The good results obtained with the implementation of ambulatory laparoscopic cholecystectomy programs have led to the expansion of the initial inclusion criteria. The main objective was to evaluate the results and the degree of satisfaction of the patients included in a program of laparoscopic cholecystectomy without admission, with expanded criteria.
MethodsObservational study of a cohort of 260 patients undergoing ambulatory laparoscopic cholecystectomy between April 2013 and March 2016 in a third level hospital. We classified the patients into 2 groups based on compliance with the initial inclusion criteria of the outpatient program. Group I (restrictive criteria) includes 164 patients, while in group II (expanded criteria) we counted 96 patients. We compared the surgical time, the rate of failures in ambulatory surgery, rate of conversion, reinterventions and mortality and the satisfaction index.
ResultsThe overall success rate of ambulatory laparoscopic cholecystectomy was 92.8%. The most frequent cause of unexpected income was for medical reasons. There was no statistically significant difference between the 2 groups for total surgery time, the rate of conversion to open surgery and the number of major postoperative complications Do not demonstrate differences in surgical time, nor in the number of perioperative complications (major complications 1.2%), or the number of failures in ambulatory surgery, nor the number of readmissions between both groups. There was no death. 88.5% of patients completed the survey, finding no differences between both groups in the patient satisfaction index. The overall score of the process was significantly better in group II (P=.023).
ConclusionsAmbulatory laparoscopic cholecystectomy is a safe procedure with a good acceptance by patients with expanded criteria who were included in the surgery without admission program.
Los buenos resultados obtenidos con la implementación de los programas de colecistectomía laparoscópica ambulatoria han llevado a la ampliación de los criterios iniciales de inclusión. Como objetivo principal planteamos evaluar los resultados y el grado de satisfacción de los pacientes incluidos en un programa de colecistectomía laparoscópica sin ingreso, con criterios expandidos.
MétodosEstudio observacional de una cohorte de 260 pacientes intervenidos de colecistectomía laparoscópica ambulatoria entre abril del 2013 y marzo del 2016 en un hospital de tercer nivel. Clasificamos a los pacientes en 2grupos en función del cumplimiento de los criterios iniciales de inclusión del programa ambulatorio. El grupo I (criterios restrictivos) incluye a 164 pacientes, mientras que, en el grupo II, se incluyen 96 pacientes (criterios expandidos: no cumplían alguno de los criterios de selección). Comparamos el tiempo quirúrgico, la tasa de ingresos no deseados, tasa de conversión, reintervenciones, mortalidad y el índice de satisfacción.
ResultadosEl porcentaje global de éxito de la colecistectomía laparoscópica ambulatoria fue del 92,8%. La causa más frecuente de ingresos no esperados fue por causas médicas. No se objetivaron diferencias estadísticamente significativas entre los 2grupos en la duración del procedimiento quirúrgico, en la tasa de conversión a cirugía abierta, ni en el número de complicaciones mayores posquirúrgicas. Cumplimentaron la encuesta el 88,5% de los pacientes, no encontrando diferencias entre los 2grupos en el índice de satisfacción de los pacientes. La calificación global del proceso fue significativamente mejor en el grupo II (p=0,023).
ConclusionesLa colecistectomía laparoscópica ambulatoria es un procedimiento seguro y con una buena aceptación por parte del grupo de pacientes con criterios expandidos que fueron incluidos en el programa de cirugía sin ingreso.
The advantages observed in the postoperative period of laparoscopic cholecystectomy compared to the traditional laparotomy approach have led to widespread use of this technique in the surgical community, along with rapid acceptance.
Technological advances in the fields of surgery, anesthesiology and pharmacology, together with the need for improvements to the healthcare system, have favored the creation of alternative healthcare models to traditional hospitalization, including major ambulatory surgery (MAS). At the beginning of the 1990s, Reddick and Olsen1 first began conducting laparoscopic cholecystectomies (LC) as outpatient surgery. These authors demonstrated an optimization of healthcare resources due to the reduced need for hospital beds, which allowed for the number of interventions to be increased and consequently reduced the surgical waiting list. In this manner, they demonstrated an improvement in the quality of care thanks to the reduction of hospital infections and the smaller impact on the patients’ daily lives, all of which contributed to the sustainability of the national healthcare system.2,3 In subsequent years, other workgroups have published acceptable results for the percentage of ambulatory failure (1%–45%), together with extremely low rates of morbidity and mortality.4–10
But, these results come from very heterogeneous studies because there are no established selection criteria or homogeneous management/execution protocols.
