Only 1% of the accidental ingestion of foreign bodies results in gastrointestinal perforation. Perforations by fish bones, often described in South East Asian populations, have the unusual characteristic of being paucisymptomatic until secondary complications occur. Fish-bone related intra-hepatic abscesses, although underreported and limited to isolated case reports, are rather unusual severe conditions and remain a therapeutic challenge. The main difficulty is to correlate the clinical picture of sepsis with both the intrahepatic abscess and the possibility of a foreign body. In all but two cases1,2 the piercing source reported has been found in the upper gastrointestinal tract, namely, the stomach and the duodenum. The fish-bone became embedded in the left lobe of the liver in most cases. The preoperative diagnosis is seldom made. The plain radiography is an unreliable tool in the diagnosis because fish-bones are usually not radio-opaque. Today, the extensive use of modern radioimaging by computed tomography scan (CT-Scan) has proved to be more helpful on the detection of ingested foreign bodies. Prompt recognition and early intervention are essential. If encapsulated abscess formations cannot be completely resolved by an interventional approach, a surgical procedure should be needed. Undiagnosed cases may result in recurrent liver abscess and sepsis and, sometimes, in the death of the patient. The mortality reported in a recent review was 17.6%.3
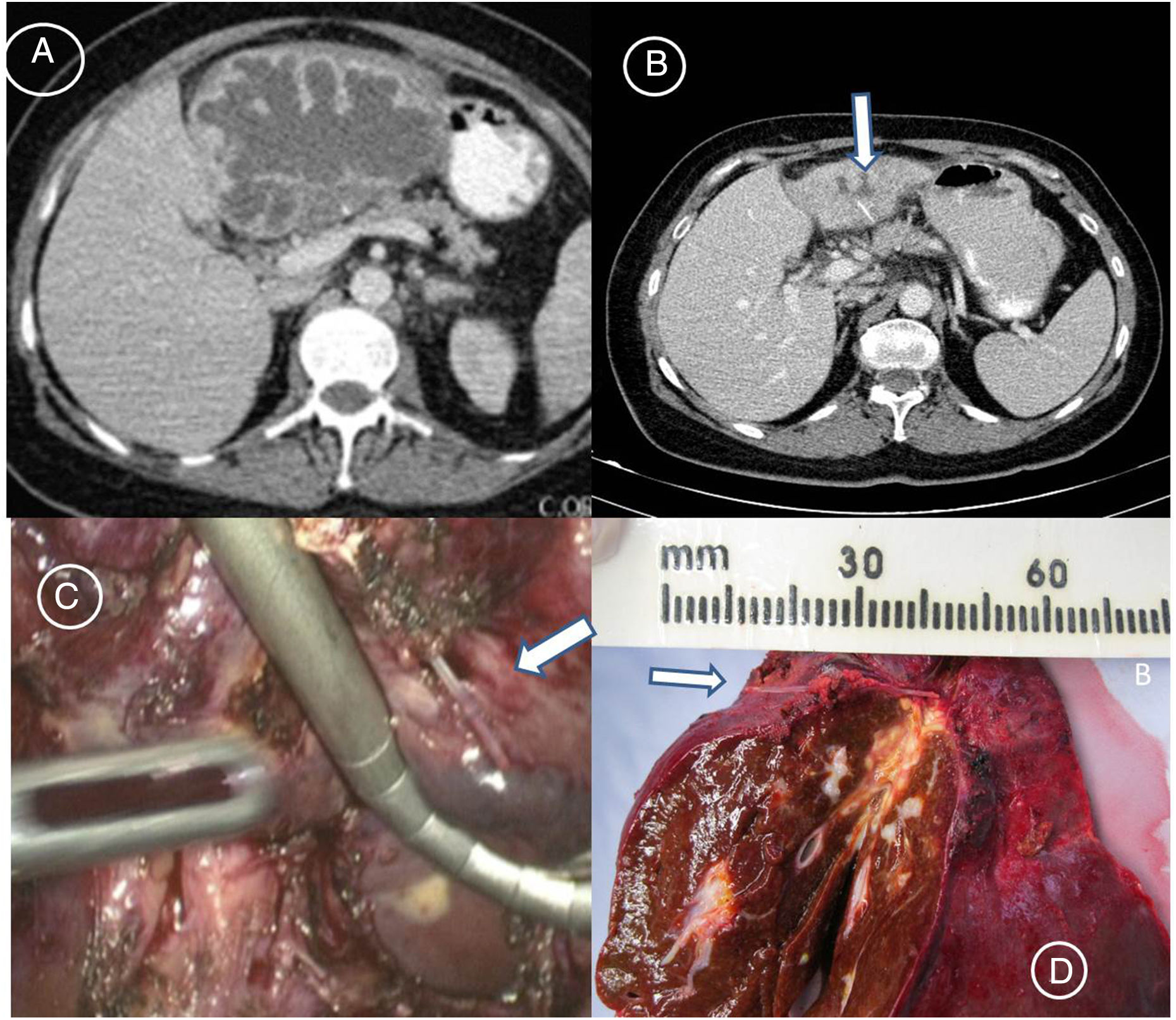
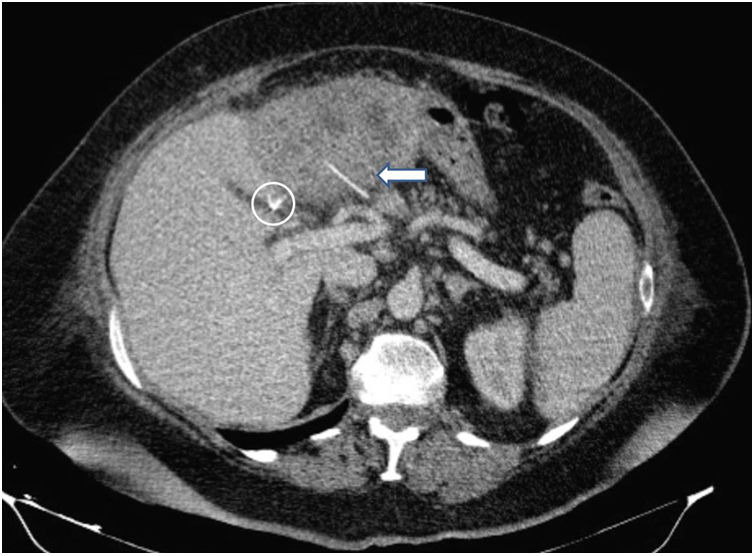
This scientific letter presents the cases of two patients satisfactorily treated in our Unit, as well as an updated review of the literature. Our first case was a 50-year-old woman who perfectly recalled the sequence of events from the unintentional ingestion of the foreign body to the development of liver complications. She started her family summer holidays celebrating the Festivity of Saint James’ day, the 25th of July, in Santiago de Compostela with a typical fish and seafood stew for dinner. She would never forget the severe epigastric pain and the horrible night she suffered, but as she did not want to interrupt her family's holidays, she treated herself with OmeprazolR twice a day and clear liquids for the next 3 days, and she improved progressively of her epigastric transfixive pain. She spent the rest of her holidays without any further symptomathology, and it was not until three weeks later that she needed urgent medical attention in our Hospital. She suffered from fever, shaking chills and shivering, persistent epigastric dullness and her temperature rose to 41°C. A CT-Scan revealed a hepatic abscess of unknown origin (Fig. 1A). She was treated percutaneously with abscess drainage and systemic antibiotics. But her encapsulated abscess formation could not be completely resolved. A new postdrainage CT-Scan showed an atrophic left hepatic lobe with a residual hepatic abscess and a high-density linear lesion inside (Fig. 1 B). Therefore, she underwent a laparoscopic left lateral liver bisegmentectomy (Segments II–III) (Fig. 1C). The vitreous