The presence of an ureteroiliac fistula (UIF) is an unusual cause of hematuria that should be suspected in patients with a history of pelvic surgery, arterial revascularization, pelvic inflammatory processes, radiotherapy or ureteral stent placement1; occasionally, it is also associated with the presence of an arterial pseudoaneurysm. One of the greatest advantages of endovascular procedures is the rapid control of bleeding with minimally invasive techniques.
We present the case of a 53-year-old male with a history of dyslipidemia, peritonitis due to acute gangrenous appendicitis requiring laparoscopic appendectomy, and bladder cancer treated by transurethral resection and endocavitary chemotherapy. Three years later, he presented recurrence of said neoplasm with infiltration of the ureteral wall and meatus, lymph node involvement and bone metastases (invasive bladder cancer pT4 pN3 M1). The patient was treated surgically by the urology department, who performed radical cystectomy associated with extended bilateral iliac lymphadenectomy and cutaneous ureterostomy. The patient also required palliative chemotherapy.
One month later, the patient came to the emergency department due to colicky pain in the left iliac fossa and bleeding through the ureterostomy. The interventional radiology unit injected iodinated contrast through the ureteral catheter, observing the presence of a left UIF, which they treated with the placement of 2 Fluency® (Bard) 8×60mm coated stents. Six months later, the patient once again presented the same symptoms. Computed tomographic (CT) angiography demonstrated a proximal leak of contrast material from the stents. The patient was again treated by the interventional radiology unit with the placement of another 8×60mm Fluency® stent.
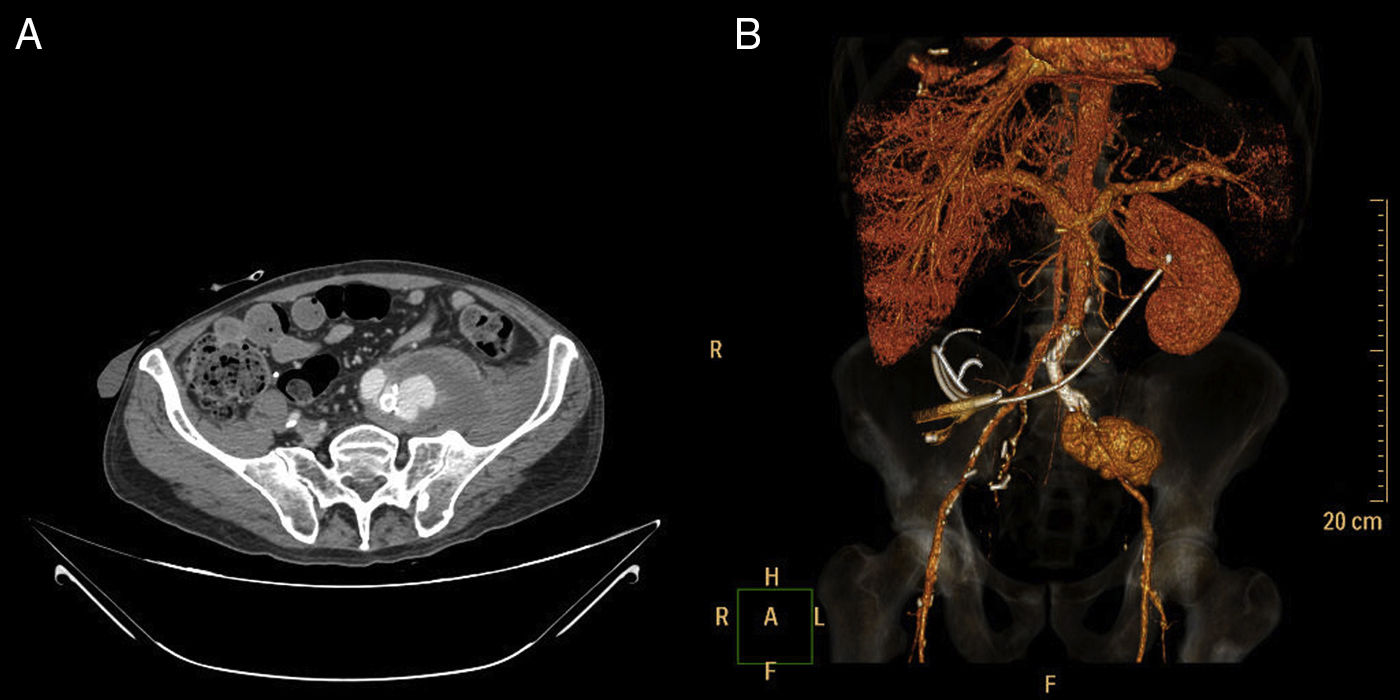
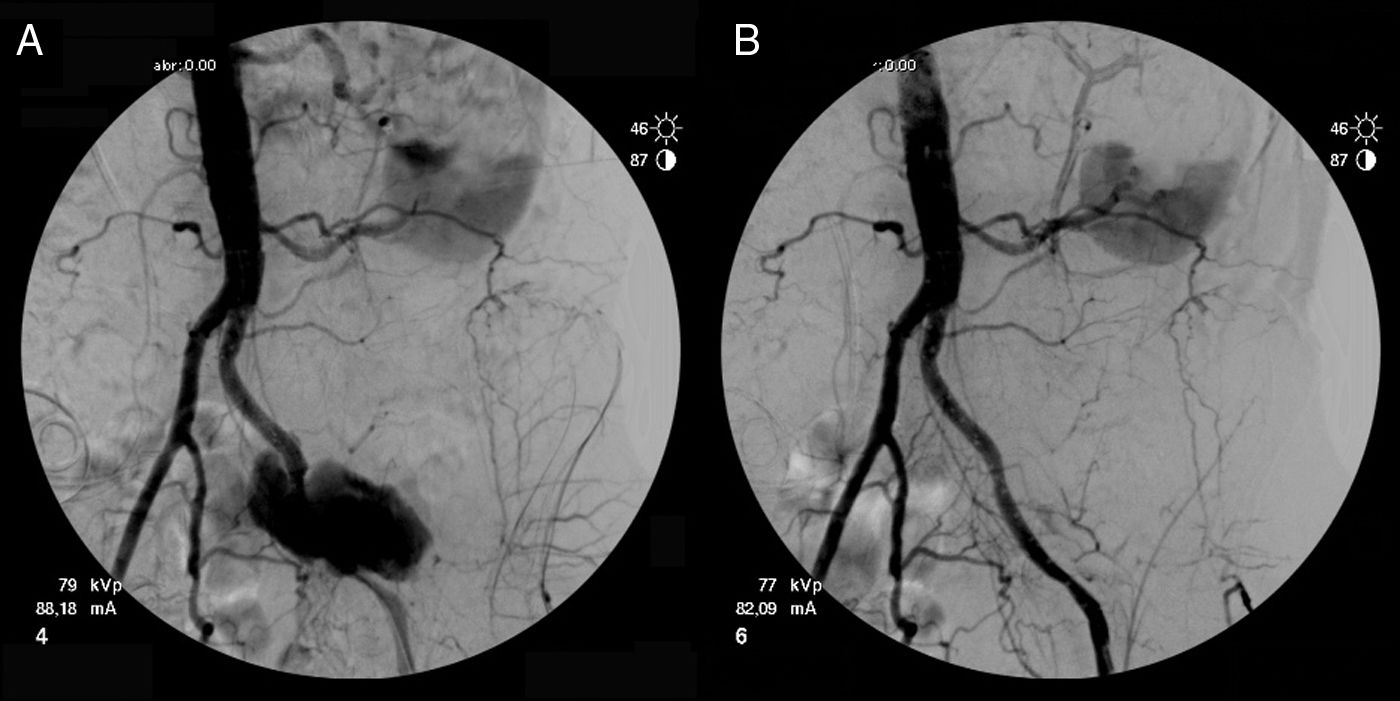
Two months later, the patient came to the emergency department again due to intense pain in the left hemiabdomen and thigh, which required the extremity to be maintained in flexion. CT angiography revealed a left common iliac pseudoaneurysm with a maximum diameter of 65mm and active bleeding (Fig. 1A and B), so the patient was referred to our service. Given the patient's surgical history and high risk, we opted for endovascular treatment, reserving open surgery for use as a last resort. Due to the antalgic position of the limb, the procedure had to be done under general anesthesia. Using left retrograde femoral puncture and following Seldinger's technique, a diagnostic arteriography was performed through a 6 Fr introducer sheath, which revealed a contrast leak through the distal portion of the previously placed endoprostheses (Fig. 2A). With the help of a 0.035inch hydrophilic guidewire and through a Vanschie II type catheter, the common iliac artery was canalized and 2 Fluency® coated stents were implanted (10×80mm and 8×80mm). As a prophylactic measure, 1.5g of cefuroxime was administered according to protocol, and no anticoagulation therapy was applied due to the active bleeding.
