Liposarcomas are rare tumors and their location in the esophagus is very uncommon. We present the case of a 26-year-old patient being studied for anemia and weight loss of 10kg in recent months, with no other associated symptoms, who was diagnosed with a well-differentiated giant esophageal liposarcoma with an undifferentiated component.
During esophagogastroscopy, a submucosal lesion was observed that extended from 18 to 39cm from the dental arch and occupied the entire esophageal lumen.
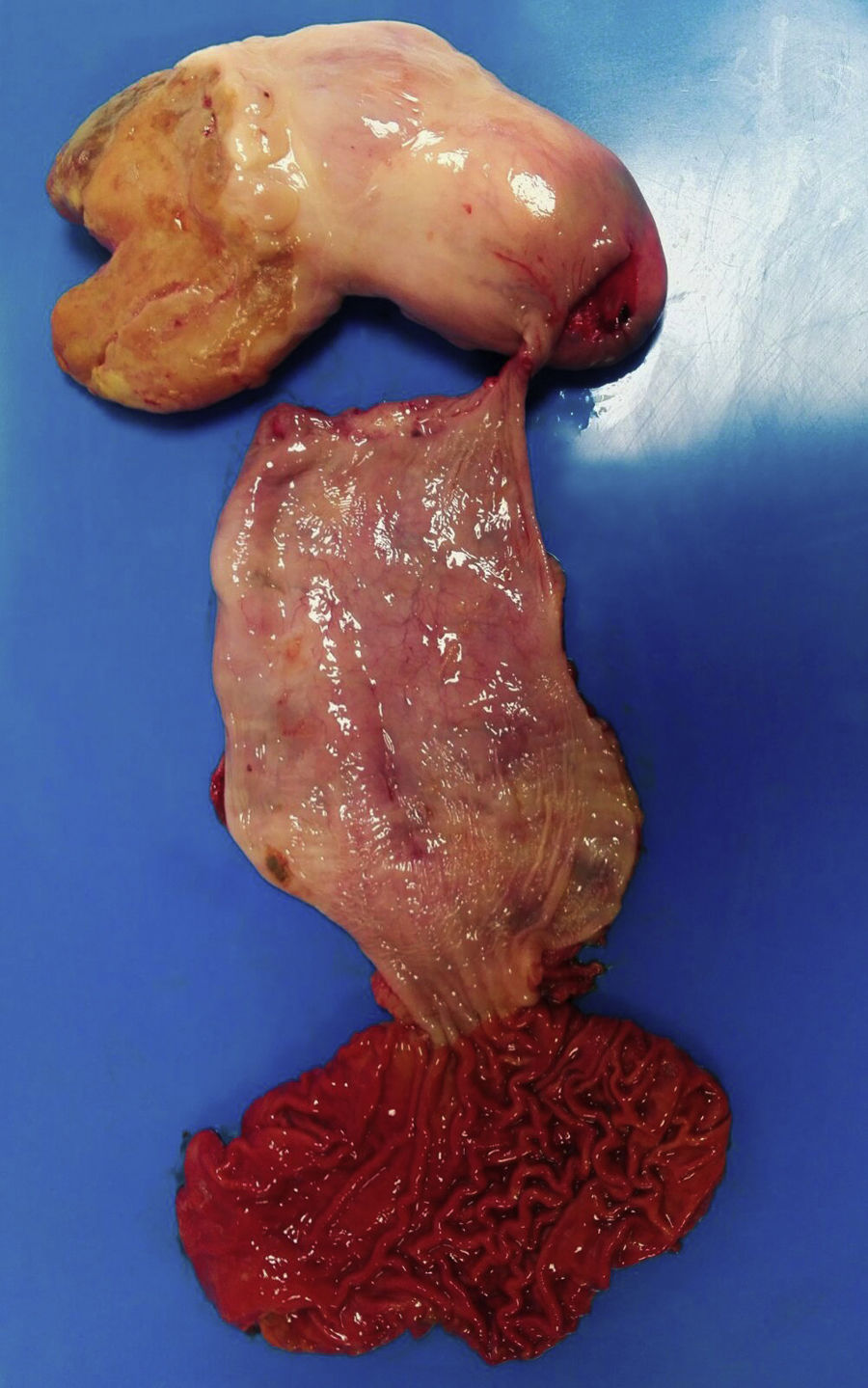
Thoracoabdominal CT scan confirmed the presence of a voluminous esophageal mass measuring 21cm in length, with a well-defined outline, apparently submucosal with fat density (Fig. 1). It was accompanied by esophageal dilatation and tracheal compression. No lymphadenopathies or signs of distant extension were detected.