Despite this, at the end of the 20th century in Spain, ambulatory management of laparoscopic cholecystectomy (LC) had not generally been accepted due to the reluctance of some surgeons because of the possible delay in detection, and therefore the resolution, of postoperative complications. This rejection was reflected in the survey conducted in 2006 by the Spanish Association of Surgeons (AEC), in which data were obtained from 37 hospitals with 426 patients undergoing LC surgery, only 3.8% of which had been treated in an MAS program. This survey revealed the very limited implementation of these programs in our country.11
A key factor in the development of an ambulatory surgery program is the criteria for patient inclusion. Inadequate patient selection could lead to an increase in the unplanned hospitalization rate and, therefore, failed ambulatory management. This variable defines the quality of the outpatient treatment process, and the percentages from different published series range from 1 to 39%. The main causes of unexpected hospital admission are postoperative symptoms (vomiting and abdominal pain), conversion to open surgery and the patient's feeling of insecurity about being discharged the same day of the intervention.12–15
Some authors have reached the conclusion that the patients with less likelihood of failed ambulatory treatment are those younger than 65 years of age with a preoperative anesthetic classification ASA grade I or II, no previous abdominal surgery, no history of having presented episodes of acute cholecystitis, and a surgery duration of less than 90min.1,16–24 They argue that the majority of postoperative complications are due to medical reasons (intolerance, nausea or vomiting, and pain), while serious complications, such as haemorrhage, biliary fistula or iatrogenic intestinal injury, are rare (0%–2%). The main causes of readmission or failure of ambulatory management are due to medical causes or social reasons.
Currently, there are studies that analyze cholecystectomy results in MAS with less restrictive criteria, including: age >65 years, previous episodes of acute cholecystitis or pancreatitis, and stable ASA III classification. These studies have observed no increase in serious complications, with ambulatory failure rates of up to 20.9%, readmission rates from 1.2 to 5%, reoperation rates <1% and conversion rates less than 2%.25–28
The experience gained after the implementation of the ambulatory LC (ALC) program by our Unit in 2010 led to the expansion of the initial criteria for patient inclusion.
The main objective of this study is to compare the results obtained in both groups of patients (restricted criteria and expanded criteria) treated in an ALC program.
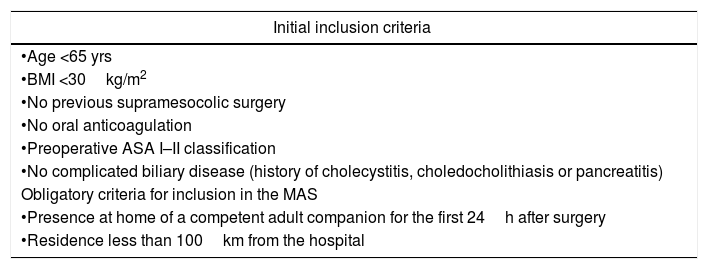
MethodsThis retrospective observational study was conducted between April 2013 and March 2016, analyzing a sample of 260 patients undergoing ALC. This sample was divided into 2 groups according to whether or not the initial inclusion criteria were met. These criteria are shown in Table 1. Patients who met all the selection criteria (restrictive criteria) were included in group I. Group II included patients who did not meet one of the selection criteria. The last 2 criteria were mandatory in the 2 groups of patients. Group I (initial criteria) included 164 patients, and group II (expanded criteria) included 96 cases.
