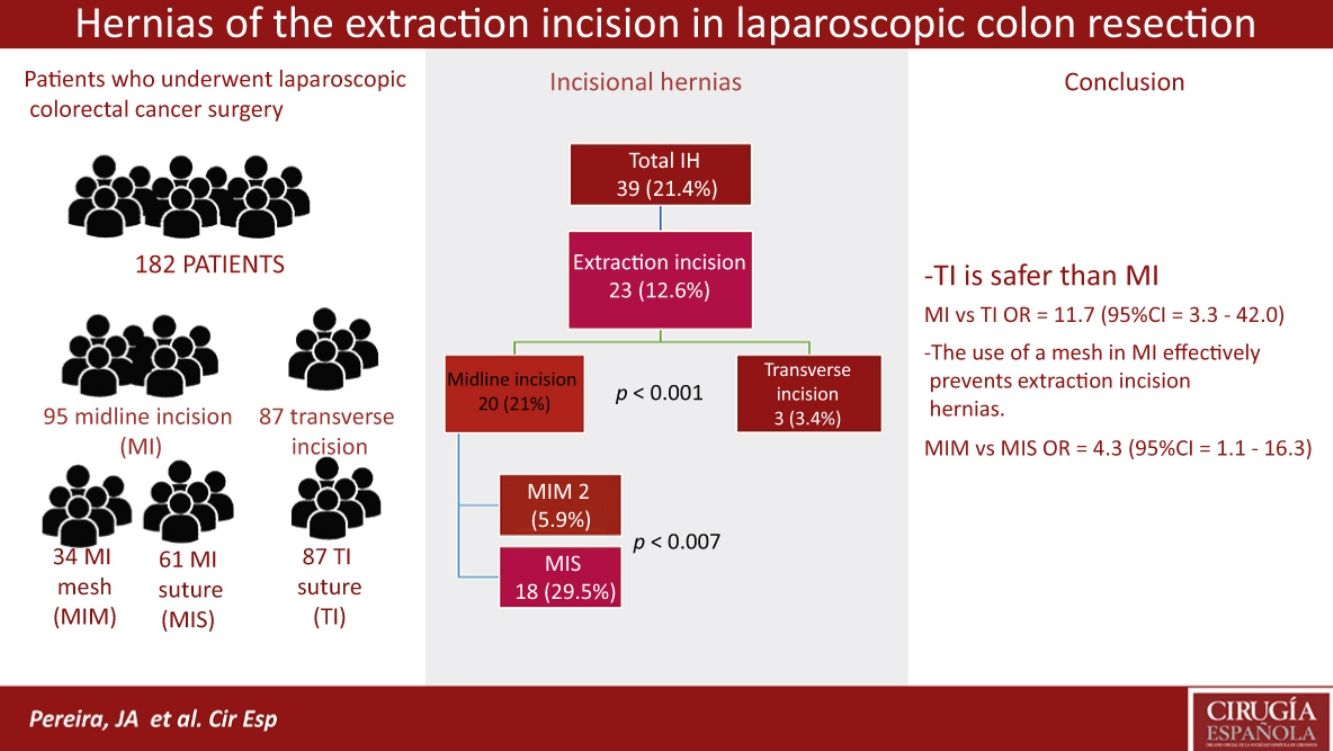
To determine the incidence of incisional hernia (IH) in the extraction incision (EI) in colorectal resection for cancer. To analyze whether the location of the incision has any relationship with the incidence of hernias and whether mesh could be useful for prevention in high-risk patients.
MethodsRetrospective review of the colon and rectal surgery database from January 2015 to December 2016. Data were classified into 2 groups, transverse (TI) and midline incision (MI), and the latter was divided into 2 subgroups (mesh [MIM] and suture [MIS]). Patients were classified using the HERNIAscore. Hernias were diagnosed by clinical and/or CT examination.
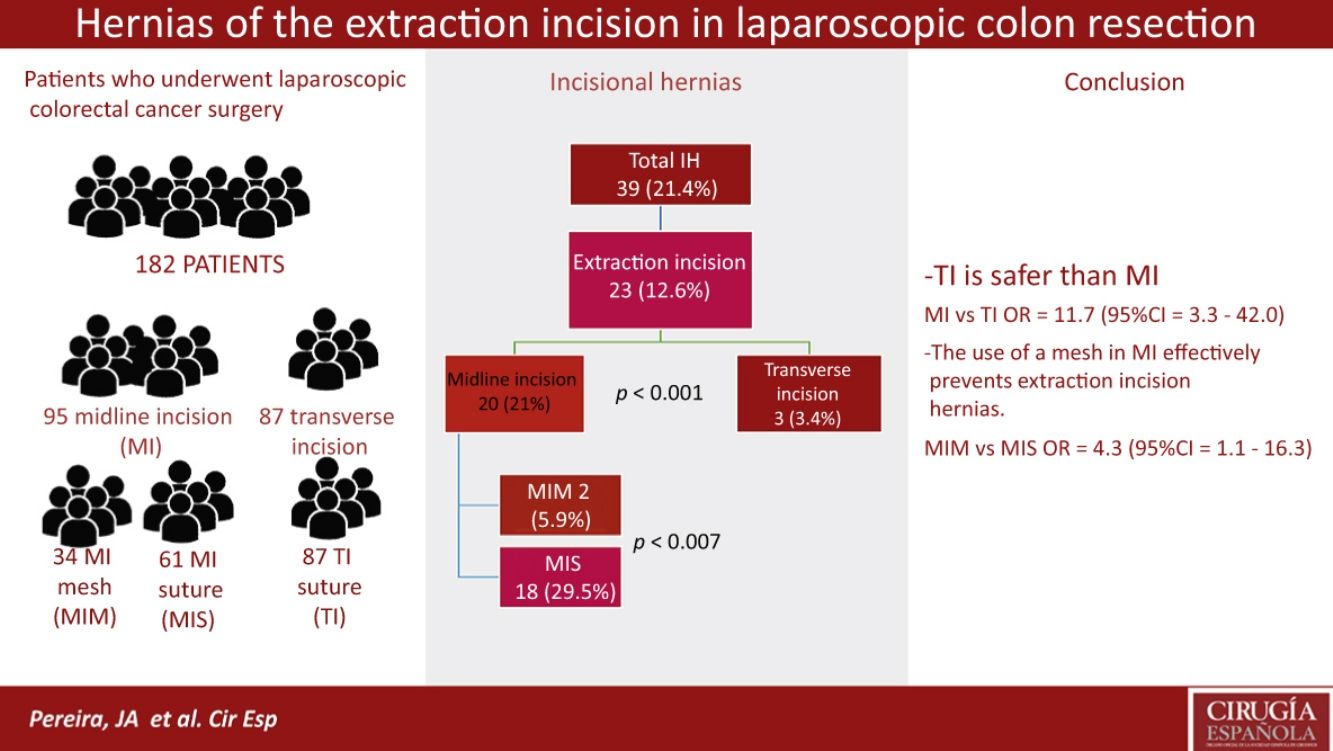
ResultsA total of 182 out of 210 surgical patients were included. After a median follow-up of 13.0 months, 39 IH (21.9%) were detected, 23 of which (13.4%) were in the EI; their frequency was lower in the TI group (3.4%) and in the MIM group (5.9%) than in the MIS group (29.5%; P=.007). The probability of developing IH in the MIS group showed an OR=11.7 (95% CI: 3.3–42.0) compared to the TI group and 4.3 (IC 95%: 1.1–16.3) vs the MIM group.
ConclusionsThe location of the incision is relevant to avoid incisional hernias. Transverse incisions should be used as the first option. When a midline incision is needed, a prophylactic mesh could be considered in high risk patients because it is safe and associated with low morbidity.
Determinar la incidencia de hernia incisional (HI) en la incisión de asistencia (IA) de la pieza en cirugía por neoplasia de colon y recto. Análisis de la relación de la localización de la incisión y uso de una malla en la prevención de la HI en pacientes de alto riesgo.
MétodosRevisión retrospectiva de la base de datos de cirugía de colon entre enero de 2015 y diciembre de 2016. Se establecieron 2 grupos: incisión transversa (IT) e incisión media (IM), a su vez este con 2 subgrupos (malla [IMM] y sutura [IMS]). Se categorizaron los pacientes mediante el sistema HERNIAscore. Las hernias se diagnosticaron clínicamente y por TAC.
ResultadosSe intervino a 210 pacientes, de los que fueron incluidos 182. Tras un seguimiento de 13,0 meses, se detectaron un total de 39 HI (21,9%), de las que 23 (13,4%) fueron en las IA. Estas fueron mucho menos frecuentes en el grupo de IT (3,4%) y en el de IMM (5,9%) que en el de IMS (29,5%; p=0,007). La probabilidad de aparición en el grupo IMS de una HI presentó una OR=11,7 (IC 95%: 3,3-42,0) frente a las IT y de 4,3 (IC 95%: 1,1-16,3) frente al grupo IMM.
