In spite of the acquired experience with laparoscopic common bile duct exploration (LCBDE) for choledocholithiasis management, there is still a risk of biliary leakage of 5–15% following choledochotomy closure. We evaluate the usefulness of fibrin-collagen sealants to reduce the incidence of biliary fistula after laparoscopic choledochorrhaphy.
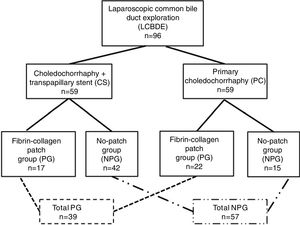
MethodsWe report a retrospective analysis of 96 patients undergoing LCBDE from March 2009 to March 2017, whose closure of the bile duct was completed by antegrade stenting and choledochorraphy or by performing a primary suture. The study population was divided into two groups according to whether they received a collagen-fibrin sealant covering the choledochorrhaphy or not, analyzing the incidence of postoperative biliary fistula in each group.
ResultsThirty-nine patients (41%) received a fibrin-collagen sponge while the bile duct closure was not covered in the remaining 57 patients (59%). The incidence of biliary fistula was 7.7% (three patients) in the first group and 14% (eight patients) in the second group (P=.338). In patients who underwent primary choledochorraphy, the fibrin-collagen sealant reduced the incidence of biliary leakage significantly (4.5% vs 33%, P=.020), which was a protective factor with an odds ratio of 10.5.
ConclusionFibrin-collagen sealants may decrease the incidence of biliary fistula in patients who have undergone primary bile duct closure following LCBDE.
A pesar de la experiencia existente con la exploración laparoscópica de la vía biliar principal (ELVBP) en el tratamiento de la coledocolitiasis y de su eficacia bien demostrada, hay un riesgo de aparición de fístulas biliares de entre un 5 y un 15% tras el cierre de la coledocotomía. Evaluamos la utilidad de los sellantes de fibrina-colágeno para reducir la incidencia de fístulas biliares tras la coledocorrafia laparoscópica.
MétodosPresentamos un análisis retrospectivo de 96 pacientes diagnosticados de coledocolitiasis sometidos a ELVBP desde marzo de 2009 a marzo de 2017. El cierre de la vía biliar se completó mediante coledocorrafia tras colocación de stent plástico transpapilar (CS) o realizando una sutura primaria (CP). La población de estudio fue dividida en dos grupos: pacientes con coledocorrafia cubierta con una lámina de colágeno-fibrina (GL) y pacientes con coledocorrafia sin cubrir (GSL). Se presenta el análisis de incidencia de aparición de fístulas biliares postoperatorias.
ResultadosTreinta y nueve pacientes (41%) fueron incluidos en el grupo GL, mientras que el grupo GSL fue formado por los 57 pacientes restantes (59%). Se demostró la homogeneidad de los grupos. La incidencia de fístulas biliares fue del 7,7% (3 pacientes) en el primer grupo y del 14% (8 pacientes) en el segundo (p=0,338). La lámina de fibrina-colágeno redujo la incidencia de fístulas biliares de forma significativa en el subgrupo de los pacientes con CP (4,5% vs 33%, p=0,020), siendo un factor protector con una odds ratio de 10,5.
ConclusiónLa lámina de fibrina-colágeno aplicada sobre la coledocorrafia tras un cierre primario de la vía biliar puede tener un papel importante en la reducción significativa de la incidencia de fístulas biliares postoperatorias.
It has been reported that between 10 and 15% of patients referred for laparoscopic cholecystectomy present with choledocholithiasis.1–3 However, a consensus on the best therapeutic approach for bile duct stones has not yet been reached. At present, endoscopic retrograde cholangiopancreatography (ERCP), followed by laparoscopic cholecystectomy (LC) in a second step, is the preferred option in most centers.4,5 Despite this, the results of the endoscopic approach and laparoscopic common bile duct exploration (LCBDE) and LC in the same procedure are similar in terms of efficacy and associated morbidity.1,6–16 One of the reasons that LCBDE has not become the gold standard for the treatment of choledocholithiasis is due to the technical difficulty and the morbidity associated with the closure of the choledochotomy after the extraction of the calculi. Traditionally, a Kehr T-tube has been used to protect the choledochorraphy from biliary fistulae. However, the morbidity associated with the drain tube itself and its withdrawal has led to the progressive replacement of this technique in recent years with the closure of the bile duct protected by transpapillary plastic prostheses or by performing a primary choledochorrhaphy.17–22 Even so, the incidence of biliary fistulae after LCBDE varies between 5 and 15%,11,20,22 the main complication being associated with the procedure.