The postoperative angiographic study confirmed the cessation of bleeding and the permeability of the iliac axis (Fig. 2B). The postoperative evolution was satisfactory, with no new episodes of hematuria.
The increased risk factors and the longer survival of patients with genitourinary neoplasms have increased the incidence of UIF in the recent literature, although it is still uncommon.2
In chronic inflammatory processes, fibrosis and precarious vascularization of the vasa vasorum create an adhesion between the ureter and artery, which is the main cause of the formation of fistulae. These are mainly located in the iliac axis, with a preference for the external iliac artery, and can be associated with abscesses or pseudoaneurysms.3 The latter are formed by localized arterial rupture with extravasation of blood encompassed by the layers of connective tissue.4 The persistence of the leak point makes them pulsatile, and the pseudoaneurysm may grow until it ruptures.5
UIF should be suspected in a patient with severe or microscopic hematuria over the course of several days and risk factors due to previous surgeries or inflammatory processes.6 In addition to hematuria, the patient may present with lumbar pain, urinary retention or infection. Pain in the flank may be secondary to obstruction of the ureter due to blood clotting2 or the rupture of a pseudoaneurysm.
The technique of choice for the diagnosis of UIF is selective arteriography, as it identifies the exact location of the fistula.5,7 Meanwhile, CT angiography is selected for the diagnosis of a pseudoaneurysm as it offers preoperative information about possible rupture, size and relationship with neighboring structures.8
Classically, surgical repair of a UIF involves femorofemoral crossover bypass with exclusion of the affected iliac artery (embolization or ligation), or less frequently in situ reconstruction. Endovascular treatment with the placement of coated stents is a minimally invasive alternative that provides quick control of the bleeding and clear advantages in patients with unfavorable anatomy. The selection of patients for one procedure or another is based on comorbidity, clinical presentation, anatomical difficulties, presence of infection, enteric contamination or the need to preserve pelvic perfusion due to contralateral arterial disease.7
Although the risk of infection and recurrence of bleeding are not well defined, these procedures are safe and effective, although not free from complications that may become severe in certain cases.
Please cite this article as: Miguel-Sánchez AM, Sarmiento-Marasovic L, Buisán-Bardají JM, Coghi-Granados J, Duato Jané Á. Reparación endovascular de seudoaneurisma arterial secundario a fístula ilíaco-ureteral. Cir Esp. 2018;96:123–125.