Rupture of abdominal aortic aneurysm is still a difficult challenge for the vascular surgeon due to the high perioperative mortality. The aim of our study is to describe the characteristics of the population as well as to compare morbidity and mortality in patients undergoing open surgery or endovascular repair in our center.
MethodsDatabase with 82 rAAA between January 2002 and December 2014, studying two cohorts, open surgery and endovascular repair. Epidemiologic, clinical, surgical techniques, perioperative mortality and complications are analyzed.
ResultsEighty-two rAAA cases were operated (men: 80, women: 2). Mean age 72±9.6 years. 76.8% (63 cases) was performed by open surgery.
Backgroundsmokers 59, 7%, alcoholism 19.5%, DM 10.9%, AHT: 53.6%, dyslipidemia 30.5%. The most frequent clinical presentation was abdominal pain with lumbar irradiation: 50 cases (20.7% associating syncope). Overall hospital mortality was 58.5%. Hemodynamic shock prior to intervention was associated with increased mortality (P<.001). Anemia, leukocytosis, aneurysm size, sex and age did not show a statistically significant difference with respect to mortality (P>.05). The presence of iliac aneurysms was associated with increased mortality (P<.0045). Perioperative mortality in endovascular repair was 42%, and in open surgery was 63.5% (P>.05). Hospital stay was lower in the endovascular group (P=.3859).
ConclusionsHemodynamic shock and the presence of concomitant iliac aneurysms have a statistically significant association with perioperative mortality in both groups. We found clinically significant differences in mortality, complications and hospital stay when comparing both groups with better results for EVAR, without statistically significant differences.
La rotura del aneurisma aórtico (AAAr) continúa siendo un reto para el cirujano, presentando una alta mortalidad perioperatoria. El objetivo de nuestro estudio es describir el tipo de población afectada comparando mortalidad y complicaciones en pacientes intervenidos mediante cirugía abierta y reparación endovascular (REVAr) en nuestro centro.
MétodosBase de datos con 82 AAAr intervenidos entre enero de 2002-diciembre de 2014, estudiándose 2 cohortes, una intervenida mediante cirugía abierta y otra con REVAr. Se analizan variables demográficas, clínicas, técnicas quirúrgicas, complicaciones y mortalidad perioperatorias.
ResultadosOchenta y dos casos de AAAr intervenidos (varones: 80, mujeres: 2). Edad media 72±9,6 años. El 76,8% se realizó mediante cirugía abierta. Antecedentes: tabaco: 59,7%, alcoholismo: 19,5%, DM: 10,9%, HTA: 53,6%, dislipemia 30,5%. La clínica de presentación más frecuente fue dolor abdominal con irradiación lumbar: 71,9% (asociando síncope 20,7%). Mortalidad intrahospitalaria global 58,5%. El shock hemodinámico previo a intervención se asocia a una mayor mortalidad (p<0,001). La anemia, leucocitosis, antecedentes médicos, tamaño aneurismático, sexo y edad no muestran asociación significativa con respecto a la mortalidad (p>0,05). La presencia de aneurismas iliacos se asocia a mayor mortalidad (p=0,0045). Mortalidad perioperatoria para REVAr: 42%, y en cirugía: 63,5% (p>0,05). Estancia media menor en el grupo de REVAr (p>0,05).
ConclusionesEl shock hemodinámico y la presencia de aneurismas iliacos parecen asociarse a una mayor mortalidad en ambos grupos. Encontramos diferencias clínicamente significativas en cuanto a mortalidad, complicaciones y estancia hospitalaria al comparar ambos grupos con mejores resultados para EVAR, sin embargo no son estadísticamente significativas.