Initial Selection Criteria.
| Initial inclusion criteria |
|---|
| •Age <65 yrs |
| •BMI <30kg/m2 |
| •No previous supramesocolic surgery |
| •No oral anticoagulation |
| •Preoperative ASA I–II classification |
| •No complicated biliary disease (history of cholecystitis, choledocholithiasis or pancreatitis) |
| Obligatory criteria for inclusion in the MAS |
| •Presence at home of a competent adult companion for the first 24h after surgery |
| •Residence less than 100km from the hospital |
ASA: American Society of Anesthesiologists preoperative risk score; MAS: major ambulatory surgery; BMI: body mass index.
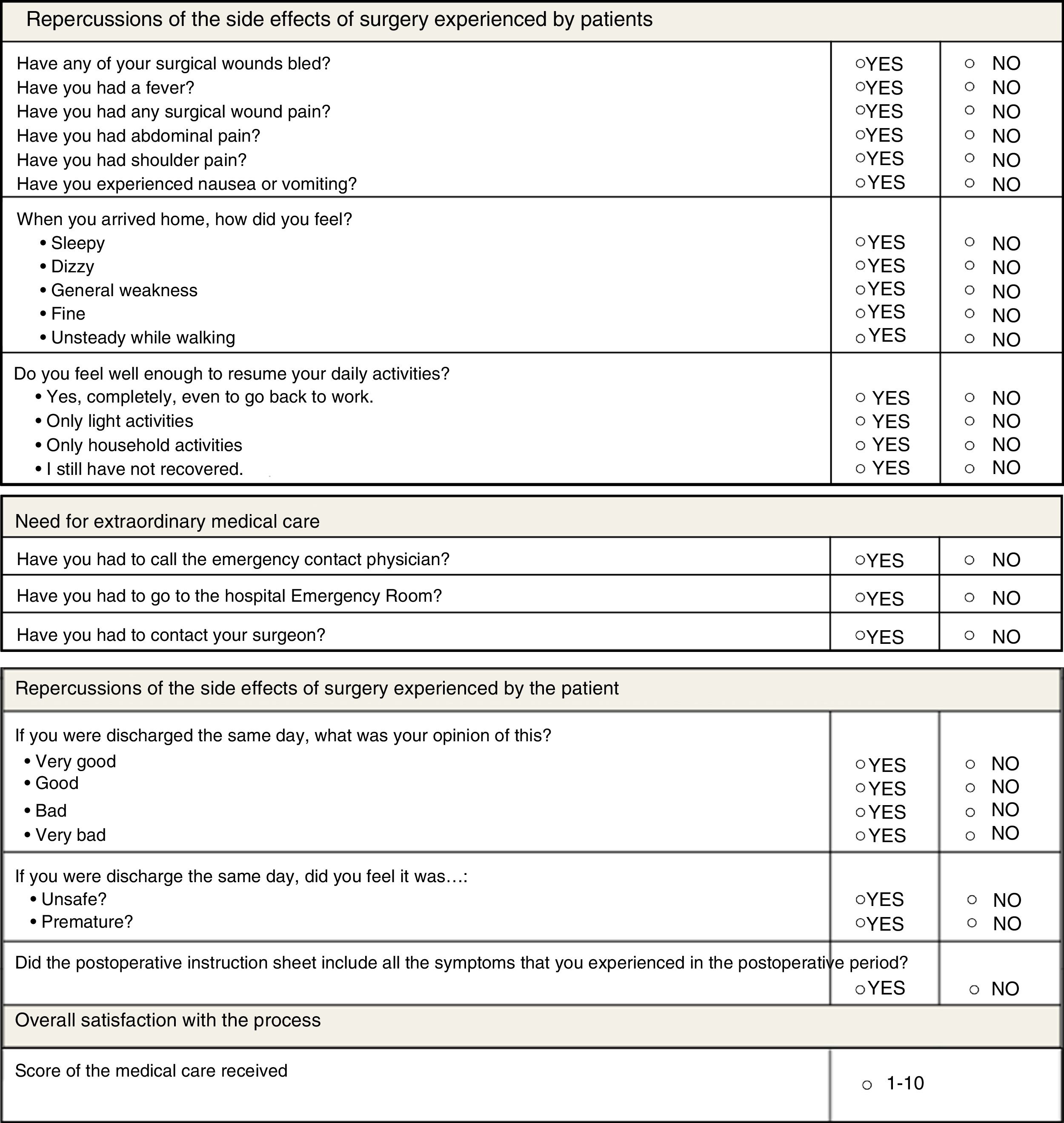
The variables analyzed were surgical time, postoperative morbidity and mortality, failure of ambulatory management, and patient satisfaction with the process. All patients were provided with a survey about their overall satisfaction with the program created by the MAS unit of the hospital, which was completed in either the outpatient consultation or over the telephone. The survey consisted of several sections and analyzed the postoperative symptoms and their impact on the patient, their degree of acceptance, their opinion about early discharge and their overall assessment of the treatment received. All the survey parameters are shown in Fig. 1.
