Echinococcosis is a parasitic disease that can develop as hydatidosis due to Echinococcus granulosa (EG) (cystic echinococcosis), cystic alveolar disease due to E. multilocularis, or polycystic echinococcosis.1 Human echinococcosis continues to be endemic, and Spain is one of the countries affected, although there are no official data since 1996. Most cases are detected incidentally; when symptoms appear, these depend on the size and location of the lesions.
In patients with human immunodeficiency virus (HIV) infection, opportunistic infections are common. However, HIV–EG coinfection is rare and can be associated with disseminated echinococcosis.2
Our objective is to present 2 patients with HIV infection and cystic echinococcosis, while reviewing the literature on this rare co-infection.
A 47-year-old woman with stage A3 HIV infection came to the emergency room due to fever over the previous 2 weeks and pain in the right hypochondrium. On examination, she presented 3-finger hepatomegaly, and the lab analysis demonstrated: 12800leukocytes/L; alkaline phosphatase 251IU/L; GGT 178IU/L; PCR 156mg/L.
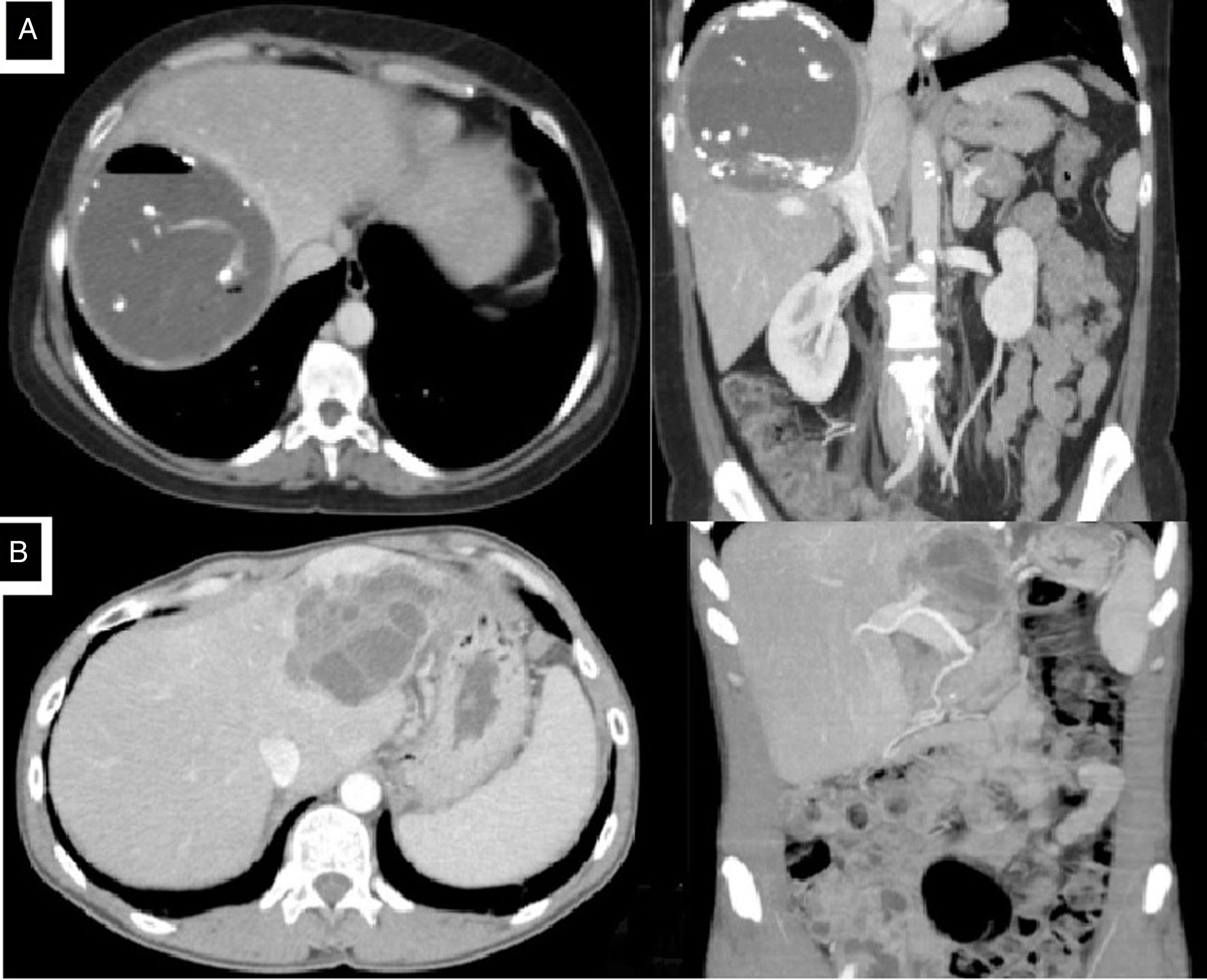
Computed tomography showed a hepatic hydatid cyst measuring 11.5cm in segments VII–VIII, with biliary communication and compression of the inferior vena cava (IVC) (Fig. 1A). The serology was positive for Echinococcus (1/1280). Treatment was started with oral albendazole 400mg/12h and piperacillin-tazobactam 4g/0.5g/8h/iv. Percutaneous drainage was performed, and Streptococcus oralis was isolated in the sample.
