Persistent peritoneal-vaginal duct can lead to the appearance of four pathologies, depending on the degree of its obliteration: inguinoscrotal hernia, communicating hydrocele, simple hydrocele or spermatic cord cyst. Likewise, it is associated with cryptorchidism and anomalies in the development of the epididymis.1
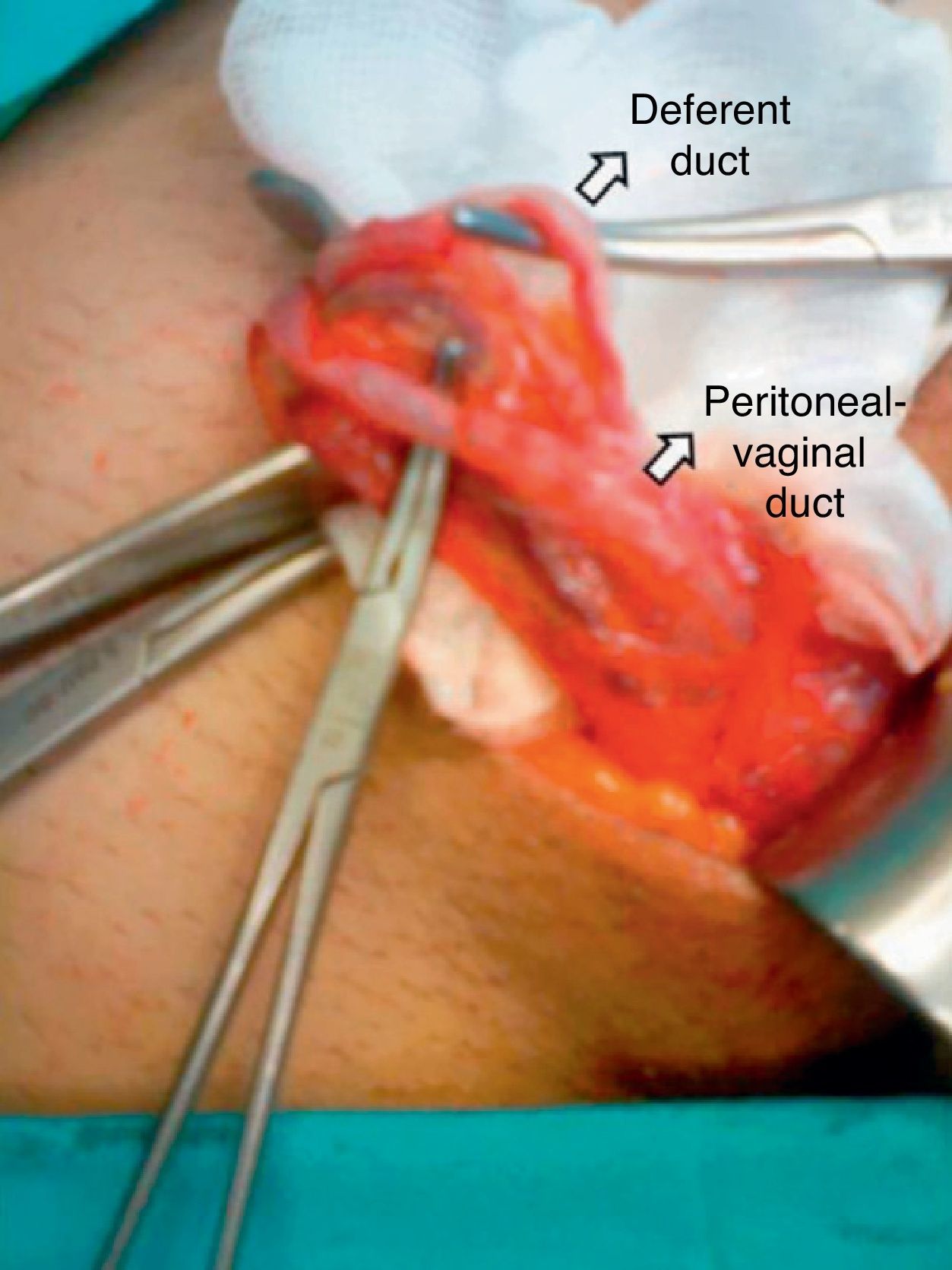
We present the case of a 40-year-old male patient with a history of renal failure secondary to renal polycystosis. He initiated a program of peritoneal dialysis, and we immediately observed passage of liquid to the right scrotal region. Physical examination ruled out the existence of an inguinal hernia. A scrotal/abdominal ultrasound showed evidence of a right communicating hydrocele. With the initial diagnosis of permeable embryonic vaginal process, we decided on surgery to perform its resection. The procedure was begun with a right inguinal incision. We proceeded with the dissection of the spermatic cord with individualization of its elements and the observed existence of the permeable peritoneal-vaginal duct that measured 0.5cm in diameter (Fig. 1). The duct was resected with ligation and proximal dissection at the internal inguinal orifice and distal ligation and dissection at its scrotal end. Hernioplasty was carried out with a mesh plug in the internal inguinal ring. The patient was discharged and followed-up in the outpatient clinic without incident; peritoneal dialysis was re-initiated after one month, with no complications.