All surgeries were scheduled in the morning, and the patients arrived at the hospital between 1 and 2h before the procedures, where the preoperative reception protocol was applied.
Postoperative management was based on a “fast track” regimen (anesthetic technique with laryngeal mask and low in opiates, administration of non-steroidal anti-inflammatory analgesia, antiemetic prophylaxis and multimodal analgesia).29–31 After surgery, the patient was transferred to the post-anesthesia recovery unit. Once the patient tolerated sitting and passed a score system based on the Aldrete criteria,32 the patient was transferred to the adaptation room to initiate oral intake of liquids and ambulation. After confirming that discharge criteria were met, patients were sent home with written postoperative instructions and a series of warning symptoms (fever over 38°C, excessive pain, swelling in the area of the surgical wound or significant bleeding and persistent vomiting despite medication).
All the patients who were discharged from the ambulatory treatment unit had a stay between 5 and 10h, since this unit is active from 9 am to 8 pm.
The following day, patients were visited by a physician from the home hospitalization unit to confirm their correct postoperative progress. In addition, all patients were scheduled for office visits in the Outpatient Consultations the 3rd to 4th weeks after hospital discharge.
Ambulatory treatment was considered a failure when the patient required transfer to the hospital ward or came to the emergency room within 24h and was admitted. The criteria for hospitalization of the patients were: conversion to open surgery, vital signs outside normal ranges, pain not controllable with oral analgesics, oral intolerance or patient refusal.
Statistical AnalysisThe qualitative variables are expressed as number of cases and percentages, while the quantitative variables are expressed as median, range, mean and standard deviation. To compare the qualitative variables, the χ2 test or the Fisher test was used, and the Student's t test was used for the quantitative variables. The statistical analysis was performed with IBM® SPSS® Statistics version 22.
ResultsDuring the period studied (April 2013 to March 2016), 598 LC were performed, 260 of which were included in the ambulatory surgery program.
The substitution rate of the series was 43%. In 2013 and 2014, 33.8% of the LC were ALC, while in 2015 and 2016 this percentage reached 55.7%.
The patients included in group II who exceeded only one expanded criterion were 93.75%, while 6.25% fulfilled 2 expanded criteria.
In the last 2 years of the study, more patients with expanded criteria were included than during the first 2 years (51 and 45 patients, respectively) representing 17 and 19.6% of ALC.