(A) Case 1: abdominal CT scan showing a hydatid cyst measuring 11.5cm in segment VII–VIII that communicates with the bile duct; (B) Case 2: abdominal CT scan showing a hydatid cyst measuring 6.4cm in the left liver lobe compressing the left intrahepatic bile duct; B: surgical field.
ERCP revealed cystobiliary communication, cystic material in the bile duct and papillary stenosis, and balloon dilation was performed. Elective surgery was scheduled, during which a hydatid cyst was observed, adhered to the diaphragm and causing partial compression of the IVC. Subtotal cystectomy was performed, leaving a patch over the IVC.
The postoperative period was uneventful, and the patient was discharged on the 4th postoperative day (POD) (Clavien 0), with albendazole treatment for one month.
A 41-year-old man, with a history of partial cystectomy due to hepatic hydatidosis, stage B3 HIV infection and HCV infection with F2 fibrosis, came to the emergency room for fever, jaundice and abdominal pain that had persisted for 4 days. Lab work revealed: 13200leukocytes/L; GGT 472U/L; alkaline phosphatase 144U/L; total bilirubin 5.3mg/dL.
Computed tomography revealed recurrence of a 6.4-cm hydatid cyst that almost completely occupied the left liver lobe, with compression of the left bile duct, splenomegaly and signs of portal hypertension (Fig. 1B).
Treatment was started with oral albendazole 400mg/12h and piperacillin/tazobactam 4g/0.5g/8h/iv. During elective surgery, a hydatid cyst was observed with left intrahepatic biliary communication and signs of chronic liver disease; and left hepatectomy was carried out with biliary reconstruction over plastic prosthesis. In the postoperative period, the patient presented ascites, which was managed with spironolactone, and a biliary fistula that was resolved by repositioning the prosthesis and percutaneous drainage (Clavien IIIA). The patient received treatment with oral albendazole for one month.