In 2004, a collagen sponge coated with human fibrinogen and thrombin23 appeared on the market, which was originally used as a hemostatic in liver surgery to cover the transection site.24,25 Subsequently, it was found that the collagen component adds tissue sealing properties, due to which its use has been extended to other purposes. There have been reports of the usefulness of fibrin-collagen patches to reduce the appearance of biliary fistulae after hepatectomy.26,27 However, there are no studies in humans that determine the efficacy of biliary sealing to protect choledochorrhaphy after LCBDE. The objective of the present study is to determine the usefulness of fibrin-collagen sealants to reduce the incidence of biliary fistulae after laparoscopic choledochorrhaphy.
MethodsPatient SelectionWe performed a retrospective analysis of 96 consecutive patients diagnosed with choledocholithiasis by magnetic resonance cholangiopancreatography (72 cases), transabdominal ultrasound (19 patients), computed tomography (3 cases) and endoscopic ultrasound (1 case). The remaining patient was diagnosed by intraoperative cholangiography. All patients underwent elective LCBDE surgery at our medical center between March 2009 and March 2017. The protocol for the treatment of choledocholithiasis included LCBDE and LC for all patients, except patients who did not present a dilated bile duct (<9mm measured on imaging tests) were cholecystectomized or had limited quality of life with important comorbidity ruling out surgery. These patients underwent ERCP, with or without subsequent LC.
Surgical TechniqueAll the interventions were performed by the three surgeons of the Hepato-Biliary-Pancreatic Surgery Unit. After exposing the bile duct, a supraduodenal choledochotomy was sufficient for the extraction of the stones. The bile duct was cleaned with pressure irrigation or extraction by balloon catheter or a Dormia basket, as necessary. The absence of residual lithiasis was guaranteed by video-choledochoscopy and/or intraoperative cholangiography. After cleaning the common bile duct, it was closed. In the first 6 years of the series, the most commonly used technique was the placement of a plastic transpapillary intracholedochal prosthesis (7 or 8.5 French and a length between 5 and 9cm, depending on the case) followed by choledochorrhaphy with continuous 4–0 monofilament suture. The placement of the prosthesis was done by simple downward pressure through choledochotomy until it determined that sufficient length has been inserted. Correct transpapillary placement was ensured by transcholedochal choledochoscopy, checking that the final tab of the prosthesis was not visible at the papilla and that, therefore, it was located on the duodenal side. The prosthesis was removed by endoscopy 1 month after surgery if spontaneous elimination had not occurred. In the last 3 years of the series, preference was given to performing a primary choledochorrhaphy with continuous 4–0 monofilament suture to eliminate the complications related to the prosthesis and the discomfort of its removal.
Since 2010, with the experience gained after its use as a biliary sealant in liver surgery, a fibrin-collagen patch has been selectively applied as a biliary sealant (Tachosil®), at the surgeon's discretion, covering the choledochorrhaphy. For placement, the sheet was folded before insertion, pulled through a trocar and expanded and applied over the suture line. Subsequently the patch was pressed with a wet gauze for 3min to ensure its fixation. The surgical procedure ended with cholecystectomy and the placement of a suction drainage to monitor the appearance of biliary fistulae. Hospital discharge occurred 48h after surgery once the absence of complications had been confirmed. In the case of the appearance of biliary discharge, confirmed by biochemistry, the drain tube was maintained until the closure of the biliary fistula.
