Liposuction is a surgical procedure that has been widely performed in recent decades, involving the extraction of subcutaneous cellular tissue for essentially aesthetic purposes. The incidence of local and systemic complications is low, although these can sometimes lead to the death of the patient (1/5000 procedures).1 An example is peritonitis secondary to iatrogenic bowel perforation caused by the liposuction cannula during the intervention. While this complication is very rare, the associated mortality rate is high (50%).2
We present the case of a 32-year-old male who reported abdominal pain, incoercible vomiting, fever, respiratory failure and hemodynamic instability 3 days after undergoing abdominal liposuction. Examination revealed a distended, painful abdomen with bloody discharge through the cannula incisions. The initial laboratory study detected leukocytosis, renal failure, elevated muscle enzymes (CK 19.393U/L), procalcitonin 2.31ng/mL and metabolic acidosis. A thoracoabdominal CT scan showed evidence of subcutaneous emphysema of the thoracic and abdominal wall, pneumomediastinum, pneumoperitoneum and free fluid in the pelvis (Fig. 1). Given these findings, empirical antibiotic therapy was initiated with piperacillin-tazobactam, fluid therapy and vasoactive support, and the patient was prepared for urgent surgery. During surgery, a double ileal perforation was confirmed with abundant peritoneal fluid, in which Pseudomonas aeruginosa was subsequently isolated. In the postoperative period in the Intensive Care Unit, the patient developed abdominal compartment syndrome, requiring reoperation with decompressive laparotomy. Despite treatment, the patient developed multiple organ failure (hemodynamic, respiratory, renal and hematological) that was resistant to treatment, resulting in death on the third day after admission. Autopsy confirmed the diagnosis of peritonitis secondary to intestinal perforation during liposuction.
From its beginning in the 1970s to the present, there have been many advances made in the surgical technique of liposuction, especially with the use of smaller-diameter cannulae, ultrasound, assisted mechanical aspiration, etc.3 Currently, the technique used is liposuction under local tumescent anesthesia, which involves injecting a mix of local anesthetic (lidocaine), a vasoconstrictor (epinephrine) and saline solution before the fat is suctioned through the cannula.4
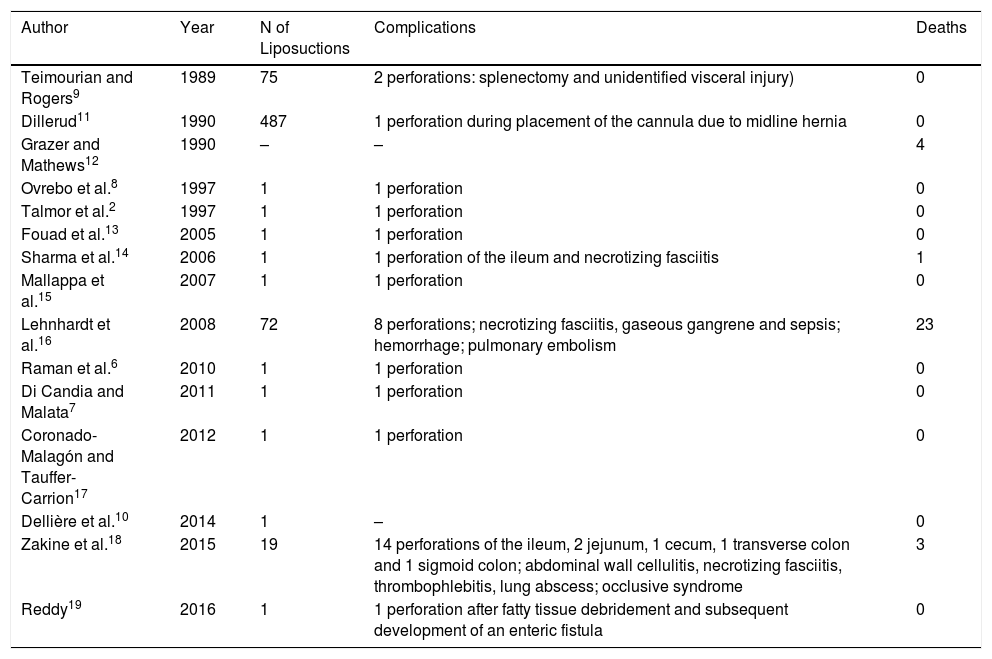
The percentage of complications reported in the literature ranges from 1% to 9%.5 These differences may be due to a publication bias regarding the complications that occur in interventions for aesthetic purposes (Table 1). In addition, the defining criteria have not been uniformly described, and therefore the comparison between studies is difficult. Minor complications are primarily related to the local anesthetic (seroma, edema, infections, hypoesthesia, pain, depigmentation and hematoma). Major complications6 include pulmonary embolism (23% of deaths), abdominal or thoracic perforation (15% mortality),7 problems related to anesthesia (bradycardia or hypotension due to lidocaine), infectious processes such as necrotizing fasciitis, hemorrhagic complications (4.6% mortality)8 or fat embolism.
