The link between Crohn's disease (CD) and gallstone ileus has been described previously in the literature.1–5 In these cases a biliary-enteric fistula is usually observed, and instead of the calculus impacting in the ileocecal valve, it does so in the segment of small intestine that is stenosed due to CD.
Ulcerative colitis (UC) and CD are 2 distinct illnesses, although both are considered chronic inflammatory bowel disease. One of the main differences between them is that CD can affect any part of the gastrointestinal tract. Inflammation of the terminal ileum is the most common location, in comparison to UC, where only the large bowel is affected.6 We present the case of an elderly patient with a prior diagnosis of ulcerative colitis who was urgently operated on for gallstone ileus. The diagnosis was confirmed preoperatively by an abdominal CT scan.
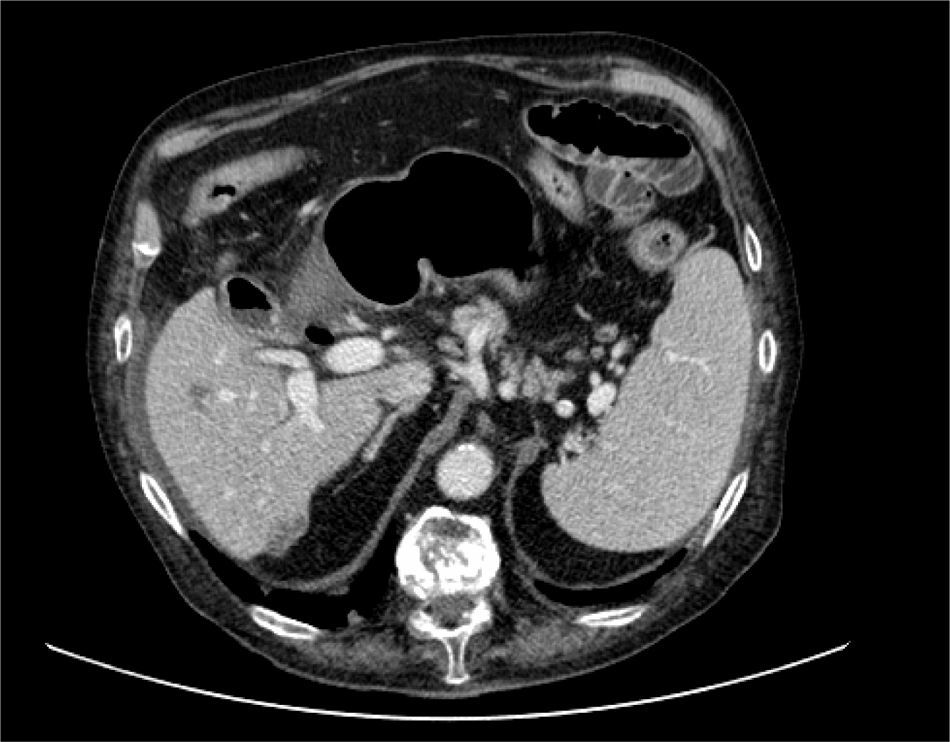
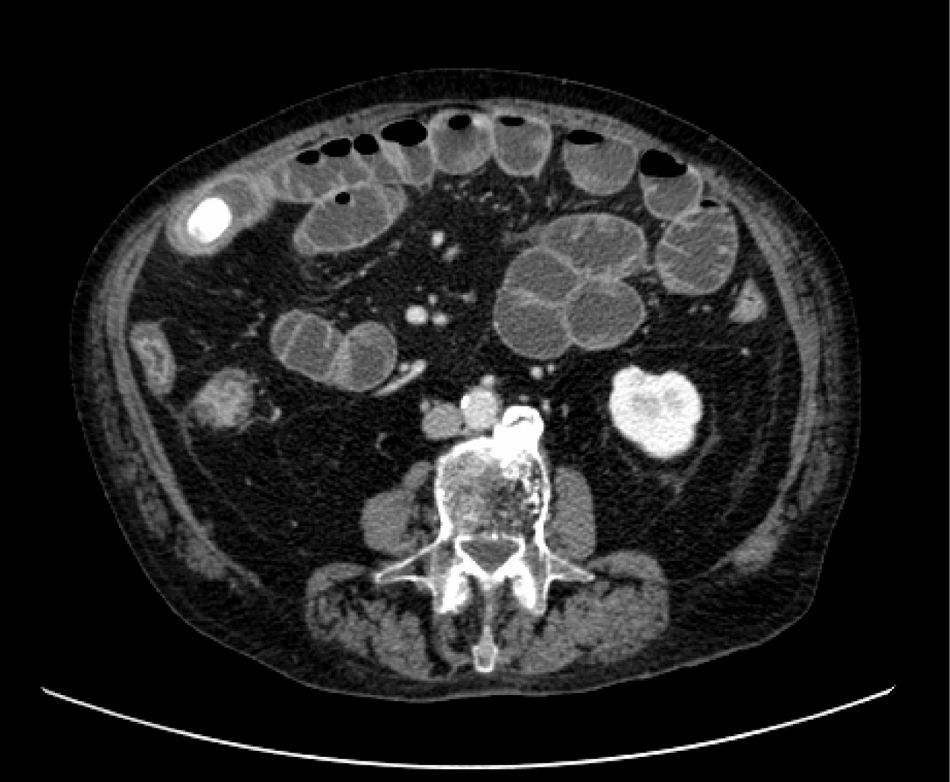
An 84-year-old male with a personal history of type II diabetes mellitus, chronic bronchitis and a 60 year diagnosis of UC treated with aminosalycilates, presented to the Emergency Department complaining of abdominal pain, vomiting, and abdominal distension of 48h duration. In the abdominal CT scan, pneumobilia was observed (Fig. 1), and distension of the small bowel up to the ileum where a calculus had impacted (Fig. 2) in a stenotic segment of terminal ileum with wall thickening that extended to the ileocecal valve. With the diagnosis of a gallstone ileus and terminal ileitis, an emergency laparotomy was performed corroborating the existence of an ileitis with a calculus of 3cm impacted in the thickened bowel and distension of the rest of the small bowel. The segment of the affected distal ileum measured around 40cm and had the typical macroscopic appearance of CD with thickening of the mesentery and its growth toward the antimesenteric margin. No signs of active inflammation were observed in the large intestine. An enterotomy was performed on the healthy proximal bowel and the calculus was extracted. The patient did not refer any symptoms of recent bowel obstruction and therefore, given the long period without any prior resections, it was decided to preserve the affected ileum and no action was performed on the gallbladder.