Variables of the AnalysisThe study population was divided into two groups according to whether a collagen-fibrin patch had been used to cover the choledochorrhaphy (patch group, PG) or the suture had been left uncovered (no patch group, NPG). The homogeneity of the groups was studied for the following variables: age, sex, body mass index, anesthetic risk, history of abdominal surgery, conversion to open surgery, diameter of the bile duct, presence of preoperative jaundice, number of stones extracted, presence of impacted lithiasis and extraction method. The incidence of postoperative biliary fistulae was analyzed in both groups (defined according to the criteria of the International Study Group of Liver Surgery as the presence of bilirubin levels three times higher than the blood values measured in the drained discharge from the third postoperative day or later, or the need for percutaneous or surgical drainage of bile collections28). Subsequently, the sample was stratified into two subgroups according to the bile duct closure technique used: choledochorrhaphy with transpapillary stent (CS) or primary choledochorrhaphy (PC). The incidence of biliary fistulae was analyzed in each according to whether they belonged to the PG or the NPG. We recorded the complications of each group according to the Dindo-Clavien classification,29,30 average hospital stay and need for readmission and reoperation.
Statistical AnalysisQuantitative values were expressed with measures of central tendency, determining the median and range. Categorical variables were recorded with absolute frequencies and percentages. The existence of significant differences between the two study groups was determined by the chi-square test for qualitative variables and the non-parametric Mann–Whitney test for quantitative variables. The odds ratio for the biliary fistula variable in both study groups was calculated. A P-value <.05 was considered statistically significant. The statistical analysis was performed using the SPSS statistical program for Mac v.20.
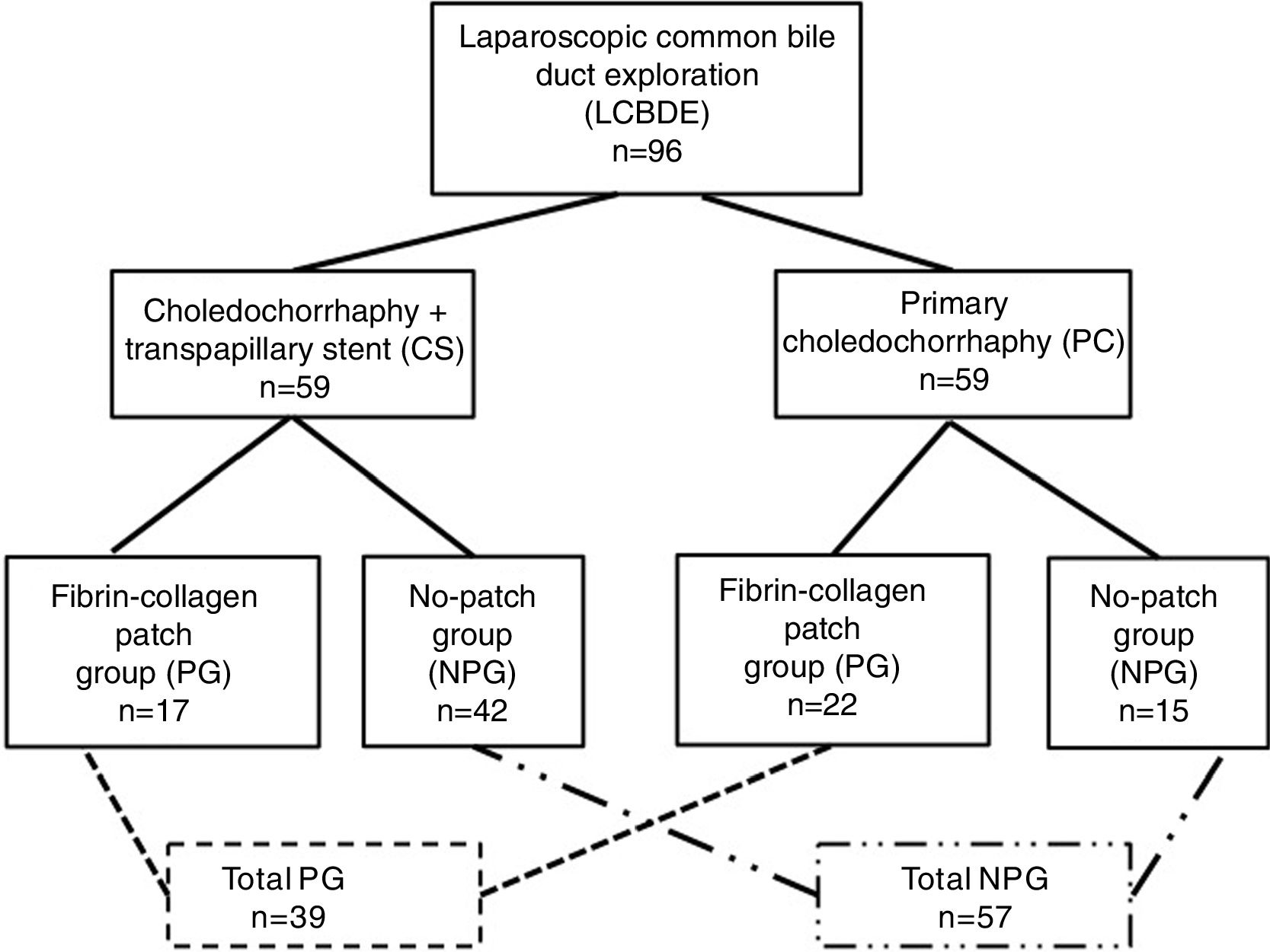
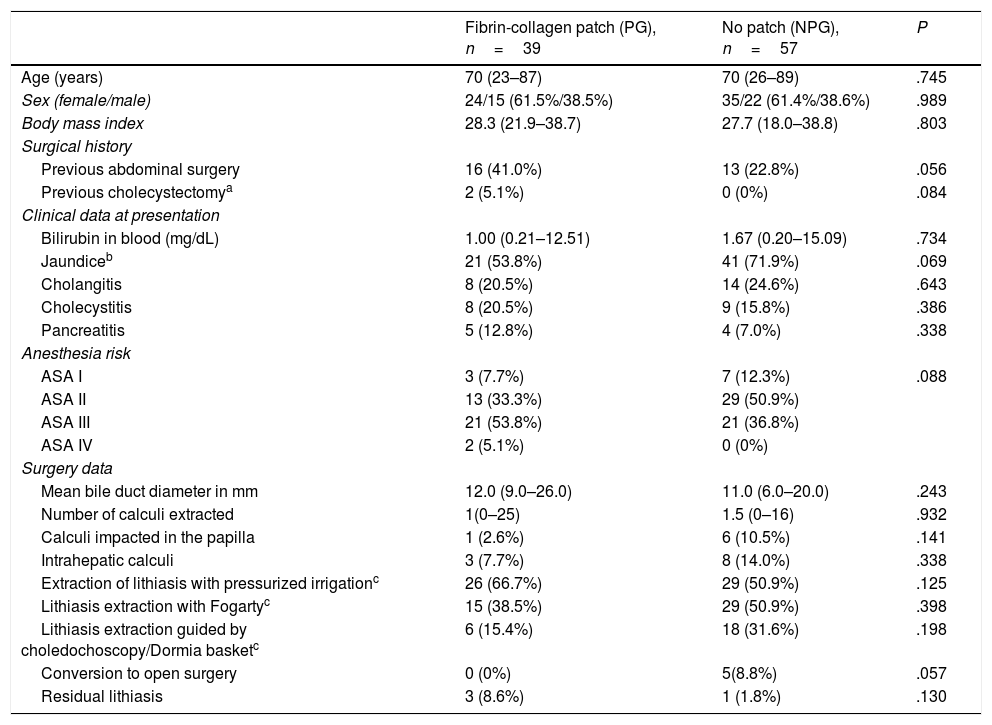
ResultsDuring the study period, 39 patients (41%) were treated with a fibrin-collagen patch (PG), and 57 patients (59%) were not (NPG). Twenty-two patients of the PG (56%) underwent PC, while 17 patients (44%) received a CS. In the NPG, 15 patients had undergone PC (26%), and CS was used in 42 (7%). Fig. 1 shows the distribution of groups and Table 1 the clinical characteristics of the patients in the study groups.