ConclusionesLa localización de la incisión es relevante para disminuir las HI. La IT debería ser utilizada preferentemente. En los casos en que se utilice una IM, el uso de una malla profiláctica en pacientes de alto riesgo puede considerarse, ya que es seguro y con baja morbilidad.
Laparoscopic surgery has been associated with a lower incidence of incisional hernias (IH). This has been reported in cholecystectomies,1,2 antireflux surgery1,3 and gynecological surgery,4 in which hand-assist extraction incisions (EI) are not usually used. However, the exact frequency of IH during laparoscopic surgery in colon resection offers controversial data, which are attributable to differences in the procedure, patient risk factors and the type of incision analyzed.5–9 In the specific case of EI, incidences close to 20% have been reported in midline incisions (MI),10,11 while the rates in transverse incisions (TI) are much lower (2%–8%).12–15
In the case of colon cancer, patients who undergo surgery for this pathology frequently present risk factors for the onset of IH, and even colon surgery itself behaves as another risk factor.7,16,17 Likewise, some studies18 have shown that EI, combined with the patient's and surgery-related risk factors, are associated with increased IH incidence, and scoring systems have even been developed to determine the level of individual risk, as in the case of the HERNIAscore.18,19
In the case of resection by laparotomy, there are data in the literature indicating that these patients can benefit from the prophylactic use of mesh implants.20–22 Given that patients operated laparoscopically share the same risk factors, it could be assumed that, in selected cases, prophylactic measures could also prevent EI complications and related reoperations.
The primary objective of our study was to determine the incidence of IH in the EI (extraction of the piece and creation of anastomosis) in different locations, comparing them in a cohort of patients who underwent laparoscopic colon cancer surgery.
The secondary objective was to evaluate the usefulness of prophylactic mesh in the prevention of EI hernias.
MethodsOur study was based on the retrospective analysis of a cohort of patients treated surgically between January 2015 and December 2016 for colorectal cancer.