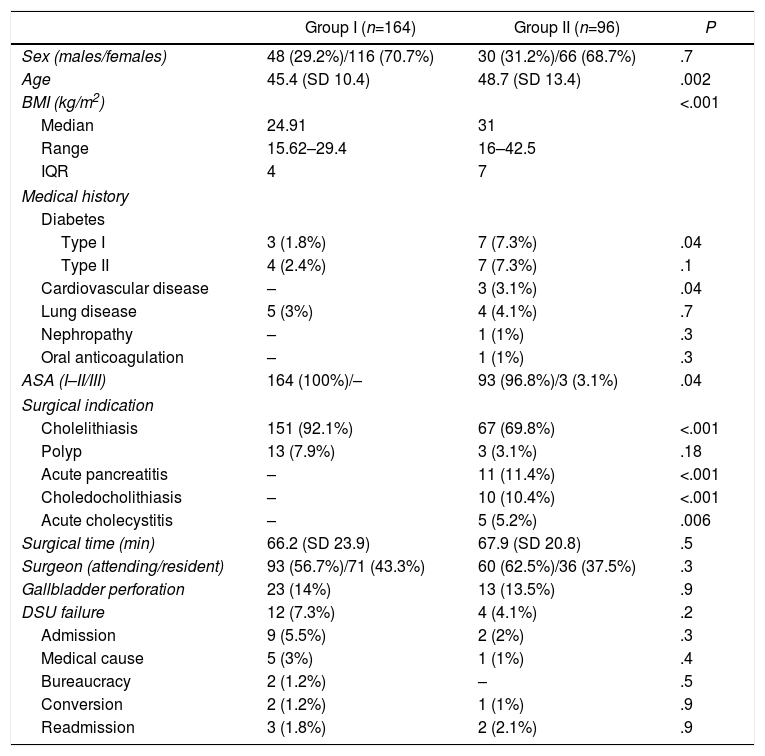
Table 2 shows the differences in the inclusion criteria in the 2 groups. The patients of the second group had a higher mean age and 16.6% were older than 65. The body mass index also increased in the second group, with a median of 31 (range 16–42.5). We also observed that 11.5% of patients in the 2nd group had class 2 obesity.
Characteristics of the Groups According to Compliance With the Initial Ambulatory Program Criteria.
| Group I (n=164) | Group II (n=96) | P | |
|---|---|---|---|
| Sex (males/females) | 48 (29.2%)/116 (70.7%) | 30 (31.2%)/66 (68.7%) | .7 |
| Age | 45.4 (SD 10.4) | 48.7 (SD 13.4) | .002 |
| BMI (kg/m2) | <.001 | ||
| Median | 24.91 | 31 | |
| Range | 15.62–29.4 | 16–42.5 | |
| IQR | 4 | 7 | |
| Medical history | |||
| Diabetes | |||
| Type I | 3 (1.8%) | 7 (7.3%) | .04 |
| Type II | 4 (2.4%) | 7 (7.3%) | .1 |
| Cardiovascular disease | – | 3 (3.1%) | .04 |
| Lung disease | 5 (3%) | 4 (4.1%) | .7 |
| Nephropathy | – | 1 (1%) | .3 |
| Oral anticoagulation | – | 1 (1%) | .3 |
| ASA (I–II/III) | 164 (100%)/– | 93 (96.8%)/3 (3.1%) | .04 |
| Surgical indication | |||
| Cholelithiasis | 151 (92.1%) | 67 (69.8%) | <.001 |
| Polyp | 13 (7.9%) | 3 (3.1%) | .18 |
| Acute pancreatitis | – | 11 (11.4%) | <.001 |
| Choledocholithiasis | – | 10 (10.4%) | <.001 |
| Acute cholecystitis | – | 5 (5.2%) | .006 |
| Surgical time (min) | 66.2 (SD 23.9) | 67.9 (SD 20.8) | .5 |
| Surgeon (attending/resident) | 93 (56.7%)/71 (43.3%) | 60 (62.5%)/36 (37.5%) | .3 |
| Gallbladder perforation | 23 (14%) | 13 (13.5%) | .9 |
| DSU failure | 12 (7.3%) | 4 (4.1%) | .2 |
| Admission | 9 (5.5%) | 2 (2%) | .3 |
| Medical cause | 5 (3%) | 1 (1%) | .4 |
| Bureaucracy | 2 (1.2%) | – | .5 |
| Conversion | 2 (1.2%) | 1 (1%) | .9 |
| Readmission | 3 (1.8%) | 2 (2.1%) | .9 |
ASA: American Society of Anesthesiologists preoperative risk score; SD: standard deviation; BMI: body mass index; IQR: interquartile range; DSU: day surgery unit.
Diabetes and heart disease were the most frequently diagnosed comorbidities among patients in group II. The history of complicated biliary disease, absent in group i, was present in 27% of the group II sample. The median time transpired between hospital admission for acute episode of pancreatitis or cholecystitis and the intervention was 62.5 days (range 3–228 days). All patients with choledocholithiasis underwent endoscopic retrograde cholangiopancreatography (ERCP). The median time between the therapeutic test and cholecystectomy was 30 days (range 3–126 days).
