness or budgetary impacts.
This study aimed to analyse the results of the new Harmonic Focus device (Focus; Ethicon Endo-Surgery, Cincinnati, OH, USA) during benign thyroid surgery and its potential advantages over the conventional ACS-14C terminal (Ethicon Endo-Surgery, Cincinnati, OH, USA), as well as the economic impact.
Methods and MaterialsThis prospective randomised study was conducted from January 2009 to March 2010 at Bellvitge University Hospital (HUB; Barcelona). The study was developed in accordance with the principles of good clinical practice and the Helsinki Declaration and was approved by the HUB Ethics Committee.
All patients included in this study received oral and written information about the study and gave their consent prior to participation.
Study DesignAll patients with multinodular goitres (MNG) and indication for surgical treatment were referred to the Endocrine Surgery unit.
The preoperative study included a routine laryngoscopy to confirm normal vocal chord mobility and, 1 month before the surgery, an ultrasound to evaluate the thyroid volume.7
All consenting patients between the ages of 18 and 80 years with MNG were included in the study. Patients with altered vocal chord mobility, a history of previous neck surgeries, chronic or transitory treatment with NSAIDs or analgesics during the period of study, clotting disorders, or cognitive degeneration were excluded.
The study was proposed to the candidates as a 2-armed randomised study to compare the results of thyroidectomies performed with 2 HS devices, the ACS-14C and Focus.
The major variable was the time required to perform the thyroidectomy. Secondary variables included the total and relative times of device use during the procedure, number of sutures, blood loss, hypocalcaemia (temporary or persistent), injury to the recurrent laryngeal nerve (RLN), incision length, post-operative pain measured in accordance with a visual pain scale, post-thyroidectomy quality of life (EuroQol; EQ),8 and a budgetary analysis.
The same 2 surgeons performed all procedures.
RandomisationRandomisation via sealed envelope occurred in the operating room on the day of surgery. Half of the patients were randomly assigned to group I (ACS-14C) and the other half to group II (HF), at a 1:1 ratio. Patients were not informed of the results of the randomisation until the study was completed.
Surgical TechniqueDuring total thyroidectomy (TT), defined as a total bilateral extracapsular lobectomy, the Focus or ACS-14C and bipolar forceps were used for tissue division, sealing, and vessel coagulation.9
The use of ligatures was determined by the surgeon, depending on the vessel size.
Operating ProcedureThe operation time was measured from the moment of cutaneous incision to the excision of the thyroid gland. The percentage of time that the device was used during the TT was calculated as follows: time using the device×100/operation time.
The incision length was measured after the skin was closed.
Analytical MethodsParathyroid hormone (PTH) levels were determined in the manner previously published by our group.10 Blood samples were extracted at the beginning of surgery and at 10min after thyroid gland removal and were labelled basal and post-thyroidectomy, respectively.
The plasmatic concentration of intact PTH was measured with an Immulite-Turbo chemiluminescent immunometric assay (Diagnostic Products, Los Angeles, CA, USA). The PTH standard reference interval in our laboratory ranges from 14 to 74pg/ml (1.5–7.8pmol/L). This method had an 8% coefficient of variation for concentrations within the reference interval, and the functional sensitivity (the concentration for which the method had a 20% coefficient of variation) was 7pg/ml (75pmol/L). The relative reduction or percent reduction in PTH was calculated as follows: ((preoperative PTH- post-resection PTH)/preoperative PTH)×100. Serum calcium levels were measured in a calorimetric assay, using the Hitachi Modular analyser (Roche Diagnostics, Mannheim, Germany). The standard reference interval for calcium in our laboratory ranges from 8.6 to 10.0mg/dl (2.15–2.50mmol/L).
“Permanent” complications were defined as RLN lesions that had not healed by the sixth post-operative month or hypocalcaemia that required treatment with calcium supplements during the same time interval.
The numbers of ligatures and sutures required for each patient were recorded.