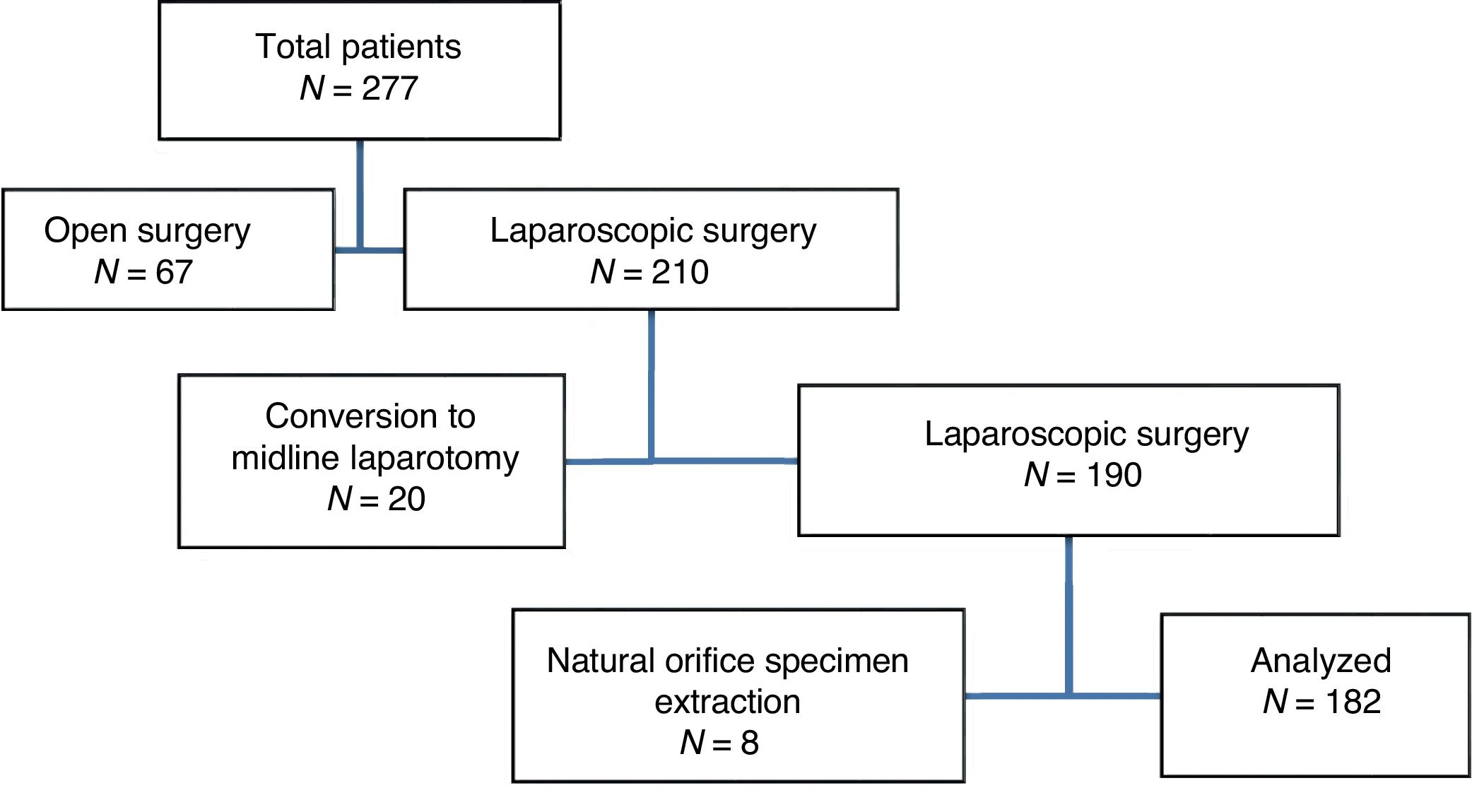
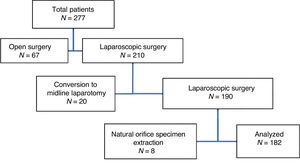
Patient files were reviewed after elective surgery for colon and rectal cancer in the indicated study period. We excluded patients who initially underwent open surgery, patients who required conversion and patients in whom the piece was removed without an EI (Fig. 1).
All patients had colon preparation with polyethylene glycol, thromboembolic prophylaxis with low-molecular-weight heparin and antibiotic prophylaxis with gentamicin and metronidazole.
The patients included were classified into 2 groups according to the type of EI: MI and TI. In turn, 2 different subgroups were created in the MI group according to the use of prophylactic mesh: MI with mesh (MIM) and MI with suture (MIS).
The closure of the EI was performed in all cases with continuous polydioxanone 1-gauge loop suture (PDS®, Ethicon, NJ, USA). In the TI group, the peritoneum was closed with a continuous 3/0 polyglactin suture (Vicryl® Ethicon, NJ, USA). In the MIM subgroup, with no specific protocol and at the discretion of the head surgeon in patients considered to be at high risk, a polyvinylidenfluoride mesh (Cicat®, DynaMesh, Aachen, Germany) was used in an onlay position and affixed with a ring of fascia staples (DFS® Autosuture, Covidien, MA, USA), adjusted to the size of the incision.
The trocar orifices greater than 5mm were closed with interrupted polyglactin gauge 1 stitches (Vicryl, Ethicon, NJ, USA).
We collected demographic data, patient medical history and risk factors, data about the surgery (duration, technique and intraoperative complications), postoperative complications grouped by the Clavien–Dindo classification23 and complementary treatment both before and after the oncological disease. The risk for developing IH was calculated especially for this study using the HERNIAscore17 scoring system, which applies the following formula: HERNIAscore=3×extraction incision+1×COPD+1×(BMI ≥25kg/m2). Three patient groups are established: low risk, 0–3 points; moderate risk, 4–5 points; and high risk, more than 6 points.
The diagnostic criteria for IH were: (1) repair of IH during follow-up; (2) clinical diagnosis of IH by the surgeon during postoperative follow-up, without surgical repair; (3) presence, in the last follow-up CT, of an interruption of the abdominal wall located in the area of the scar, accompanied by protrusion in the remaining patients.
CT scans were analyzed by a surgeon not involved in the surgical procedure. The cases that were classified as uncertain were reviewed by a radiologist as the second observer and were only considered positive with confirmation by the radiologist.