The study was completed with an endoscopic ultrasound, which showed a mass that depended on the submucosa of the esophageal wall and ruled out infiltration of the displaced structures. FNA biopsy of the lesion reported a malignant mesenchymal lesion, undifferentiated, with Ki-67 >30%.
Surgery was indicated, and an esophagectomy was conducted with three accesses: thoracoscopy, laparoscopy and cervicotomy. Given the extension of the tumor in the cervical region, the cervical esophagus was divided about 2cm from the mouth of the esophagus. The piece was extracted abdominally due to its large volume. Esophageal reconstruction involved a posterior mediastinal tubular gastric pull-up and manual cervical anastomosis.
At the opening of the specimen, a large intraluminal tumor was found occupying the entire thoracic esophagus and the distal portion of the cervical esophagus, pedunculated with an implantation base in the cervical esophagus (Fig. 2).
The pathological anatomy study reported a submucosal pedunculated lesion measuring 16×9×7cm. It was a well-differentiated liposarcoma with a dedifferentiated component, tumor-free pedicle, and no lymph node metastases. The immunohistochemistry study revealed immunoreactivity for P16 and S100 proteins in the well-differentiated areas and for desmin and CD34 in the dedifferentiated areas. The molecular analysis of the MDM2 gene revealed amplification in 85% of the cells.
The incidence of liposarcoma is 0.5% of all esophageal tumors.1 The average age of onset is 58 years and they are more frequent in males (72%).
In most cases they grow on large pedunculated polyps and less frequently in the esophageal wall thickness. The average size is 13cm long and 3.5cm wide.1 In most cases, the base of implantation is located in the cervical esophagus.2–4
They can be asymptomatic for years until they reach a large size. The most common symptoms are dysphagia and weight loss, although they can also present with odynophagia, cough, nausea, retrosternal pain and even asphyxia.3,5
For the diagnosis, esophagogastroscopy is useful, which frequently reveals a lesion covered with normal-looking mucosa. In our case, the large volume of the lesion with growth toward both the cervical esophagus and the distal esophagus prevented us from locating an implantation base and initially oriented us toward a transmural lesion. CT or MRI will provide anatomical data of the lesion and its composition. The barium esophagogram often shows a dilated and atonic esophagus that can sometimes become confused with an achalasia. Echoendoscopy may be useful for the diagnosis of a polypoid lesion because it helps detect the fibrovascular axis, with an echogenic aspect of the adipose tissue and anechoic areas due to its vascularization. In addition, direct biopsy can lead us to a histological diagnosis.3,6,7 The location of the implantation pedicle will help us in choosing an appropriate treatment.
Histologically, they grow from the mucous or submucosal layer of the esophagus,8 and are classified into 4 subtypes: well differentiated, this being the most common (68%), myxoid (20%), undifferentiated (6%) and pleomorphic (6%). In our patient, the anatomopathological diagnosis established a heterogeneous pattern with a well differentiated and undifferentiated component.
We must make differential diagnosis with other mesenchymal tumors such as leiomyosarcoma or GIST,9 both have submucosal growth and can reach large sizes. The definitive diagnosis is anatomopathological, including specific immunohistochemical techniques.
The treatment of choice is the complete resection of the tumor, which can be done through different techniques.6,10 Endoscopic excision is an option in polypoid lesions with stems less than 2cm clearly identifiable and poorly vascularized.10 Resection through an esophagotomy is the technique of choice in polyps larger than 5cm with large vascularized pedicles. The most common approach is cervicotomy, although it can also be done through thoracotomy,1 depending on the location of the stem of the lesion. Esophagectomy is an option in lesions with several bases of implantation or suspicion of transmural tumors.10
The prognosis is uncertain, due to the small number of cases published with long follow-up.4 Factors that will influence the prognosis are the histological subtype, the location and the radicability of the surgical resection.
Please cite this article as: Rodríguez Pérez A, Pérez Serrano N, García Tejero A, Escudero Nalda B, Gil Albarellos R. Liposarcoma gigante de esófago en paciente joven, asintomático. Cir Esp. 2018;96:381–383.