Cystic lesions of the adrenal gland are a rare pathology, with an overall reported incidence in autopsy series between 0.064% and 0.18%. Currently, the incidence is increasing due to improvements and the greater use of imaging tests.1 The lesions are mostly small (<4cm) and asymptomatic, while giant lesions (>10cm) are very rare.2,3
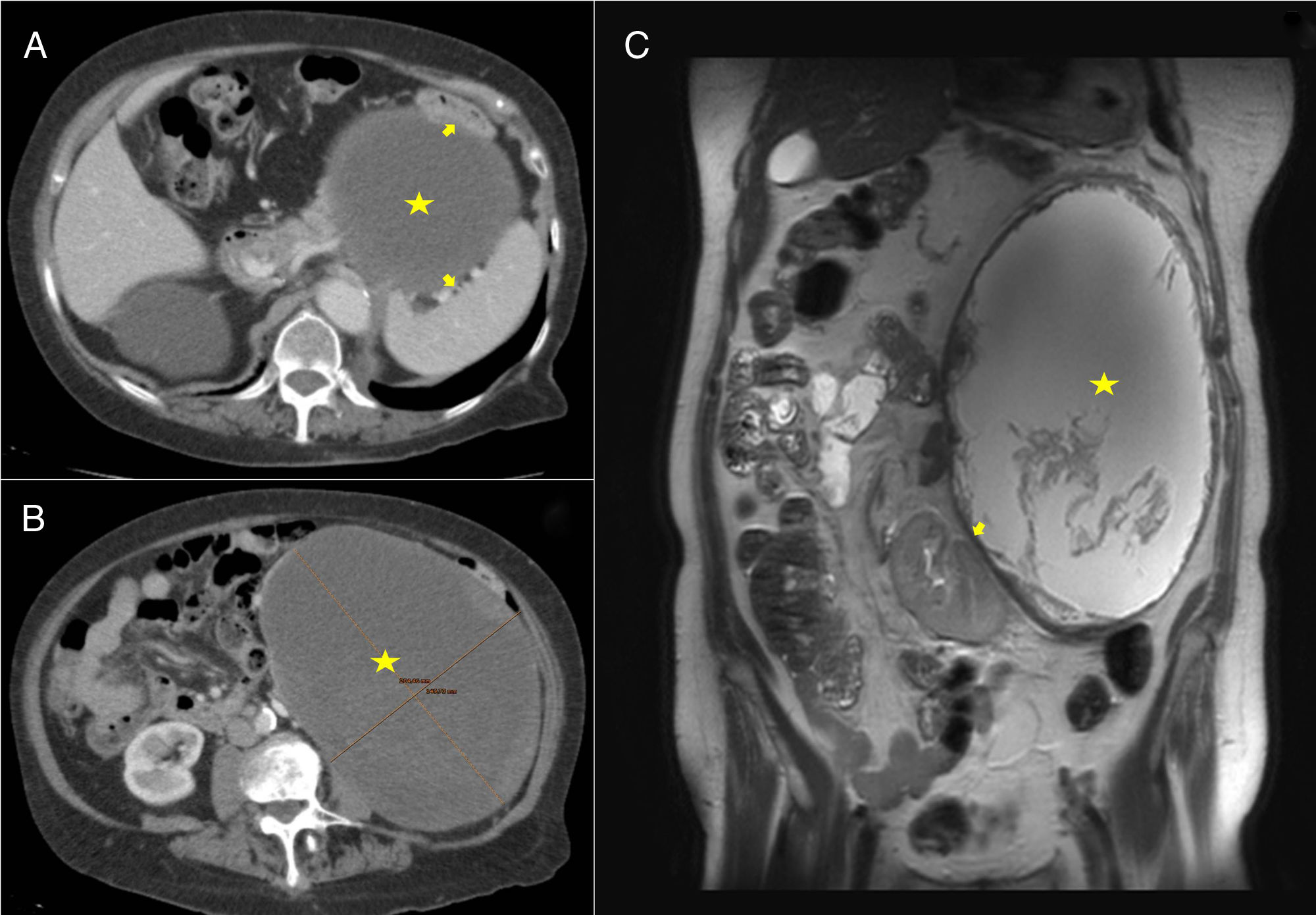
Our patient is an 84-year-old woman with a history of lumbar pain radiating toward the flank and hypogastrium associated with a palpable abdominal mass that had been increasing in size for the previous 8 years. On physical examination, the abdomen was soft and a mass was observed in the left hemiabdomen extending from the subcostal region to the left iliac fossa; the mass had smooth edges, and palpation was not painful. Blood count, biochemistry and hormone function tests showed no noticeable alterations. A computed tomography (CT) scan revealed a large mass in the left hemiabdomen (caudal and medial to the splenic angle of the colon) that was predominantly cystic and measured 20×14.5×19.5cm (Fig. 1A and B). Magnetic resonance imaging (MRI) detected a large retroperitoneal mass that occupied the entire left flank, showing liquid content (Fig. 1C), whose origin could not be specified. Given the large size of the tumor, the patient's symptoms and the need for classification, we decided to operate.