Statistical AnalysisThe statistical analysis was calculated with the SPSS 20.0 program (IBM Inc. Rochester, MN, USA). Quantitative variables are presented as mean±standard deviation, and qualitative variables are presented as proportions. The association between qualitative variables was analyzed using contingency tables (chi-squared and Fisher's exact test, when necessary) and quantitative variables, using the Student's t test for unpaired data or the Mann–Whitney test when necessary. Normal distribution of the quantitative variables was verified by the Kolmogorov–Smirnov test. Statistical significance was established at P<.05. The odds ratio for IH occurrence for each group and their confidence intervals were calculated.
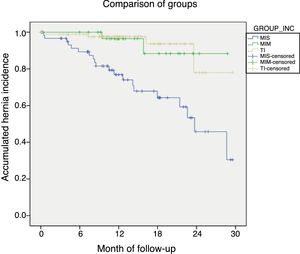
The risk of IH over time was calculated for both the entire population and for subgroups derived from a predictive variable using the nonparametric Kaplan–Meier estimator, considering the survival function as the proportion of patients with an abdominal wall without hernia.
The study was developed following international standards and guidelines for clinical research (code of ethics and Declaration of Helsinki) and in accordance with legal regulations for confidentiality and personal data.
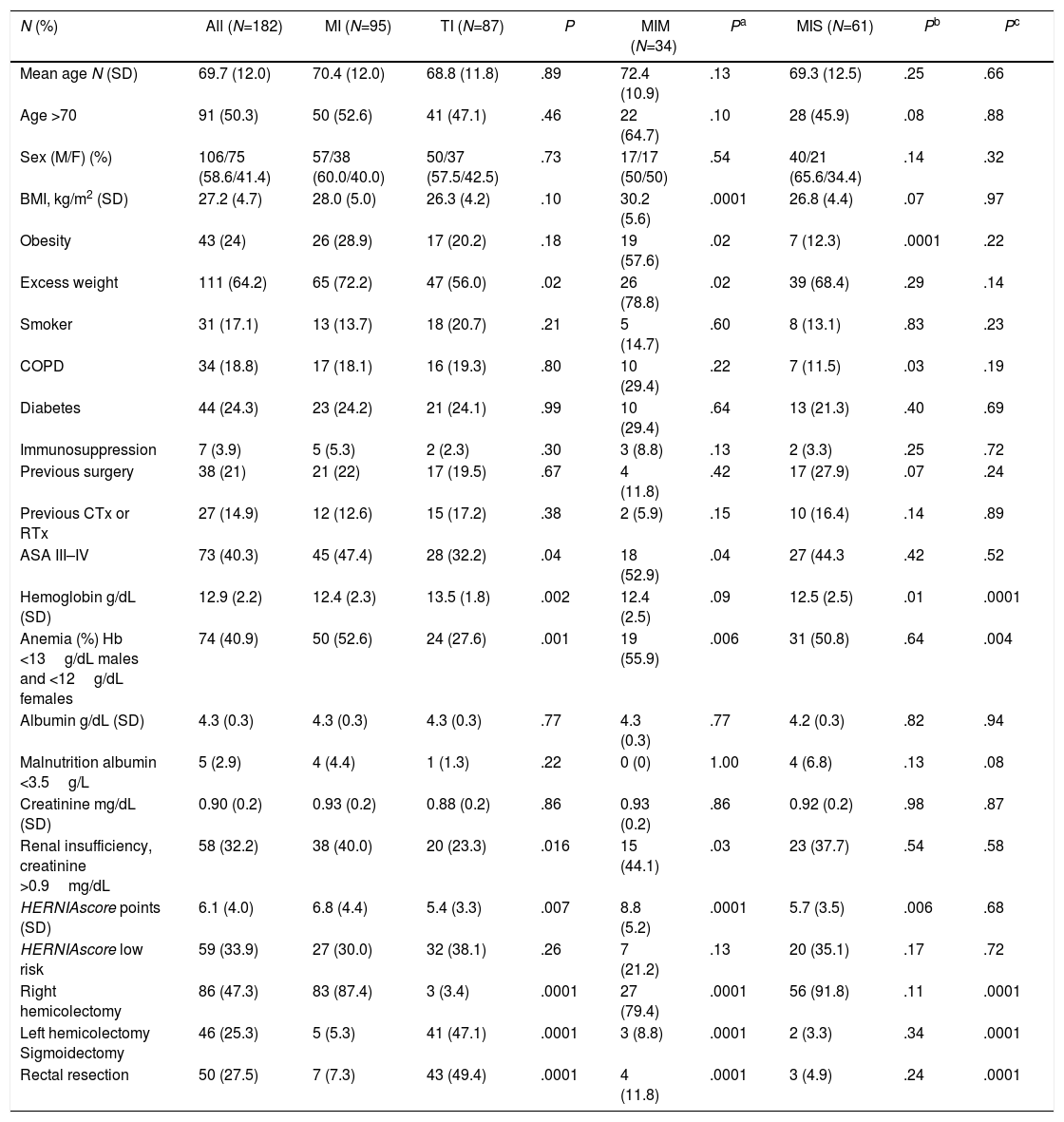
ResultsDuring the study period, 210 patients were treated laparoscopically, 182 of whom met the inclusion criteria (Fig. 1). Table 1 demonstrates the characteristics of the cohort and the patient groups/subgroups with midline incisions (MI) according to whether mesh was used (MIM) or not (MIS) and respective comparisons with the patients who had TI.