Ruptured infrarenal abdominal aortic aneurysm (AAAr) continues to be a challenge for vascular surgeons in the emergency setting. Open surgery (OS) has been the treatment of choice for decades,1,2 with associated mortality rates of 32%–70% according to different publications. However, these results have not improved over the years.3–5 Furthermore, this procedure entails a large number of perioperative complications, most importantly total ischemia caused by hemodynamic shock, which later leads to multiple organ failure.6,7
The introduction of endovascular aneurysm repair (EVAR) by Yusuf in 1994 for the treatment of AAAr was an important innovation that gave rise to several studies showing better results and supporting the use of this technique, with reported perioperative mortality rates from 5% to 35%.8 In recent years, EVAR has become the treatment of choice, and the current trend is to use this method whenever possible.1,3,5
Endovascular therapy has many advantages over OS, such as the possibility to perform the procedure under local anesthesia, the absence of aortic clamping and therefore reperfusion syndrome, less blood loss and reduced hypothermia.9
Nonetheless, EVAR also has several disadvantages when compared to open surgery. First is the need for a CT scan with contrast for the anatomical evaluation of the aneurysm, its relationship with the renal arteries and the iliac morphology. Patients must be hemodynamically stable to withstand the time required for the imaging test and preoperative preparation for the procedure, which is longer in endovascular therapy.1,6 It is also necessary to have a trained multidisciplinary team available that includes surgeons, radiologists, nurses, anesthesiologists, radiology technicians, etc., as well as the adequate materials for each case and a properly equipped operating room.4 Likewise, EVAR requires closer long-term patient follow-up because late complications are more frequent, such as endoleaks (with aneurysmal sac growth) and migration.5
The aortic morphology must also meet the appropriate anatomical conditions to perform the endovascular procedure, which is defined in its instructions for use. The proportion of infrarenal abdominal aortic aneurysms (AAA) that are treatable by EVAR is 47%–67%. If the intervention is conducted outside the defined instructions, there is a high risk of early type I endoleaks, migrations and reoperations.2 Patients who have undergone open surgery have much more serious immediate complications, such as bleeding, sigmoid ischemia and cardiopulmonary disease, while the development of late complications is exceptional.7
Our objective is to describe the global sample of patients treated at our hospital with AAAr, their demographic and medical characteristics, factors that may be involved in a poorer prognosis, and overall morbidity and mortality. In addition, we will compare the prognoses between the EVAR and open surgery groups in terms of mortality, hospital stay and postoperative complications.
MethodsThe study was conducted at the Hospital Universitario in León, Spain, which is a tertiary hospital that provides treatment for Angiology and Vascular Surgery pathologies to a population of approximately 485000 inhabitants.