Blood loss was estimated by the weight of the gauze before and after use. 1g was calculated as 1ml of blood.
Drainage use was considered on a case-by-case basis because it was not included in our standard protocol.
ProcedurePatients were treated according to the standard protocol and discharged from the hospital 24h after the surgery. Patients with reduced intraoperative PTH levels >62.5% or postoperative PTH levels <1.9mg/dl began treatment with calcium supplements (oral or intravenous) at the time of their first meal.10
Serum calcium levels were measured daily at 7:00 am until hospital discharge.
Hypocalcaemia was defined as a serum calcium level <86mg/dl (<2.15mmol/L). Calcium supplements were prescribed when the serum calcium levels were ≤7.2mg/dl (≤1.8mmol/L) or for values between 7.2 and 8.6mg/dl (1.8–2.15mmol/L) when accompanied by symptoms of clinical hypocalcaemia (Trousseau's sign, tetany, or paraesthesia).
The calcium supplement dosage (oral route) required during hospitalisation or at discharge was recorded.
Pain was evaluated on a visual analogue scale at 24h and 7days after surgery as a part of postoperative pain control. The type and dosage of analgesic required to control the pain were also recorded.
In cases that required prolonged hospitalisation, pain was evaluated every 24h until discharge.
The post-operative quality of life was evaluated with the EQ-5D questionnaire during the follow-up period.8
The follow-up appointments for patients who did not experience complications occurred at 1 week and 6 months after surgery. Patients who experienced complications had a monthly follow-up until recovery or 6 months after surgery.
Monthly indirect laryngoscopic check-ups were performed for patients with laryngeal nerve lesions for 6 months or until injured vocal chord movement was confirmed.
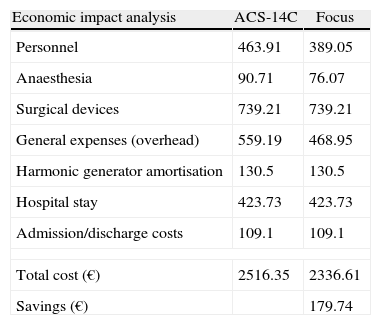
Cost Impact AnalysisThe economic impact analysis weighed the costs of the total thyroidectomy (in accordance with the prices at our surgical centre) against the relative costs of the saved surgical time. The following factors were considered: personnel (composed of the surgical team, which was similar in both arms of the study), anaesthetic drug use, medical devices, overhead costs, cost of the HS generator, and costs of hospitalisation and admission (administrative costs).
StatisticsStatistical analysis was performed according to the protocol. The sample size was calculated according to previously published results.1,4 Assuming a difference in operation times of 15% between groups II and I for a total thyroidectomy and an average operation time of 100min with a standard deviation of 25min, the calculated required sample size was 45 patients per group, for a power of 80%. Due to recruitment difficulties, we performed an intermediate analysis and stopped when we obtained statistical significance.
The categorical values are expressed as numbers of patients and percentages. A 2-variable chi-squared distribution and Fisher's test were used for categorical values, and the Mann–Whitney test was used for variables that did not follow a normal distribution. Statistical analyses were performed with SPSS version 18 for Microsoft Windows (SSPS, Inc., Chicago, IL, USA). P-values of <.05 were considered significant.