Hydatidosis is a health problem in endemic areas such as Spain. Its most frequent locations are the liver (70%–80%) and lungs, and less frequently the spleen and kidneys.1,3
In HIV-positive patients, protozoan infections are the most frequent parasitosis,1,4 while those caused by helminths are rare. Among these, cestodes are exceptionally rare.1 The differential diagnosis should include typical infections in HIV5 and may be difficult in immunosuppressed patients, so it should be considered in patients from endemic areas.6
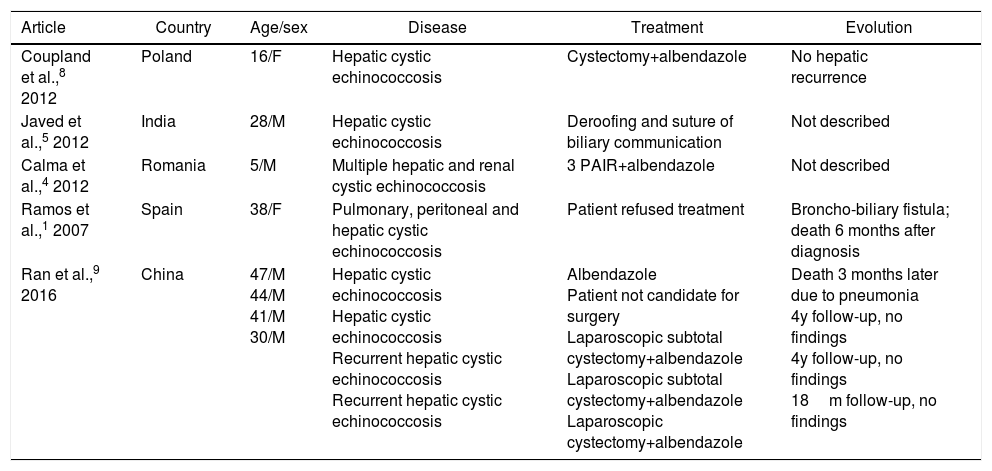
The literature on hydatidosis and HIV is scarce.7 In a review of PubMed articles from 1996 to date with the keywords ‘hydatid disease’ and ‘HIV’ (43 results), 14 cases of hydatidosis and HIV infection were found; however, only 8 had liver involvement1,4,5,8,9 (Table 1). The rest included 2 cases of alveolar echinococcosis, 2 with pulmonary hydatidosis, spinal cyst in one patient and hydatid cyst of the abdominal wall in another.1,5,8,9 In this article, we present 2 cases of HIV-hepatic hydatidosis coinfection, both with cystobiliary communication, a situation that is observed in approximately one-third of hydatid cysts.
Articles With Coexistence of Hepatic Hydatidosis and HIV Infection.
| Article | Country | Age/sex | Disease | Treatment | Evolution |
|---|---|---|---|---|---|
| Coupland et al.,8 2012 | Poland | 16/F | Hepatic cystic echinococcosis | Cystectomy+albendazole | No hepatic recurrence |
| Javed et al.,5 2012 | India | 28/M | Hepatic cystic echinococcosis | Deroofing and suture of biliary communication | Not described |
| Calma et al.,4 2012 | Romania | 5/M | Multiple hepatic and renal cystic echinococcosis | 3 PAIR+albendazole | Not described |
| Ramos et al.,1 2007 | Spain | 38/F | Pulmonary, peritoneal and hepatic cystic echinococcosis | Patient refused treatment | Broncho-biliary fistula; death 6 months after diagnosis |
| Ran et al.,9 2016 | China | 47/M 44/M 41/M 30/M | Hepatic cystic echinococcosis Hepatic cystic echinococcosis Recurrent hepatic cystic echinococcosis Recurrent hepatic cystic echinococcosis | Albendazole Patient not candidate for surgery Laparoscopic subtotal cystectomy+albendazole Laparoscopic subtotal cystectomy+albendazole Laparoscopic cystectomy+albendazole | Death 3 months later due to pneumonia 4y follow-up, no findings 4y follow-up, no findings 18m follow-up, no findings |
M: male; F: female; PAIR: puncture, aspiration, injection, re-aspiration.
According to recent literature, HIV-EG coinfection, due to immunosuppression, may predispose patients to develop disseminated forms and rapid progression of parasitic disease more frequently than in patients not infected by HIV.2,5,10 Javed et al. suggest that the larger size of the cysts and the higher frequency of complications, such as infection or biliary communication, may be related to immunosuppression in HIV patients, but there are no conclusive data confirming it as a risk factor for the development of hydatidosis.5 In addition, patients with hydatidosis are usually asymptomatic, and infection can occur 5–15 years before the symptoms appear, making it difficult to determine how long HIV infection and hydatidosis coexisted in the patient.4
In conclusion, cestode infections are rare in HIV patients, but they can occur and be associated with a greater severity of hydatidosis. More studies are needed, especially in countries where hydatidosis continues to be endemic, in order to determine the association between the two diseases and their effect on clinical course, epidemiology and host immune response.
Please cite this article as: Manuel-Vazquez A, Latorre-Fragua R, Espinosa A, del Cerro J, Ramia JM. Hidatidosis hepática en pacientes positivos para el virus de la inmunodeficiencia humana. Cir Esp. 2019;97:239–241.