Characteristics of the Series and Comparison of the Groups and Subgroups.
| N (%) | All (N=182) | MI (N=95) | TI (N=87) | P | MIM (N=34) | Pa | MIS (N=61) | Pb | Pc |
|---|---|---|---|---|---|---|---|---|---|
| Mean age N (SD) | 69.7 (12.0) | 70.4 (12.0) | 68.8 (11.8) | .89 | 72.4 (10.9) | .13 | 69.3 (12.5) | .25 | .66 |
| Age >70 | 91 (50.3) | 50 (52.6) | 41 (47.1) | .46 | 22 (64.7) | .10 | 28 (45.9) | .08 | .88 |
| Sex (M/F) (%) | 106/75 (58.6/41.4) | 57/38 (60.0/40.0) | 50/37 (57.5/42.5) | .73 | 17/17 (50/50) | .54 | 40/21 (65.6/34.4) | .14 | .32 |
| BMI, kg/m2 (SD) | 27.2 (4.7) | 28.0 (5.0) | 26.3 (4.2) | .10 | 30.2 (5.6) | .0001 | 26.8 (4.4) | .07 | .97 |
| Obesity | 43 (24) | 26 (28.9) | 17 (20.2) | .18 | 19 (57.6) | .02 | 7 (12.3) | .0001 | .22 |
| Excess weight | 111 (64.2) | 65 (72.2) | 47 (56.0) | .02 | 26 (78.8) | .02 | 39 (68.4) | .29 | .14 |
| Smoker | 31 (17.1) | 13 (13.7) | 18 (20.7) | .21 | 5 (14.7) | .60 | 8 (13.1) | .83 | .23 |
| COPD | 34 (18.8) | 17 (18.1) | 16 (19.3) | .80 | 10 (29.4) | .22 | 7 (11.5) | .03 | .19 |
| Diabetes | 44 (24.3) | 23 (24.2) | 21 (24.1) | .99 | 10 (29.4) | .64 | 13 (21.3) | .40 | .69 |
| Immunosuppression | 7 (3.9) | 5 (5.3) | 2 (2.3) | .30 | 3 (8.8) | .13 | 2 (3.3) | .25 | .72 |
| Previous surgery | 38 (21) | 21 (22) | 17 (19.5) | .67 | 4 (11.8) | .42 | 17 (27.9) | .07 | .24 |
| Previous CTx or RTx | 27 (14.9) | 12 (12.6) | 15 (17.2) | .38 | 2 (5.9) | .15 | 10 (16.4) | .14 | .89 |
| ASA III–IV | 73 (40.3) | 45 (47.4) | 28 (32.2) | .04 | 18 (52.9) | .04 | 27 (44.3 | .42 | .52 |
| Hemoglobin g/dL (SD) | 12.9 (2.2) | 12.4 (2.3) | 13.5 (1.8) | .002 | 12.4 (2.5) | .09 | 12.5 (2.5) | .01 | .0001 |
| Anemia (%) Hb <13g/dL males and <12g/dL females | 74 (40.9) | 50 (52.6) | 24 (27.6) | .001 | 19 (55.9) | .006 | 31 (50.8) | .64 | .004 |
| Albumin g/dL (SD) | 4.3 (0.3) | 4.3 (0.3) | 4.3 (0.3) | .77 | 4.3 (0.3) | .77 | 4.2 (0.3) | .82 | .94 |
| Malnutrition albumin <3.5g/L | 5 (2.9) | 4 (4.4) | 1 (1.3) | .22 | 0 (0) | 1.00 | 4 (6.8) | .13 | .08 |
| Creatinine mg/dL (SD) | 0.90 (0.2) | 0.93 (0.2) | 0.88 (0.2) | .86 | 0.93 (0.2) | .86 | 0.92 (0.2) | .98 | .87 |
| Renal insufficiency, creatinine >0.9mg/dL | 58 (32.2) | 38 (40.0) | 20 (23.3) | .016 | 15 (44.1) | .03 | 23 (37.7) | .54 | .58 |
| HERNIAscore points (SD) | 6.1 (4.0) | 6.8 (4.4) | 5.4 (3.3) | .007 | 8.8 (5.2) | .0001 | 5.7 (3.5) | .006 | .68 |
| HERNIAscore low risk | 59 (33.9) | 27 (30.0) | 32 (38.1) | .26 | 7 (21.2) | .13 | 20 (35.1) | .17 | .72 |
| Right hemicolectomy | 86 (47.3) | 83 (87.4) | 3 (3.4) | .0001 | 27 (79.4) | .0001 | 56 (91.8) | .11 | .0001 |
| Left hemicolectomy Sigmoidectomy | 46 (25.3) | 5 (5.3) | 41 (47.1) | .0001 | 3 (8.8) | .0001 | 2 (3.3) | .34 | .0001 |
| Rectal resection | 50 (27.5) | 7 (7.3) | 43 (49.4) | .0001 | 4 (11.8) | .0001 | 3 (4.9) | .24 | .0001 |
ASA: American Society of Anesthesiology; COPD: chronic obstructive pulmonary disease; BMI: body mass index; CTx: chemotherapy; RTx: radiotherapy.
MI were used more frequently in resections of the right colon (87.4%) while TI were used in resections of the left colon (47.1%) and rectum (49.4%). MI were always implemented in the region of the navel, and TI were used for suprapubic sites (N=83).