No differences were observed between the two groups in terms of surgical time, the number of failed ambulatory treatments and the number of readmissions. The overall percentage of successful ambulatory management was 92.8%. These patients had a stay in the postoperative recovery area from 5 to 10h, since the Day Surgery Unit has a schedule from 9 am until 8 pm.
The percentages of unplanned admission were 5.5 and 2% in group I and group II, respectively. The most frequent causes for which the patients required admission were medical, including nausea, vomiting and abdominal pain (5 patients from group I and one from group II).
The conversion rate was 1.2% in group I due to a common bile duct lesion, which was resolved with primary suture, ERCP and sphincterotomy, and another patient due to intestinal perforation, which was resolved with primary suture. In group II, the conversion rate was 1% due to poor visualization of Calot's triangle. These postoperative complications (major and minor) extended the mean hospital stay to 34.66h (SD 24.33) in group I and 36h (SD 16.97) in group II.
All the patients who required hospital admission in group II only presented one expanded criterion. We did not observe that the sum of the expanded criteria was a risk factor for readmission.
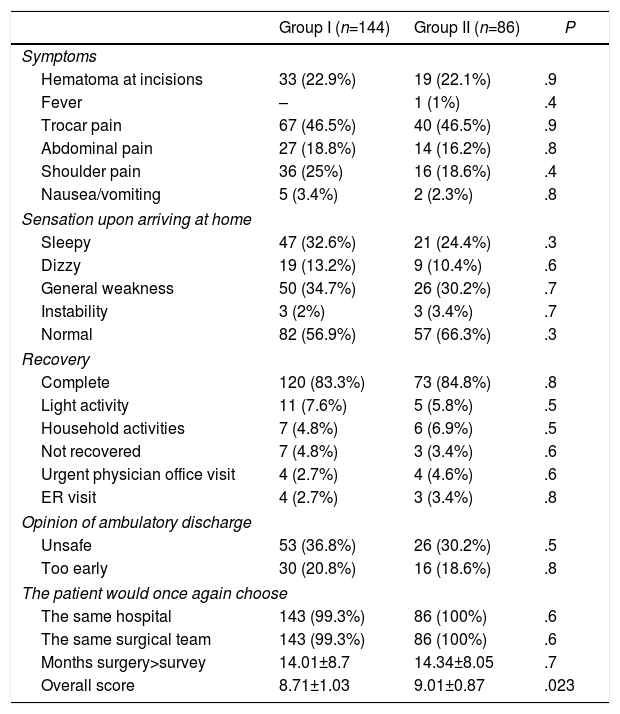
85.38% of the surveys were completed by telephone. The mean time between surgery and completing the survey was 14.01±8.7 months in group I and 14.34±8.05 in group II.
The survey was correctly completed by 87.80% of group I (144 out of 164 patients) and 89.58% of group II (86 of 96).
No differences were found regarding postoperative symptoms or satisfaction rate. The overall evaluation of the ambulatory treatment process was better in group II (P=.023) (Table 3).
Results of the Patient Satisfaction Survey.