We designed an analytical and descriptive observational study including all patients diagnosed with ruptured infrarenal abdominal aneurysm who were alive upon entrance to the operating room. Aneurysmal rupture was defined by hemorrhage outside the aortic wall on imaging tests or by direct observation after laparotomy. CT angiography was performed in those patients who were hemodynamically stable or moderately unstable, with blood pressures between 60 and 100mmHg and a good maintained level of consciousness. We considered the patients to be hemodynamically unstable when they presented diastolic pressures lower than 60mmHg, reduced level of consciousness or associated cardiac alterations.
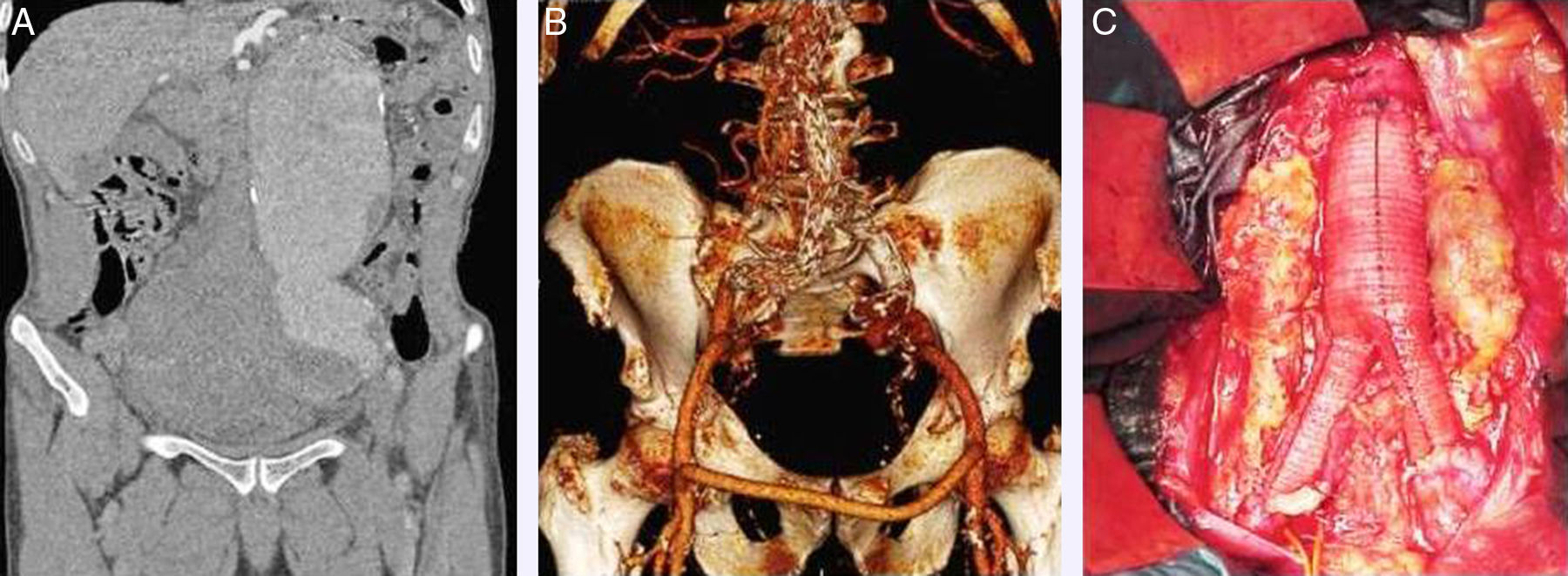
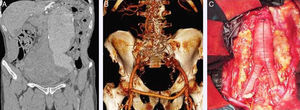
The study period was 12 years, from January 2002 to December 2014. To obtain data, medical records were reviewed. We studied 82 cases in total, divided into two cohorts: one for AAAr treated with the EVAR approach, and another for patients who underwent open surgery. The type of intervention was decided according to patient characteristics, anatomy of the aneurysm and the preferences of the surgeon (Fig. 1).
(A) CT angiography image, showing ruptured infrarenal abdominal aorta aneurysm associated with left iliac aneurism; (B) CT angiography showing the correct placement of an aortouniiliac EVAR stent associated with femorofemoral bypass; (C) open surgery with resection of the aneurysm and aortobiiliac graft.
The variables studied were the following:
- •
Patient demographic characteristics: age and sex
- •
Medical history of interest: smoking, ischemic heart disease, renal failure, arterial hypertension, chronic obstructive pulmonary disease, diabetes mellitus, hypercholesterolemia, cerebrovascular disease
- •
Symptoms at presentation: lumbar pain, abdominal pain, syncope, cardiorespiratory arrest, asthenia, nausea and/or vomiting and combinations
- •
Presence of concomitant iliac aneurysms
- •
Surgical techniques used
- •
Global mortality rates, divided according to chronology and origin (immediate post-op <24h, time in recovery unit and hospitalization time)
- •
Preoperative conditions that could influence prognosis (measured in mortality rates): presence of hemodynamic instability, defined as a systolic blood pressure lower than 90mmHg or clinical signs of shock (presence of oliguria or anuria, paleness, altered state of consciousness), hemoglobin below 8g/dL, presence of chronic kidney disease, ischemic heart disease, smoking, COPD and peripheral artery disease
A descriptive analysis was completed of the global sample for the variables studies, using measures of central tendency. Both groups were compared in terms of mortality rates and associated postoperative complications.
Statistical AnalysisThe statistical analysis was calculated with the G-STAT 2.0-X2 program. The comparative statistical method involved a chi-squared test, and P<.05 was considered significant.
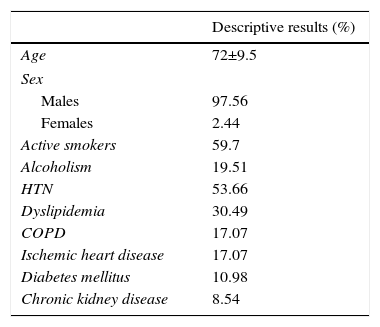
ResultsIn the study period mentioned, we identified 82 patients with AAAr (80 males and 2 females). Mean age was 72±9.5, ranging from 47 to 90 years; 59.7% were active smokers, and 19.51% had a history of alcoholism, all of whom were smokers.
With regard to the medical history of interest, we found 53.66% had arterial hypertension, 30.49% dyslipidemia, 17.07% COPD, 17.07% ischemic heart disease, 10.98% diabetes mellitus, and 8.54% chronic kidney disease (Table 1).
The most frequent symptoms at presentation were abdominal pain in 71.95%, associated with syncope in 20.73%, 20.73% lumbar pain, and vomiting in 19.51%. Pure lumbar pain was seen in 19.51%; 6.09% presented with cardiorespiratory arrest, and 2.43% with fever and a state of general malaise.
The presence of concomitant iliac aneurysms was observed in 32.93%.