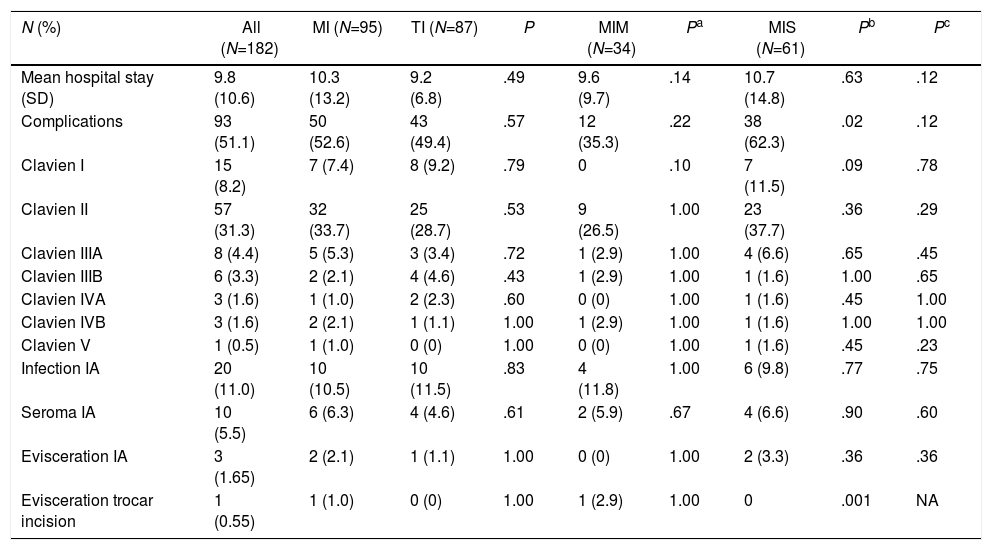
Table 2 shows the distribution of complications by groups and subgroups. The only complication that presented a statistically significant difference was the appearance of an evisceration of a trocar incision in the MIM group. In this group, no evisceration of the EI was detected, however, evisceration did appear in the 2 other groups with incidences of 3.3% (MIS) and 1.1% (TI), respectively.
Postoperative Evolution and Complications.
| N (%) | All (N=182) | MI (N=95) | TI (N=87) | P | MIM (N=34) | Pa | MIS (N=61) | Pb | Pc |
|---|---|---|---|---|---|---|---|---|---|
| Mean hospital stay (SD) | 9.8 (10.6) | 10.3 (13.2) | 9.2 (6.8) | .49 | 9.6 (9.7) | .14 | 10.7 (14.8) | .63 | .12 |
| Complications | 93 (51.1) | 50 (52.6) | 43 (49.4) | .57 | 12 (35.3) | .22 | 38 (62.3) | .02 | .12 |
| Clavien I | 15 (8.2) | 7 (7.4) | 8 (9.2) | .79 | 0 | .10 | 7 (11.5) | .09 | .78 |
| Clavien II | 57 (31.3) | 32 (33.7) | 25 (28.7) | .53 | 9 (26.5) | 1.00 | 23 (37.7) | .36 | .29 |
| Clavien IIIA | 8 (4.4) | 5 (5.3) | 3 (3.4) | .72 | 1 (2.9) | 1.00 | 4 (6.6) | .65 | .45 |
| Clavien IIIB | 6 (3.3) | 2 (2.1) | 4 (4.6) | .43 | 1 (2.9) | 1.00 | 1 (1.6) | 1.00 | .65 |
| Clavien IVA | 3 (1.6) | 1 (1.0) | 2 (2.3) | .60 | 0 (0) | 1.00 | 1 (1.6) | .45 | 1.00 |
| Clavien IVB | 3 (1.6) | 2 (2.1) | 1 (1.1) | 1.00 | 1 (2.9) | 1.00 | 1 (1.6) | 1.00 | 1.00 |
| Clavien V | 1 (0.5) | 1 (1.0) | 0 (0) | 1.00 | 0 (0) | 1.00 | 1 (1.6) | .45 | .23 |
| Infection IA | 20 (11.0) | 10 (10.5) | 10 (11.5) | .83 | 4 (11.8) | 1.00 | 6 (9.8) | .77 | .75 |
| Seroma IA | 10 (5.5) | 6 (6.3) | 4 (4.6) | .61 | 2 (5.9) | .67 | 4 (6.6) | .90 | .60 |
| Evisceration IA | 3 (1.65) | 2 (2.1) | 1 (1.1) | 1.00 | 0 (0) | 1.00 | 2 (3.3) | .36 | .36 |
| Evisceration trocar incision | 1 (0.55) | 1 (1.0) | 0 (0) | 1.00 | 1 (2.9) | 1.00 | 0 | .001 | NA |
EI: extraction incision.
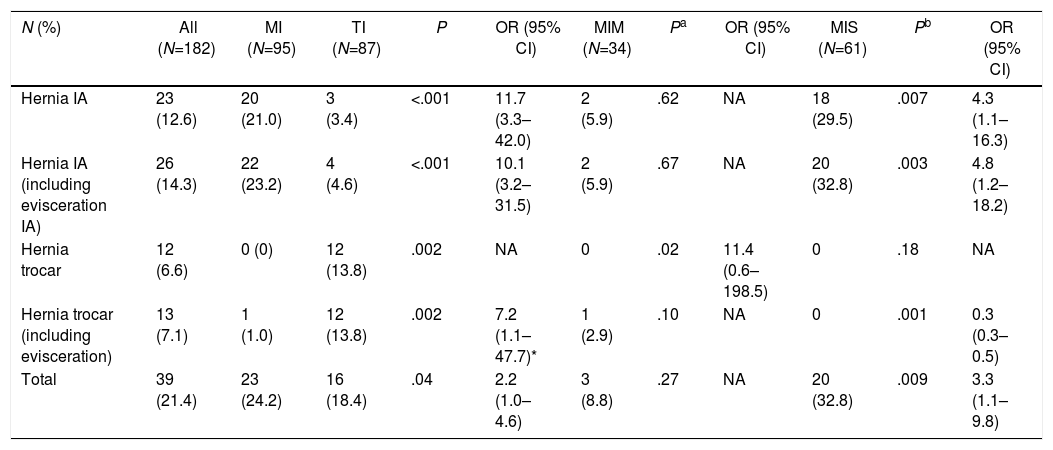
Table 3 presents a comparison between the different IH and their location by groups and subgroups after a median follow-up of 13.0 months (SD 6.2; 95% CI: 10.4–19.1 months). The lowest incidence of all types of IH appeared in the MIM group (8.8%). Regarding EI, the MIM and TI groups had similar frequencies of IH (MIM 5.9% vs TI 3.4%; P=.62), while the MIS group had the highest incidence (29.5%), with a 4 times greater probability of IH than the MIM group (OR 4.3; 95% CI: 1.1–16.3) that was almost 12 times greater than the TI group (OR 11.7; 95% CI: 3.3–42).