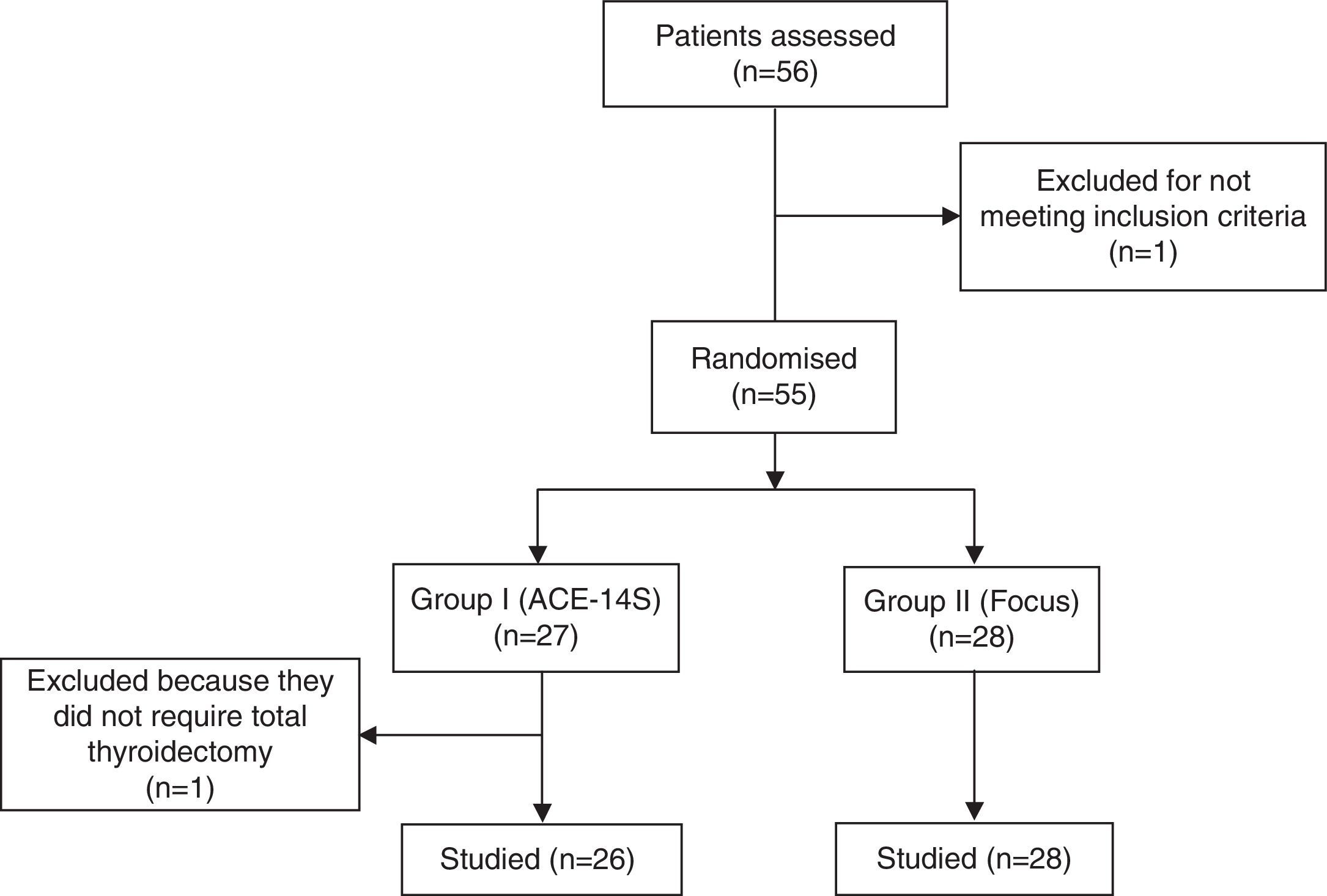
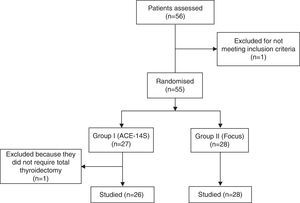
ResultsFifty-six patients were included in the study (Fig. 1). Two patients were excluded: 1 patient did not require a total thyroidectomy and therefore underwent partial thyroidectomy; the other was excluded for chronic analgesic use while on the waiting list.
The remaining 54 patients were divided as follows: 26patients in group I (ACE-14S) and 28 in group II (Focus).