Perioperative Patient Data From the Two Study Groups.
| Fibrin-collagen patch (PG), n=39 | No patch (NPG), n=57 | P | |
|---|---|---|---|
| Age (years) | 70 (23–87) | 70 (26–89) | .745 |
| Sex (female/male) | 24/15 (61.5%/38.5%) | 35/22 (61.4%/38.6%) | .989 |
| Body mass index | 28.3 (21.9–38.7) | 27.7 (18.0–38.8) | .803 |
| Surgical history | |||
| Previous abdominal surgery | 16 (41.0%) | 13 (22.8%) | .056 |
| Previous cholecystectomya | 2 (5.1%) | 0 (0%) | .084 |
| Clinical data at presentation | |||
| Bilirubin in blood (mg/dL) | 1.00 (0.21–12.51) | 1.67 (0.20–15.09) | .734 |
| Jaundiceb | 21 (53.8%) | 41 (71.9%) | .069 |
| Cholangitis | 8 (20.5%) | 14 (24.6%) | .643 |
| Cholecystitis | 8 (20.5%) | 9 (15.8%) | .386 |
| Pancreatitis | 5 (12.8%) | 4 (7.0%) | .338 |
| Anesthesia risk | |||
| ASA I | 3 (7.7%) | 7 (12.3%) | .088 |
| ASA II | 13 (33.3%) | 29 (50.9%) | |
| ASA III | 21 (53.8%) | 21 (36.8%) | |
| ASA IV | 2 (5.1%) | 0 (0%) | |
| Surgery data | |||
| Mean bile duct diameter in mm | 12.0 (9.0–26.0) | 11.0 (6.0–20.0) | .243 |
| Number of calculi extracted | 1(0–25) | 1.5 (0–16) | .932 |
| Calculi impacted in the papilla | 1 (2.6%) | 6 (10.5%) | .141 |
| Intrahepatic calculi | 3 (7.7%) | 8 (14.0%) | .338 |
| Extraction of lithiasis with pressurized irrigationc | 26 (66.7%) | 29 (50.9%) | .125 |
| Lithiasis extraction with Fogartyc | 15 (38.5%) | 29 (50.9%) | .398 |
| Lithiasis extraction guided by choledochoscopy/Dormia basketc | 6 (15.4%) | 18 (31.6%) | .198 |
| Conversion to open surgery | 0 (0%) | 5(8.8%) | .057 |
| Residual lithiasis | 3 (8.6%) | 1 (1.8%) | .130 |
The quantitative variables are expressed as median and range, and the qualitative variables as absolute frequency and percentage.
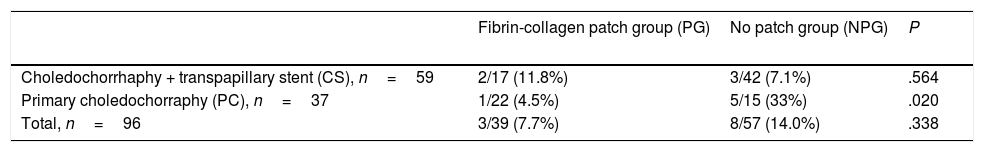
The incidence of biliary fistulae was 7.7% (three patients) in the PG and 14% (eight patients) in the NPG, although only one of the fistulae detected in the entire series, which appeared in a PG patient, was type C. In spite of the difference detected between the two groups, this was not statistically significant (P=.338). However, when the effect of the sealant was analyzed within each choledochorrhaphy subgroup, it was detected that the application of the fibrin-collagen sponge reduced the incidence of biliary fistulae in the PC group (4.5% in the PG vs 33% in the NPG, P=.020), but not in the transpapillary stent group (CS) (11.8% in the PG vs 7.1% in the NPG, P=.564) (Table 2). Within the PC group, the fibrin patch proved to be a protective factor, with an odds ratio of 10.5 (confidence limit, 1.08–102.17).