foreign body, of about 2.5cm in length, which was extracted from the abscess cavity, turned out to be a fish-bone (Fig. 1D), which corresponded with the findings of the postdrainage CT-Scan referred to above. Her post-operative course was uneventful and the patient is doing well after her follow-ups 6 years later. Two years later a second female patient, 69-years-old, was referred to our Unit with a postcholecystectomy liver abscess. She had already undergone a laparoscopic cholecystectomy one month before for an “acute cholecystitis”. The CT-Scan that prompted her admission clearly showed a hepatic abscess in segment III with a high-density linear image that communicated with the hepatic abscess area (Fig. 2). Because of our previous experience with patient number one, we could quickly identify the origin of the disease, and make a preoperative diagnosis of a hepatic abscess due to a fish-bone. The patient was operated again, and an abscess drainage and the removal of the fish-bone were performed. The patient was satisfactorily discharged on the 8th post-operative day. She is doing well after her follow-ups 4 years later.
Patient no. 1. (A) Admission CT Scan showing a huge left hepatic lobe abscess of unknown origin. (B) Postdrainage control CT Scan showing an atrophic left hepatic lobe with the residual hepatic abscess and a high-density linear lesion inside (arrow). (C) Laparoscopic view of the fish bone (arrow). (D) Corresponding gross specimen of the resected left lateral segment of the liver. The fish bone (arrow) is shown horizontally having migrated into the liver, and the hepatic abscess can be observed. Color version.
We have been able to collect, including our two patients presented here, at least 53 well-described identified cases of fish bone-related intra-hepatic abscesses. In our literature review only 4 papers have been published by Spanish groups.4–7 We found a mortality of 9.4% (5 deceased patients out of the 53 cases studied). The treatment of choice in the literature remains an aggressive approach. It involves the mandatory drainage of the abscess and removal of the fish-bone, and a careful search for the source of perforation. Recently, some reports have shed some light on the role of minimally invasive treatments for this condition. The treatment consists of a non-operative ultrasonographic-guided abscess drainage, the interventional percutaneous or endoscopic removal of the foreign body, and the systemic administration of appropriate antibiotics.8–10 Our cases and the review of the literature illustrate the difficulty in making the preoperative diagnosis, and alert that such etiologic source should be included in the differential diagnoses in patients with liver abscesses of unknown origin. The more familiar with this pathology surgeons, gastroenterologists and hepatologists are, the more patients will be diagnosed and treated properly.
Please cite this article as: Gómez Portilla A, Ezurmendia B, Martín E, López de Heredia E, Muriel López J. Absceso intrahepático por espina de pescado. ¿Una condición pasada por alto infradiagnosticada? Cir Esp. 2019;97:116–118.