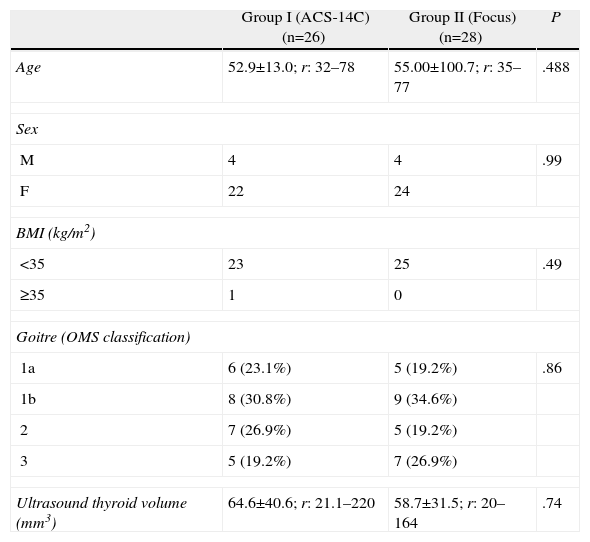
The groups were homogenous and comparable (Table 1).
Characteristics of the Study Groups.
| Group I (ACS-14C)(n=26) | Group II (Focus)(n=28) | P | |
| Age | 52.9±13.0; r: 32–78 | 55.00±100.7; r: 35–77 | .488 |
| Sex | |||
| M | 4 | 4 | .99 |
| F | 22 | 24 | |
| BMI (kg/m2) | |||
| <35 | 23 | 25 | .49 |
| ≥35 | 1 | 0 | |
| Goitre (OMS classification) | |||
| 1a | 6 (23.1%) | 5 (19.2%) | .86 |
| 1b | 8 (30.8%) | 9 (34.6%) | |
| 2 | 7 (26.9%) | 5 (19.2%) | |
| 3 | 5 (19.2%) | 7 (26.9%) | |
| Ultrasound thyroid volume (mm3) | 64.6±40.6; r: 21.1–220 | 58.7±31.5; r: 20–164 | .74 |
Values represent means±standard deviations.
BMI: body mass index; r: range.
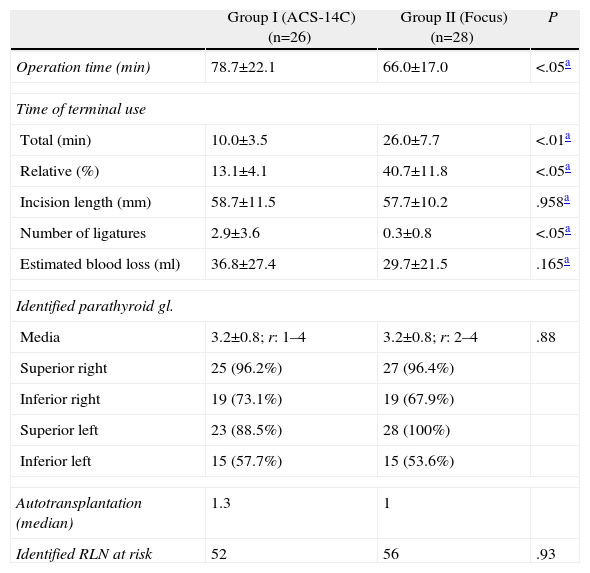
The use of Focus significantly reduced the average operation time by 13min (78.7±22.1min for group I vs 66.0±17.0min for group II; P<.05), representing a 16% reduction in the operation time (Table 2).
Results I.
| Group I (ACS-14C)(n=26) | Group II (Focus)(n=28) | P | |
| Operation time (min) | 78.7±22.1 | 66.0±17.0 | <.05a |
| Time of terminal use | |||
| Total (min) | 10.0±3.5 | 26.0±7.7 | <.01a |
| Relative (%) | 13.1±4.1 | 40.7±11.8 | <.05a |
| Incision length (mm) | 58.7±11.5 | 57.7±10.2 | .958a |
| Number of ligatures | 2.9±3.6 | 0.3±0.8 | <.05a |
| Estimated blood loss (ml) | 36.8±27.4 | 29.7±21.5 | .165a |
| Identified parathyroid gl. | |||
| Media | 3.2±0.8; r: 1–4 | 3.2±0.8; r: 2–4 | .88 |
| Superior right | 25 (96.2%) | 27 (96.4%) | |
| Inferior right | 19 (73.1%) | 19 (67.9%) | |
| Superior left | 23 (88.5%) | 28 (100%) | |
| Inferior left | 15 (57.7%) | 15 (53.6%) | |
| Autotransplantation (median) | 1.3 | 1 | |
| Identified RLN at risk | 52 | 56 | .93 |
Values represent means±standard deviations.