Incidence of Incisional Hernia by Groups and Subgroups.
| N (%) | All (N=182) | MI (N=95) | TI (N=87) | P | OR (95% CI) | MIM (N=34) | Pa | OR (95% CI) | MIS (N=61) | Pb | OR (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hernia IA | 23 (12.6) | 20 (21.0) | 3 (3.4) | <.001 | 11.7 (3.3–42.0) | 2 (5.9) | .62 | NA | 18 (29.5) | .007 | 4.3 (1.1–16.3) |
| Hernia IA (including evisceration IA) | 26 (14.3) | 22 (23.2) | 4 (4.6) | <.001 | 10.1 (3.2–31.5) | 2 (5.9) | .67 | NA | 20 (32.8) | .003 | 4.8 (1.2–18.2) |
| Hernia trocar | 12 (6.6) | 0 (0) | 12 (13.8) | .002 | NA | 0 | .02 | 11.4 (0.6–198.5) | 0 | .18 | NA |
| Hernia trocar (including evisceration) | 13 (7.1) | 1 (1.0) | 12 (13.8) | .002 | 7.2 (1.1–47.7)* | 1 (2.9) | .10 | NA | 0 | .001 | 0.3 (0.3–0.5) |
| Total | 39 (21.4) | 23 (24.2) | 16 (18.4) | .04 | 2.2 (1.0–4.6) | 3 (8.8) | .27 | NA | 20 (32.8) | .009 | 3.3 (1.1–9.8) |
EI: extraction incision.
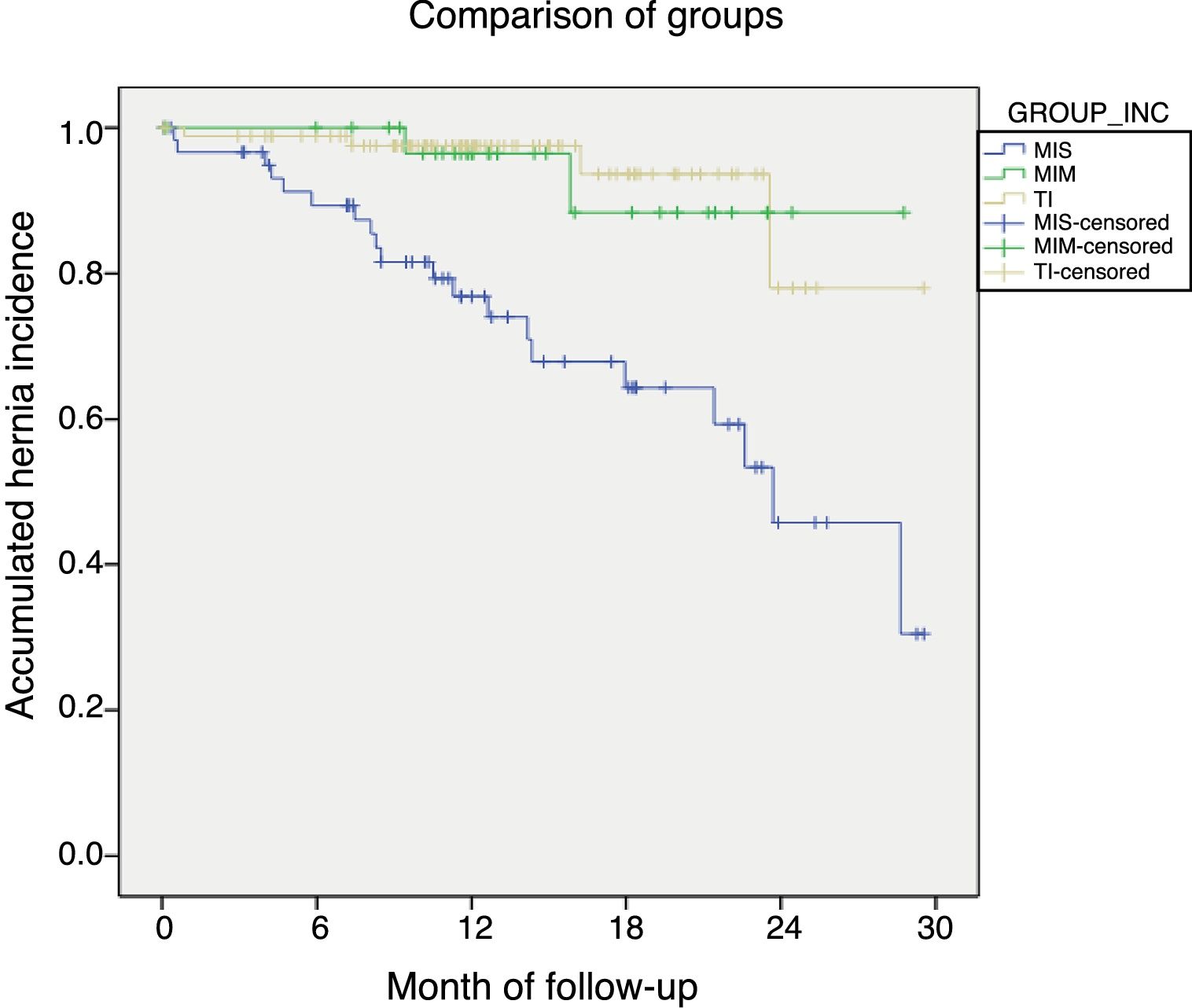
When these data were compared using Kaplan–Meier curves (Fig. 2), the cumulative risk for the appearance of hernias was statistically significant in the MIS group compared to the MIM (log-rank 8.86; P=.003; OR 28.3; 95% CI: 18.83–38.43) and with the TI (log-rank 23.7; P<.001; OR 27.0; 95% CI: 19.98–27.42). In contrast, the comparison between the MIM and TI groups showed similar curves without statistical significance (log-rank 0.07; P=.79).