| Group I (n=144) | Group II (n=86) | P | |
|---|---|---|---|
| Symptoms | |||
| Hematoma at incisions | 33 (22.9%) | 19 (22.1%) | .9 |
| Fever | – | 1 (1%) | .4 |
| Trocar pain | 67 (46.5%) | 40 (46.5%) | .9 |
| Abdominal pain | 27 (18.8%) | 14 (16.2%) | .8 |
| Shoulder pain | 36 (25%) | 16 (18.6%) | .4 |
| Nausea/vomiting | 5 (3.4%) | 2 (2.3%) | .8 |
| Sensation upon arriving at home | |||
| Sleepy | 47 (32.6%) | 21 (24.4%) | .3 |
| Dizzy | 19 (13.2%) | 9 (10.4%) | .6 |
| General weakness | 50 (34.7%) | 26 (30.2%) | .7 |
| Instability | 3 (2%) | 3 (3.4%) | .7 |
| Normal | 82 (56.9%) | 57 (66.3%) | .3 |
| Recovery | |||
| Complete | 120 (83.3%) | 73 (84.8%) | .8 |
| Light activity | 11 (7.6%) | 5 (5.8%) | .5 |
| Household activities | 7 (4.8%) | 6 (6.9%) | .5 |
| Not recovered | 7 (4.8%) | 3 (3.4%) | .6 |
| Urgent physician office visit | 4 (2.7%) | 4 (4.6%) | .6 |
| ER visit | 4 (2.7%) | 3 (3.4%) | .8 |
| Opinion of ambulatory discharge | |||
| Unsafe | 53 (36.8%) | 26 (30.2%) | .5 |
| Too early | 30 (20.8%) | 16 (18.6%) | .8 |
| The patient would once again choose | |||
| The same hospital | 143 (99.3%) | 86 (100%) | .6 |
| The same surgical team | 143 (99.3%) | 86 (100%) | .6 |
| Months surgery>survey | 14.01±8.7 | 14.34±8.05 | .7 |
| Overall score | 8.71±1.03 | 9.01±0.87 | .023 |
The current acceptance of MAS has been possible thanks to the improvement of surgical techniques, advances in pharmacology and anesthesiology and the development of home hospitalization units.
In the development of an MAS program, the patient selection criteria have a clear impact on the hospital admission rate, which is a reflection of the quality of the program.
In our series, 92.8% of the patients were discharged on the same day of the intervention. Only 7.2% of cases needed hospital admission (5.5% in group i and 2% in group II). Our results are similar to those published in other series with similar inclusion criteria.27,28,33
We recorded a readmission rate of 3.9% (2.1% in group II) and a conversion rate of 2.2% (1.2% and 1.04% in group i and ii, respectively). These data agree with what is published in the literature.25–28
When we started the ambulatory LC program, the inclusion criteria were stricter than at present, with the intention to minimize the percentage of unexpected admission or the appearance of a postoperative complication.
As more experience has been gained in the ALC program, the inclusion criteria have been reviewed and agreed upon with anesthesiologists, making them more flexible and broader in order to encompass patient groups that were previously not considered suitable for ambulatory treatment. All patients were evaluated preoperatively in the pre-anesthesia office visit, and, in addition to the surgeons, the anesthesiologists were also a small group of professionals especially dedicated to this program.
This review found no differences between the group of patients who underwent ALC with and without expanded criteria for the following variables: surgical time, number of conversions to open surgery and unplanned admissions.
We believe that using a satisfaction survey is essential to assess patient needs and expectations, in addition to defining their degree of perceived satisfaction. In this series, we observed that only 6.5% of the patients indicated that they thought discharge had been too early, and 33.9% felt insecure because they had not been hospitalized. Despite this, the degree of satisfaction was high and similar in both groups. It should be mentioned that the overall rating of the care received was significantly better in the group with expanded criteria.
This study has limitations, mainly because it is a retrospective and non-randomized study, with no calculated sample size. There is probably patient selection bias, since their inclusion in the MAS program was the decision of the surgeon. There may be a historical bias, since all patients in group II were operated on in the last 2 years of the study and most patients in group I were included at the beginning of the period. Therefore, it is logical that the experience of our group would have improved toward the end of the study, which may have influenced the results.
From our experience, we can affirm that ALC is a safe procedure with good acceptance by patients included with expanded criteria. We have found no differences in the quality indices for the immediate postoperative period or in the degree of satisfaction and acceptance of patients, despite being a group with greater ambulatory failure. In addition, with this observational study, we have obtained ambulatory failure and readmission rates for our setting, which will allow us to have reference values for future studies.
To corroborate this working hypothesis, a clinical trial should be considered to eliminate patient selection biases, which invariably exist because ALC is not a widely used technique among the general population.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Sala-Hernández A, Granero Castro P, Montalvá Orón E, Maupoey Ibáñez J, García-Domínguez R, Bueno Lledó J, et al. Evaluación de la seguridad y satisfacción de los pacientes en un programa de colecistectomía laparoscópica ambulatoria con criterios expandidos. Cir Esp. 2019;97:27–33.