Summary of Cases of Intestinal Perforation After Liposuction Published in the Literature.
| Author | Year | N of Liposuctions | Complications | Deaths |
|---|---|---|---|---|
| Teimourian and Rogers9 | 1989 | 75 | 2 perforations: splenectomy and unidentified visceral injury) | 0 |
| Dillerud11 | 1990 | 487 | 1 perforation during placement of the cannula due to midline hernia | 0 |
| Grazer and Mathews12 | 1990 | – | – | 4 |
| Ovrebo et al.8 | 1997 | 1 | 1 perforation | 0 |
| Talmor et al.2 | 1997 | 1 | 1 perforation | 0 |
| Fouad et al.13 | 2005 | 1 | 1 perforation | 0 |
| Sharma et al.14 | 2006 | 1 | 1 perforation of the ileum and necrotizing fasciitis | 1 |
| Mallappa et al.15 | 2007 | 1 | 1 perforation | 0 |
| Lehnhardt et al.16 | 2008 | 72 | 8 perforations; necrotizing fasciitis, gaseous gangrene and sepsis; hemorrhage; pulmonary embolism | 23 |
| Raman et al.6 | 2010 | 1 | 1 perforation | 0 |
| Di Candia and Malata7 | 2011 | 1 | 1 perforation | 0 |
| Coronado-Malagón and Tauffer-Carrion17 | 2012 | 1 | 1 perforation | 0 |
| Dellière et al.10 | 2014 | 1 | – | 0 |
| Zakine et al.18 | 2015 | 19 | 14 perforations of the ileum, 2 jejunum, 1 cecum, 1 transverse colon and 1 sigmoid colon; abdominal wall cellulitis, necrotizing fasciitis, thrombophlebitis, lung abscess; occlusive syndrome | 3 |
| Reddy19 | 2016 | 1 | 1 perforation after fatty tissue debridement and subsequent development of an enteric fistula | 0 |
Intestinal perforation after liposuction was first reported in the literature in 1989.9 Thereafter, the information available for this complication is based on the publication of isolated cases or small series by surgeons, which primarily describe intestinal perforations and serious infections after the placement of the cannulae.
It is well known that there is a group of patients at high risk for intestinal perforation after liposuction. Patients with abdominal wall hernias (including umbilical10), previous abdominal surgery, immunosuppression and obesity with a predominance of body fat distributed at the hypogastrium all have a higher risk. Any changes in the abdominal wall make it difficult to identify the correct plane to perform liposuction. Scars in the lower abdomen, with the resulting wall fibrosis and subcutaneous cellular tissue, represent high-friction areas that make handling of the suction cannulae difficult. Performing an ultrasound or abdominal CT scan prior to surgery provides important additional information about the abdominal wall characteristics.8 Applying undue or poorly-directed force with the surgical instruments or the use of vibrating cannulae during the procedure may increase the risk of accidental perforations of the fascia and peritoneum, reaching the intestine.8 Also, poor positioning of the patient without adequate hyperextension of the abdomen can favor this complication.
It seems appropriate, therefore, to propose the following measures for the prevention of intestinal injuries and their complications related to liposuction surgery:
In the preoperative period: abdominal examination to assess scars, hernias or diastasis with risk of perforation. In uncertain cases, an ultrasound or CT scan should be performed.
During the intervention: perform a technique that would specifically avoiding the aponeurotic plane of the abdominal wall, while considering the direction of the cannula, force used and position of the patient.
In the postoperative period: systemic evaluation of symptoms and signs of complications during the first 24h after the intervention (could be done 3h after the intervention, and again after 16–24h). In case of alarming symptoms, such as severe pain, nausea, bloating or subcutaneous crepitation, perform abdominal examination and complementary tests urgently.
In conclusion, liposuction is a priori a safe and effective surgical procedure. Nevertheless, under certain circumstances that are difficult to predict, it can cause serious complications that put the patient's life at risk, such as intestinal perforation. It is important for surgeons to select patients appropriately and strictly monitor them in the immediate postoperative period in order to detect and treat any potential complications as soon as possible.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Marques Álvarez L, Rodríguez-García R, Palomo Antequera C, Escudero Augusto D, González-Pinto I. Perforación intestinal tras liposucción. Cir Esp. 2019;97:536–538.