Incidence of Bile Leaks in the Study Groups.
| Fibrin-collagen patch group (PG) | No patch group (NPG) | P | |
|---|---|---|---|
| Choledochorrhaphy + transpapillary stent (CS), n=59 | 2/17 (11.8%) | 3/42 (7.1%) | .564 |
| Primary choledochorraphy (PC), n=37 | 1/22 (4.5%) | 5/15 (33%) | .020 |
| Total, n=96 | 3/39 (7.7%) | 8/57 (14.0%) | .338 |
Qualitative variables are expressed as absolute frequency and percentage.
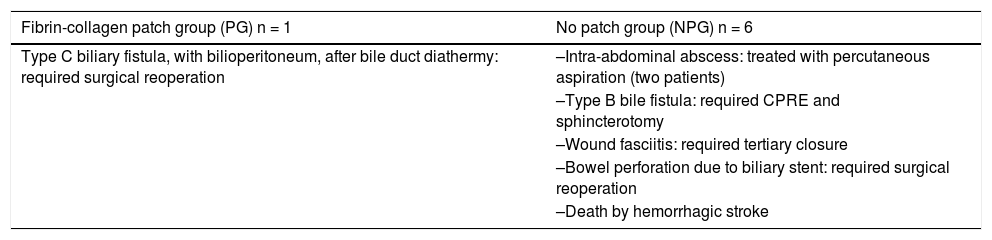
Major complications (Dindo-Clavien≥3) appeared in one patient (2.6%) of the PG and in six patients (10.5%) of the NPG (P=.141). One patient in each group was reoperated, due to a type C biliary fistula in the PG and intestinal perforation of a migrated stent after several months in the NPG. There was no mortality related to the technique, although one patient died on the second postoperative day due to a hemorrhagic stroke. Major complications are shown in Table 3. The hospital stay was significantly shorter for the PG, with a median of 3 days (range 2–57), compared to the NPG, with a median of 4 (range 1–30) and a P-value=.008. The need for hospital re-admission after LCBDE was not different between the two study groups (2.6% [one patient] in PG vs 3.5% [two patients] in the NPG, P=.794).
Major Complications (Dindo-Clavien≥3) in the Study Groups.
| Fibrin-collagen patch group (PG) n = 1 | No patch group (NPG) n = 6 |
|---|---|
| Type C biliary fistula, with bilioperitoneum, after bile duct diathermy: required surgical reoperation | –Intra-abdominal abscess: treated with percutaneous aspiration (two patients) |
| –Type B bile fistula: required CPRE and sphincterotomy | |
| –Wound fasciitis: required tertiary closure | |
| –Bowel perforation due to biliary stent: required surgical reoperation | |
| –Death by hemorrhagic stroke |
Complications caused by stent migration 1 month after LCBDE that required CPRE for extraction instead of endoscopy were not included in this comparison.
Stent-related complications appeared after discharge in six patients (10.2%). Two of these patients belonged to PG and four to NPG. Stent migration to the bile duct occurred in five cases, requiring ERCP instead of a simple upper endoscopy for its extraction. A sixth patient had to undergo surgery for a late-onset intestinal perforation a few months after LCBDE. In this case, the spontaneous elimination of the prosthesis toward the jejunum prevented its endoscopic removal. However, intra-abdominal adhesions following a previous surgery had transfixed the loops, impeding evacuation of the stent through the digestive tract and causing the perforation.