(A and B) CT: cystic mass (marked with a star) compressing and displacing the spleen, colon and left kidney (arrows). (C) MRI-T2: mass with liquid content and heterogeneous internal material (marked with a star); the walls present an irregular morphology and increased thickness, displacing the left kidney downwards and internally (arrow).
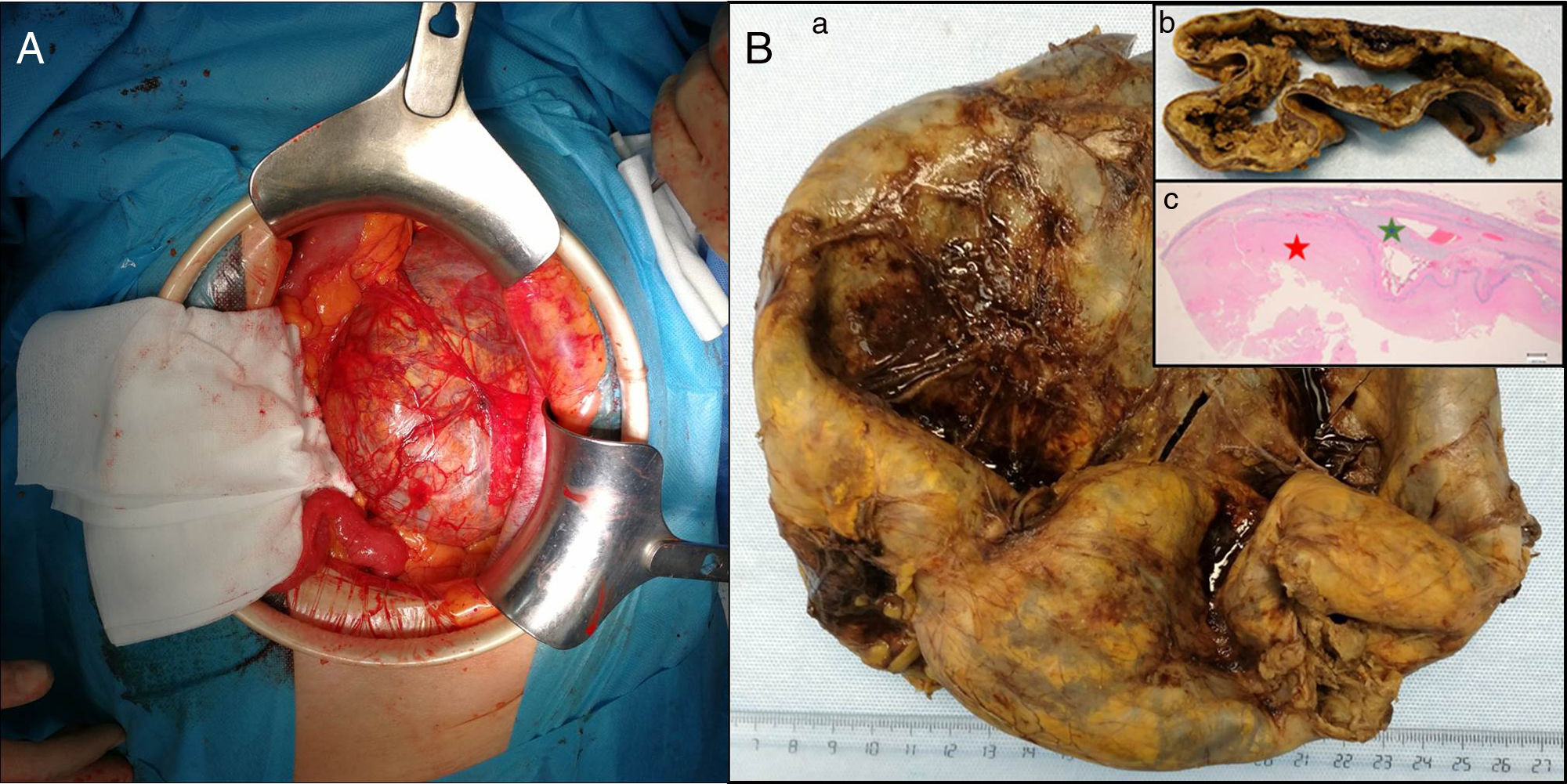
Using a mid-line laparotomy, a giant intra-abdominal cystic tumor was observed that measured approximately 20×15×15cm (Fig. 2A). Complete resection was performed without complications. The patient presented satisfactory postoperative progress and was discharged on the fifth postoperative day. During follow-up in the outpatient consultation, the patient was asymptomatic, and there have been no signs of recurrence after 12 months of follow-up. The pathology report identified the mass as a giant adrenal adenoma with cystic degeneration secondary to hemorrhage with fibrinoid necrosis (Fig. 2B).