r: range.
The total device usage time was significantly different between the groups (10.0±3.5min in group I vs 2.0±7.7min for group II; P<.05). The percentage of time that the device was used during the total thyroid surgery duration was significantly higher in group II than in group I (13.1%±4.1% vs 40.7%±11.8%, respectively; P<.05).
The number of ligatures was significantly reduced in group II (2.9±3.6 vs 0.3±0.8; P<.05; Table 2).
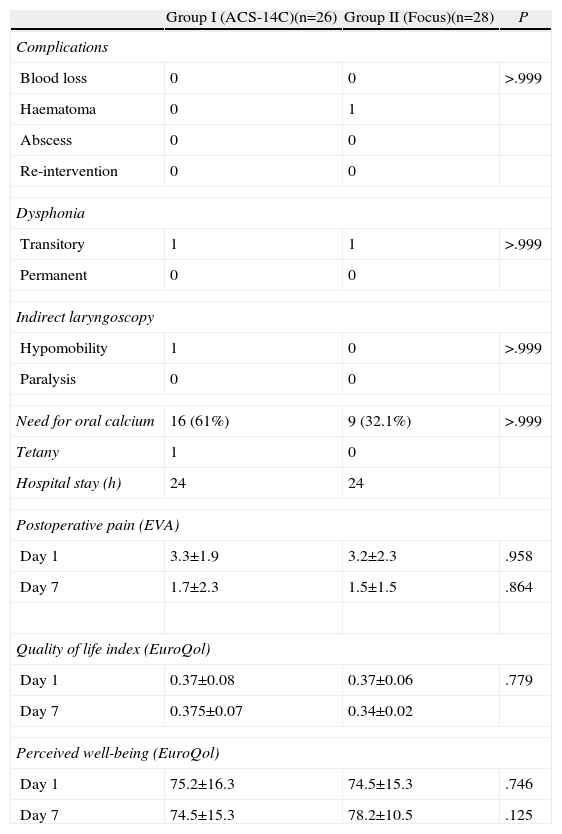
There were no differences with regard to intraoperative blood loss, incision size, the number of identified or transplanted parathyroid glands, or the number of identified at-risk RLN. One patient with an extremely narrow RLN (group II) presented with dysphonia in the immediate post-operative period. Indirect laryngoscopy revealed a hypomobile CV that spontaneously recovered after 3 weeks (P>.9; Table 3).
Results II.
| Group I (ACS-14C)(n=26) | Group II (Focus)(n=28) | P | |
| Complications | |||
| Blood loss | 0 | 0 | >.999 |
| Haematoma | 0 | 1 | |
| Abscess | 0 | 0 | |
| Re-intervention | 0 | 0 | |
| Dysphonia | |||
| Transitory | 1 | 1 | >.999 |
| Permanent | 0 | 0 | |
| Indirect laryngoscopy | |||
| Hypomobility | 1 | 0 | >.999 |
| Paralysis | 0 | 0 | |
| Need for oral calcium | 16 (61%) | 9 (32.1%) | >.999 |
| Tetany | 1 | 0 | |
| Hospital stay (h) | 24 | 24 | |
| Postoperative pain (EVA) | |||
| Day 1 | 3.3±1.9 | 3.2±2.3 | .958 |
| Day 7 | 1.7±2.3 | 1.5±1.5 | .864 |
| Quality of life index (EuroQol) | |||
| Day 1 | 0.37±0.08 | 0.37±0.06 | .779 |
| Day 7 | 0.375±0.07 | 0.34±0.02 | |
| Perceived well-being (EuroQol) | |||
| Day 1 | 75.2±16.3 | 74.5±15.3 | .746 |
| Day 7 | 74.5±15.3 | 78.2±10.5 | .125 |
As shown in Table 3, 64% of the patients from group I and 36% from group II required oral calcium supplements (oral route) due to intraoperative PTH values P<.05. One patient from group I presented with symptoms of tetany, although no patients were permanently hypocalcaemic. There were no significant differences related to the appearance of complications, length of hospitalisation, pain, need for analgesics, or subjective pain perception between the groups (EQ).