DiscussionAt present, it has been sufficiently demonstrated that LCBDE is as effective as ERCP+LC for the treatment of choledocholithiasis and that both share a similar rate of complications; neither approach is superior to the other.1,13–16 In spite of this, in most hospitals, the endoscopic approach is chosen for the treatment of patients with bile duct lithiasis. A recent study of a national survey conducted in the United States showed that 86% of surgeons chose to perform ERCP and a subsequent LC for the treatment of choledocholithiasis.5 Among the reasons for not choosing the completely laparoscopic approach, the respondents argued the easy availability of expert endoscopists (which should not be a reason if the surgeon was an expert in LCBDE), the lack of necessary equipment (not really different from that used during LC, except for the choledochoscope, which is not absolutely essential), but above all the fact of not being comfortable with the LCBDE technique. Specifically, the difficulty in achieving a hermetic closure of the bile duct by laparoscopy without causing stenosis is one of the greatest difficulties faced by the surgeons who select this approach. Despite the fact that the abandonment of the Kehr tube has brought advantages such as reducing the morbidity of LCBDE,17,20,31 the incidence of biliary fistulae after laparoscopic choledochotomy and choledochorrhaphy continues to be between 5 and 15% of patients.20 Our study concurs with these data, providing global figures for biliary fistula of 11.5%. Only one of our patients developed a C-type fistula that required reoperation, and most cases of B-type fistula were due to the persistence of the biliary discharge beyond 1 week and not to the need for therapeutic intervention. Despite this, the appearance of a biliary fistula after LCBDE remains one of the problems of this surgery to be resolved. With this objective, the technique of choledochorrhaphy protected by transpapillary stent was introduced, with good results,19,32 arguing that the reduction of intrabiliary pressure that is achieved by maintaining the papilla open with the stent should reduce the bile filtrate through the choledochal suture. Nonetheless, as we showed in our series, the prosthesis itself can be a cause of morbidity, in addition to the discomfort that an endoscopy causes the patient for its removal.
The use of fibrin sponges as hemostatic agents has been known since the 1990s,33 and since then their use has been widespread to achieve hemostasis of solid organs with diffuse bleeding.24,25 At the same time, it has been proved that the presence of collagen adds sealing capacity to the patch, enabling the closure of aerial, biliary, lymphatic and cerebrospinal fluid fistulae.23 The combination of hemostatic effects and biliary sealing began to be of special interest in liver surgery.27,34 Although there are studies that reveal the fibrinolytic capacity of bile in vitro, theoretically affecting the integrity of the fibrin-collagen patches,35 a recent study has been published that demonstrates the reduction of biliary fistulae after split-liver transplantation in adults with the use of these sponges.26 Although the effect of biliary sealing should be as effective after choledochorrhaphy in LCBDE, only animal studies have shown good results for this indication, there being no published experience in humans. At our hospital, while the use of the fibrin-collagen sponge was introduced in hepatic surgery, it began to be used in 2010 to protect the choledochorraphy of biliary fistulae. Our results show that its application managed to reduce the number of fistulae in the global series by half, although only at the expense of patients who did not receive transpapillary stents. In the absence of biliary hyperpressure, keeping the papilla open by means of plastic stents, adding sealants to the choledochorraphy, does not offer any benefit. On the other hand, after a primary choledochorrhaphy, this increase in biliary pressure with the closed papilla seems to be better supported by the application of fibrin-collagen sealants, significantly decreasing the incidence of biliary fistulae. It is evident that, with equal results for the appearance of fistulae, primary closure of the common bile duct offers advantages over the stent-protected closure, given the morbidity associated with stents and their removal. In addition, the increase in costs derived from the use of fibrin-collagen sealants could be compensated by a reduction in overall hospital stay as a consequence of the lower morbidity detected. Although our study has the bias of being a retrospective study in which the use of the sealants and the type of choledochorrhaphy has not been protocolized, it is the first study in humans that describes the beneficial sealing effect of the fibrin-collagen patch used on the bile duct. Until the publication of randomized clinical trials with larger sample sizes that may contribute more evidence, we believe that the most appropriate choledochotomy closure technique after LCBDE is primary choledochorrhaphy protected with a fibrin-collagen sponge.
FundingThe authors have received no funding in order to conduct this study, or in the composition and publication of the manuscript.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Parra-Membrives P, Martínez-Baena D, Lorente-Herce JM, Martín-Balbuena R. Eficacia del sellante de fibrina-colágeno para reducir la incidencia de fístulas biliares tras la exploración laparoscópica de la vía biliar. Cir Esp. 2018;96:429–435.