(A) Intraoperative: large retroperitoneal cystic mass displacing the colon and spleen laterally and the left kidney downwards prior to resection; (B) Anatomic pathology: (a) surgical piece measuring 18.5×15.5×4cm, yellowish in color, (b) corresponding with a cystic cavity with a friable, rough wall that is brownish in color, ranging between 4 and 10mm in thickness. (c) Histologically, the mass corresponded with an adrenal adenoma with cystic degeneration secondary to hemorrhage, with fibrinoid necrosis (red star) (green star shows the remains of the adrenal cortex). The colors of the figure can only be seen in the electronic version of the article.
The first case of an adrenal cyst was described by Greiselius in 1670, and the second was reported almost two centuries later in 1837.4 These lesions represent a rare entity with heterogeneous symptoms and etiology.5 They are generally benign, but may be associated with adrenal neoplasms.6 Their presentation is usually unilateral, rarely bilateral (8%–15%), and more frequent between the third and fifth decades of life. There is a certain predominance in females, with sizes varying from a few mm to 50cm or more.5
Adrenal cysts are classified into four histological subtypes: pseudo-, epithelial, endothelial and parasitic. Pseudocysts are the most frequent subtype and are mostly due to the organization of a previous traumatic hematoma, a toxic or infectious process or, less frequently, secondary to degeneration or hemorrhage of an adrenal tumor.6 Adrenal tumors such as adenomas can generate cystic changes secondary to degeneration or hemorrhage, resulting in a cystic lesion that can be included in the pseudocyst group,7 as in the case presented.
Small-sized cystic lesions of the adrenal gland are often asymptomatic, while giant lesions (>10cm) present with abdominal and/or lumbar pain (as in the case presented), gastrointestinal symptoms secondary to extrinsic compression, dyspnea or palpable mass.2
Giant cysts are difficult to diagnose preoperatively, given the difficulty to determine their origin.8 Once suspected or identified, the strategy is based on assessing the functional status and malignant potential.9 Imaging studies are used to assess the size, morphological characteristics (texture, density, wall thickness, calcifications) and relationships with neighboring structures; however, these findings are usually inadequate for the definitive subtyping of an adrenal cyst or to distinguish between benign and malignant entities. With these tests, the differential diagnosis should include splenic, pancreatic, hepatic, renal, mesenteric and retroperitoneal cysts as well as abdominal aneurysms.4 CT is the imaging test of choice for the initial evaluation of an adrenal mass, with a sensitivity of 85%–95%. MRI has a specificity similar to CT to differentiate between benign and malignant lesions; however, it seems superior for determining lesion dimensions, discriminating the lesion from adipose tissue and detecting pheochromocytomas.10
The treatment of choice is complete surgical resection, which has an excellent prognosis with no evidence of recurrence.3 The lateral transabdominal approach continues to be the most frequently used method, offering the advantages of optimal control of the vessels and visceral structures as well as easy identification of anatomical landmarks. Midline laparotomy is performed in complicated cases, in very large tumors or when there is evidence of compression or invasion of the surrounding structures, which is why we use this approach.5 Percutaneous aspiration is an alternative treatment option when the cyst is not hormonally active, there is no suspicion of malignancy and in patients with high surgical risk.8
We conclude that giant adrenal cystic lesions are a very rare pathology, with a heterogeneous etiology and clinical behavior. Imaging and adrenal function studies are very important. When there is an uncertain diagnosis, large lesions or suspicion of malignancy (as in the case presented), complete surgical resection of the lesion and a thorough pathological study are required,
Please cite this article as: Trujillo Díaz JJ, Ferreras García C, Romero de Diego A, González-Obeso E, Beltrán de Heredia y Rentería JP. Adenoma suprarrenal gigante con degeneración quística hemorrágica. Cir Esp. 2019;97:539–541.