Budgetary Impact AnalysisAccording to the collected data, the surgical time was reduced by 13min in the Focus group (group II), thus saving an estimated 174.74€ (Table 4).
Economic Impact.
| Economic impact analysis | ACS-14C | Focus |
| Personnel | 463.91 | 389.05 |
| Anaesthesia | 90.71 | 76.07 |
| Surgical devices | 739.21 | 739.21 |
| General expenses (overhead) | 559.19 | 468.95 |
| Harmonic generator amortisation | 130.5 | 130.5 |
| Hospital stay | 423.73 | 423.73 |
| Admission/discharge costs | 109.1 | 109.1 |
| Total cost (€) | 2516.35 | 2336.61 |
| Savings (€) | 179.74 | |
All savings were related directly or indirectly to the reduced operation time.
DiscussionHS technology has proven safe and effective and has been shown to improve thyroid surgery in terms of reduced surgical times, a reduced need for ligatures, reduced pain, and reduced postoperative drainage, compared to conventional thyroidectomy.1–4 This technology also has a definite role in minimally invasive thyroid surgery.5,6
The Focus was designed to improve thyroid surgery through better ergonomics by permitting the use of a scissor as a dissector with both gripping and dissection capacity. This improves the surgical time by reducing the number of device changes between the surgeon and the instrumentalist.
The objective of this study was to evaluate the results and possible advantages of the new Focus device compared to the less ergonomic conventional ACE-14S. We assume that in many institutions, conventional thyroidectomy includes the routine use of HS and/or other energy devices.
The groups of patients that underwent surgery with the ACS-14C and Focus devices were homogenous and comparable. Regarding the principal objective of the study, the Focus reduced operation times by 16% (13min), compared to the ACE-14S, a result that was confirmed in a similar recently published study.11 In addition, the Focus was used for a longer time during surgery, compared to ACS-14C, when measured both absolutely and relative to the total surgery time (%) and reduced the thyroidectomy cost by 179.75€ (Tables 2 and 3).
Several factors contributed to the reduction in surgical time. Improved ergonomics allowed more surgical manoeuvres without changing the surgical instrument. The number of surgical manoeuvres was estimated indirectly from the percentage of surgical time during which the device was used.
The Focus group required significantly fewer ligatures; this also contributed to the reduced surgical time, although to a lesser extent. The first studies that compared HS with conventional techniques demonstrated that fewer ligatures were crucial to reductions in surgical time.3 In this study, however, the number of ligatures was less important, and the reduction in surgical time could be primarily attributed to the extended use of the device during surgery.
In this study, use of the Focus reduced the surgical time by 13min and decreased the number of required ligatures when compared to the ACE-14S, thus reducing the cost per procedure by 179.74€. Other variables such as the length of hospital stay and surgical complications did not differ between the groups and did not influence the final budgetary analysis. The majority of previous studies concluded that HS is cost-effective with respect to conventional haemostasis with ligatures, clips or electro-cauterisation, although the most important variable has consistently been the reduction in operation time.2,4,12–14 Not all publications, however, have reported an economic benefit when comparing HS with conventional haemostasis.6,15–17
It is difficult to determine the full economic impact of the Focus in total thyroidectomies, as no previous studies have compared the impact of conventional haemostasis. Two recent meta-analysis papers reported that HS reduced operating times by 22.67 and 23.1min.18,19 It seems logical to suggest that the Focus is highly effective when compared to conventional surgery, both in cost and in surgical time.