The surgical techniques used were EVAR in 23.17% and open surgery in 76.83%. Endovascular repair was conducted in all cases with aortouniiliac stent by Medtronic (Dublin), along with femorofemoral crossover bypass. The procedures were done under general anesthesia.
The open surgical techniques were: aortobifemoral graft, 36.59%; aorto-aortic graft, 30.79%; and aortoiliac graft, 9.76% of all AAAr.
Overall perioperative mortality (<30 days) was 58.41%, most of which was during the immediate postoperative period (less than 24h) in 48%, in the recovery unit in 37% and in the hospital ward in 15%.
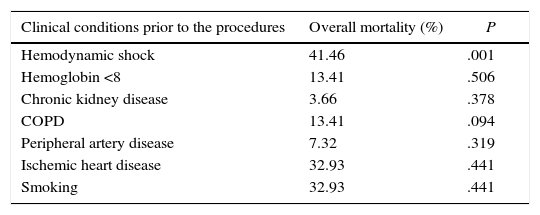
In our study, 70.82% of the deceased patients had hemodynamic shock prior to intervention (P<.05). Increased mortality did not significantly correlate with the presence of anemia, chronic kidney disease, COPD, chronic ischemic heart disease or smoking (Table 2).
Clinical Conditions Prior to the Procedures in Terms of Overall Mortality.
| Clinical conditions prior to the procedures | Overall mortality (%) | P |
|---|---|---|
| Hemodynamic shock | 41.46 | .001 |
| Hemoglobin <8 | 13.41 | .506 |
| Chronic kidney disease | 3.66 | .378 |
| COPD | 13.41 | .094 |
| Peripheral artery disease | 7.32 | .319 |
| Ischemic heart disease | 32.93 | .441 |
| Smoking | 32.93 | .441 |
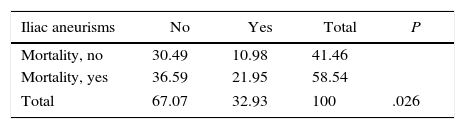
The presence of concomitant iliac aneurysms seemed to be associated with higher mortality (P<.05). Out of the 27 patients with associated concomitant iliac aneurysms, 66.7% died (Table 3).
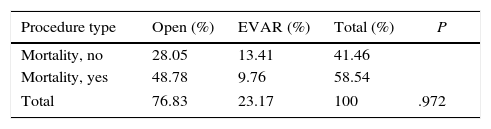
When analyzing the associated mortality according to the type of intervention, we observed that the mortality rate was higher in the open surgery group. Out of the deceased patients, 83.33% belong to the open surgery group. In contrast, there was a 16.67% mortality rate associated with the endovascular therapy group. However, although the mortality results were clearly superior in the open surgery group, this percentage was not statistically significant, with a P>.05 (Table 4).
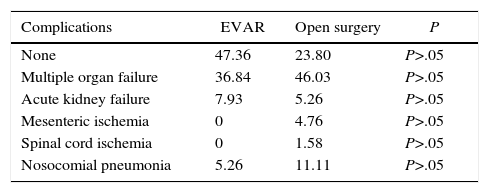
The comparison of the results between the two groups in terms of complications obtained a total absence of complications in the EVAR group of 47.36%, compared to 23.80% in the open surgery group. The percentage of multiple organ failure in the EVAR group was 36.84% versus 46.03% in the open surgery group. Nosocomial pneumonia was 5.26% in EVAR and 11.11% in surgery. Acute renal failure was 5.26% for EVAR and 7.93% for surgery. There was a total of 0% mesenteric ischemia in EVAR versus 4.76% in open surgery, and 0% spinal cord ischemia in the EVAR group compared to 1.58% in the surgery group (Table 5).
Postoperative Complications According to Type of Technique Used.
| Complications | EVAR | Open surgery | P |
|---|---|---|---|
| None | 47.36 | 23.80 | P>.05 |
| Multiple organ failure | 36.84 | 46.03 | P>.05 |
| Acute kidney failure | 7.93 | 5.26 | P>.05 |
| Mesenteric ischemia | 0 | 4.76 | P>.05 |
| Spinal cord ischemia | 0 | 1.58 | P>.05 |
| Nosocomial pneumonia | 5.26 | 11.11 | P>.05 |
As for the mean stay in the recovery unit, in the EVAR group this was 1.31±1.33 days and 4.28±6.29 days in the open surgery group (P>.05). Mean hospital stay was 9.36±8.80 day for the EVAR group and 12.50±14.41 days in the surgery group (P>.05).