At present, it is very uncommon for a patient with CD to be wrongly diagnosed with UC, because radiology techniques, histological studies, and endoscopic procedures have advanced considerably. However, 5% of patients present characteristics of both CD and UC and cannot be classified as either type. In these cases the term non-classified inflammatory bowel disease is used.6
At the time of surgery, our patient displayed terminal ileitis with microscopic characteristics typical of CD, in spite of his previous diagnosis of UC. The treatment he followed with oral aminosalycilates could be effective both for CD and UC and did not help to discriminate between the diseases. In the abdominal CT scan, which was performed as an emergency procedure to confirm the diagnosis of small bowel obstruction, the existence of CD with gallstone ileus was considered for the first time.
The manifestation of a gallstone ileus in patients with CD1–5 is exceptional. Cases of small bowel obstruction caused by foreign bodies impacting on stenosed bowel segments in patients with CD have been described.7–9 They usually occur in elderly individuals who have had CD for a long time and in some cases, the diagnosis of CD was carried out after an operation.1 Pneumobilia is fundamental in confirming the existence of a biliary-enteric fistula, which according to some authors is not always necessary for the appearance of gallstone ileus.3,4 Abdominal CT seems to be without doubt the best imaging test for a correct diagnosis,10 as it was in our case.
For this patient, in his eighties, it was decided not to perform a cholecystectomy in order to avoid the risks of a lesion of the common bile duct. A segmental resection of the terminal ileum was deemed unnecessary because there was no prior history compatible with small bowel obstruction.
Please cite this article as: De Tomás Palacios J, et al. Íleo biliar en paciente con enfermedad de Crohn. Cir Esp. 2013;91:56–7.