The relative increase in the device usage time throughout thyroidectomy with the Focus (up to 44%) shows that, although it is made of disposable materials, Focus use is more cost effective than ACS-14C use for total thyroidectomy.
Management of the saved surgical time should allow an increase in the number of surgical procedures in a single surgical session and better management of resources.
Routine intraoperative PTH (PTHio) measurements allowed us to predict post-thyroidectomy hypocalcaemia immediately and treat our patients on an outpatient basis or during 24-h hospital stays.10,20 Although there was no difference in the number of identified or autotransplanted parathyroid glands, our PTHio measurements predicted a higher rate of hypocalcaemia for group I patients. It is difficult to explain the basis of this difference. Melck et al. reported fewer episodes of transitory hypocalcaemia in patients who underwent HS surgery compared to surgery performed with conventional haemostasia19; the authors speculated that HS obligated dissection of the parathyroid glands farther from the thyroid gland. In our case, identification and dissection of the parathyroid glands were similar in both groups, and we are thus unable to explain the discrepancy in the predicted PTHio.
Patients were examined via indirect laryngoscopy 1 week after surgery in all cases where RLN injury was identified as a risk. There were no significant differences between the groups regarding RLN lesions. One patient in group II presented with post-operative dysphonia due to a hypo mobile right vocal fold, which spontaneously recovered 3 weeks later. We attribute this to the dissection of an extremely delicate RLN, as reported in the surgical notes. From a technical perspective, this thyroidectomy was performed with bipolar forceps and HS. Once the RLN has been exposed, the distal section, from whence the inferior thyroid artery or its branches cross underneath, is dissected with a dissector and bipolar forceps to the insertion of the RLN in the cricoarytenoid muscle. In this region, the nerve is fixed to the surrounding anatomical structures, which are much thicker than the nerve; therefore, the use of powered devices for nerve dissection is inappropriate, and furthermore, carries the risk of thermal injury.
No differences were observed in the dissected thyroid volume, blood loss, incision size, or the rate of complications between the 2 groups with respect to haemorrhage, haematoma, wound infection, and re-intervention.
The same was true with respect to pain evaluation and quality of life perception. The groups responded similarly to the visual pain scale and the EQ-5D questionnaire at 1 and 7days after surgery. Miccoli suggested that harmonic technology should reduce postoperative pain because of the reduction in muscle fibre stimulation.4 Our study did not corroborate this finding, although the fact that the Focus and ACS-14C use the same ultrasonic waves might explain the lack of pain reduction associated with the harmonic device in both groups.
The limitations of this study should be considered. The operation and device utilisation time might be affected by differences in the experience levels within the surgical team. Although it was not reported in the results, this variable was evaluated and we found no significant differences.
We do not believe that the reduced sample size significantly biased the data, and we estimate that with a greater number of patients, the statistical significance would be greater.
The economic impact analysis is specific to our hospital and country, as there are no uniform criteria for the accounting methods of cost per procedure.
ConclusionThe ergonomic Focus device offers additional advantages over those already achieved with HS technology, with respect to reduced operation times and consequent economic savings. Although this device is disposable, its functionality during the procedure makes it cost-effective when compared to similar, older devices. Use of the harmonic Focus thus has repercussions for surgical centre management.
Conflict of InterestThis study was funded by Ethicon Endosurgery.
Please cite this article as: Moreno P, Francos JM, García-Barrasa A, Fernández-Alsina E, de Lama E, Martínez R, et al. Eficacia e impacto económico del bisturí armónico Focus frente al dispositivo ACS-14C en la tiroidectomía total por bocio multinodular. Estudio prospectivo aleatorizado. Cir Esp. 2013;91:664–671.