DiscussionThe results of our study do not show statistically significant differences in favor of one or another technique in terms of mortality and complication rates. However, in percentage terms, we have obtained more favorable results for hospitalization in the critical care unit, hospital stay and postoperative complications in the endovascular therapy group. Recently, the IMPROVE-TRIAL (a randomized multicenter study of 613 patients comparing both strategies) has demonstrated that EVAR did not present lower 30-day mortality compared to OS. Nonetheless, as in our study, patients who had undergone EVAR had shorter stays in the critical care unit and hospital ward. In the systematic review by Antoniou et al., the results also supported the endovascular technique.
Of all the factors analyzed, only hemodynamic instability was associated with an increase in global mortality that was statistically significant, which seems logical. It would not be applicable to measure the association by groups, since a greater number of patients in poorer hemodynamic conditions are usually present in the OS group. We should consider that patients undergoing EVAR must be able to withstand the time required to perform a CT scan and for correct preparation and evaluation of the procedure. This datum may be an important confounding factor favoring EVAR, hence the importance of performing randomized studies to objectively compare both techniques.6–8 The same would occur with unfavorable aortic anatomies, as in the case of aneurysms with thrombi and calcium.
For many decades, open surgery has been the treatment of choice for ruptured abdominal aneurysm, with mortality rates around 50%.2 Many studies have concluded that endovascular therapy achieves lower short-term morbidity and mortality while reducing hospital stay, resuscitation unit stay and organ complications.1
Endovascular treatment seems to offer better results for short-term mortality (<30 days), although it is still unclear whether the figure is higher for long-term mortality.10 After the perioperative period, survival is equal for both groups, and cardiovascular events and cancer are the most common causes of death.11
On the other hand, several studies argue that endovascular therapy is associated with a greater number of reoperations in the long term and a need for an annual follow-up CT scans. The DREAM study is a randomized multicenter trial comparing the results obtained with EVAR versus OS in patients with abdominal aneurysm without rupture. This study concludes that the results of both techniques are similar, although a higher rate of reoperation is expected for the EVAR group. Our study is limited to the observation of immediate results (first 30 days), so a more extended study would be necessary to evaluate this question.
In our study, the presence of concomitant iliac aneurysms seems to show an increase in mortality rates, with a statistically significant association compared to patients without this presentation. This association has not been reported in the literature, and we think it may be due to the associated complexity of polyaneurysmal disease in both the scheduled and emergency treatment settings.
The most frequent clinical manifestation was abdominal pain, either associated or not with lower back pain, vomiting and hypotension. It is recommended to rule out this pathology in patients with compatible clinical conditions, especially in male smokers, over 65, with risk factors such as COPD and hypertension. The finding compatible with the exploration would be the presence of expansive aortic beat, and ultrasound should be the first screening test used.12
Our study has the limitation of being retrospective. Moreover, it presents a smaller sample of patients treated with endovascular therapy, because over the years the trend has been to perform most of the procedures using this technique, although years ago the open approach was most common. Therefore, the highest percentage of patients collected in our study who underwent endovascular therapy are from the most recent years, so it may also be biased for this reason.
The retrospective nature of the study, the small sample size of the series and the influence of technical learning on the new endovascular procedures and its recent introduction in the emergency setting may limit our observations, which are factors that should be analyzed by other groups. Like other current studies, patients were not randomized to create homogeneous groups, which could lead to selection bias as the sample of patients treated by open surgery were in worse condition before treatment.13
Randomized, observational studies with homogeneous samples are needed, where the most hemodynamically unstable patients are not included in the open surgery group, which may make the results significantly biased. However, such studies may not be feasible as many researchers would consider them unethical.
In our experience, the current trend in our department, as well as in many others that are equipped with material and trained personnel, is to perform endovascular therapy of ruptured abdominal aortic aneurysms whenever possible, providing that hemodynamic and anatomical conditions are favorable.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Novo Martínez GM, Ballesteros Pomar M, Menéndez Sánchez E, Santos Alcántara E, Rodríguez Fernández I, Zorita Calvo AM. Reparación endovascular versus cirugía abierta en el tratamiento de la rotura de aneurisma abdominal. Cir Esp. 2017;95:38–43.
Presented as an oral communication at the 61st Conference of the SEACV in Castellón, Spain (June 2–5, 2015).