DiscussionThe data provided by our study confirm that the laparoscopic approach for resection of colon cancer presents, when preventive measures are not used, an IH rate similar to that of open surgery, as has already been indicated by other studies.7,11 In fact, data from the National Incisional Hernia Registry24 show a high frequency of hernia operations related with a previous laparoscopy.
The statistical comparison of the patient characteristics (Table 1) shows significant differences in some parameters considered risks for the development of IH, such as excess weight, anemia and renal failure. This aspect is very well reflected when comparing the HERNIAscore of the two groups, which was also significant. In contrast, when comparing the percentage of patients from the group considered low risk by the HERNIAscore, these differences disappeared (Table 1). This difference has its origin in a higher percentage of high-risk patients in the MI group (MI 48.9% vs TI 32.1%, P=.025).
The comparison of the MIS subgroup with the TI group did not show significant differences other than the presence of a higher percentage of patients with anemia. However, the percentage of high-risk patients did not have significant differences (MIS 40.4% vs TI 32.1%; P=.32), so the results of both groups in terms of incidence of IH are comparable.
Like previous studies,11–15 our study corroborates that the use of an MI for the extraction of the piece is accompanied by a greater frequency of EI hernias than when using a TI. In fact, the guidelines of the European Hernia Society (EHS) for laparotomies25 recommend avoiding MI to reduce the frequency of IH. The suprapubic Pfannenstiel incision seems optimal for this purpose, as stated by other authors.13
Trocar site hernias also frequently occurred after laparoscopy in the cases analyzed (6.6%). Unexpectedly, the frequency of trocar hernias was higher in the TI group (13.8%); only one was detected in the MI group, which was associated with evisceration. This is reflected in a higher probability of trocar hernias in TI (OR 7.2; 95% CI=1.1–47.7). In our opinion, this is not due to a protective effect of the EI type, but caused by other factors, especially technical, because when we compared the incidence of hernias by groups according to the HERNIAscore, the frequency of trocar hernia did not show significant differences among them (low risk 3.4%; moderate risk 11.4%; high risk 8.5%).
The first measure to avoid these hernias is, of course, meticulous closure of the trocar site orifices. As indicated by the guidelines of the EHS,25 there are no comparative studies to recommend the closure technique, type of material or use of surgical mesh. However, a randomized prospective study done in cholecystectomies showed that the prophylactic use of mesh was accompanied by better results.26
Patients who received a prophylactic mesh presented a significantly higher percentage of obesity, chronic obstructive pulmonary disease and anemia, as well as a significantly higher HERNIAscore, which is clearly reflected when comparing patients in the group considered high risk with scores above 6 (MIM 63.6% vs MIS 40.4%; P=.033). This correlates the fact that prophylactic mesh was used only in the MI at the discretion of the surgeon, without any type of protocol. The surgeons who opted for prophylaxis were guided by the algorithm that we apply with good results in midline laparotomies.20 In these higher risk patients, this measure was effective and safe to prevent EI hernias, without presenting a greater number of general or wound-related complications, as has already been described in previous studies.20–22 Likewise, no evisceration occurred in this group, compared to 3.3% in the MIS group; however, the differences were not significant, probably because of the sample size.
In the groups that received sutures (MIS and TI) and had similar characteristics in terms of their risk factors, IH were much more frequent in the MI than in the TI, so it can be inferred that the location of the incision was a key factor to decrease the number of hernias detected during follow-up. A recent randomized study15 that compared midline incisions with lateral TI only succeeded in demonstrating a lower incidence of IH in TI in the analysis by protocol, since in the comparison by intention of treatment significance was not reached after one year of follow-up due to a high number of protocol violations. For all these reasons, future randomized studies should be expected in order to definitively clarify the superiority of TI over MI for EI.
In the present study, the analysis using Kaplan–Meier curves shows that the MIM group, despite having a greater number of risk factors, is equal to the TI in terms of the accumulated risk for the appearance of IH, while the MIS group has the worst prognosis. This result supports the hypothesis that TI is superior to MI in terms of lower frequency of IH and that prostheses in MI achieve results similar to TI.
A weak point of our study is that the short stitches or ‘small bite’ closure technique was not used for the incisions; this method was introduced very recently, but there are already reports of fewer hernias with its use.27,28 Therefore, future comparative studies should be done based on a closure that follows this technique, as recommended by the EHS guidelines.25 However, this limitation is also shared by other studies carried out to date.11,12,15
The second limitation is that it is not a prospective study, so, in view of our results, it is clear that one or several randomized trials will be necessary in the future to: (1) definitively determine whether the TI is superior to the MI; (2) compare various TI among themselves (lateral and midline); and (3) determine whether prophylactic measures are necessary and in which incisions they are most appropriate.
Until such studies have been completed, and in light of what we have reported, we consider the location of the incision to be relevant and recommend the preferential use of TI in patients who are undergoing laparoscopic colon resection. MI should be reserved for cases in which TI is technically not possible.
If an MI is used, the surgeon should evaluate the risk factors and, in cases where it is high, our research indicates the advantages and low morbidity when using a prosthesis to prevent IH.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Pereira JA, Pera M, López-Cano M, Pascual M, Alonso S, Salvans S, et al. Hernias de la incisión de asistencia tras resección colorrectal laparoscópica. Influencia de la localización de la incisión y del uso de una malla profiláctica. Cir Esp. 2019;97:20–26.