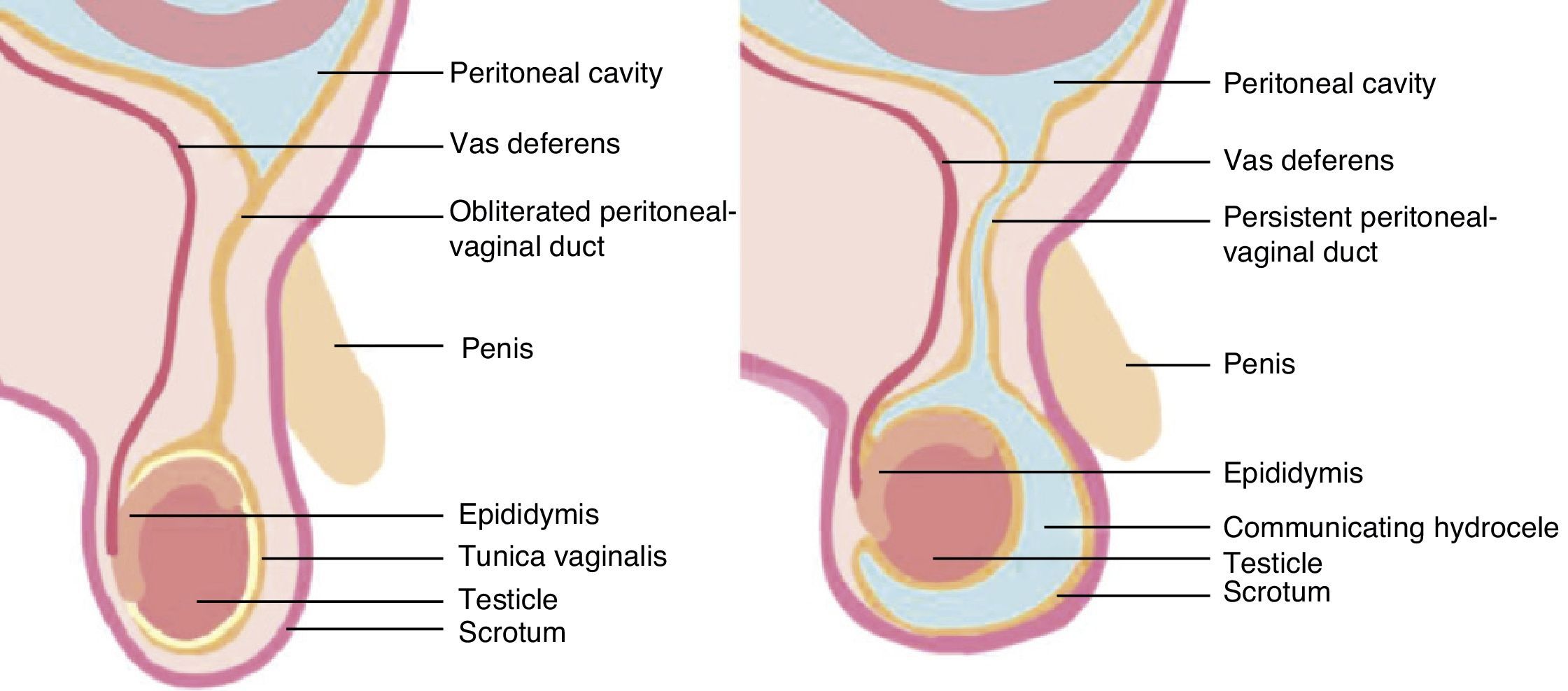
The formation of the peritoneal-vaginal duct is completed in the third month of gestation with evagination of the coelom on each side of the midline toward the scrotal fold. Between the third month and the end of gestation and directed by the fibers of the gubernaculum testis, the testicle descends from its primitive retroperitoneal location to the scrotal region. Afterwards, the vaginal process of the peritoneum is obliterated, forming a fibrous cord called the Cloquet ligament. The distal part of the duct becomes the tunica vaginalis of the testicle. In 40% of cases, this obliteration is completed in the last weeks of gestation. In the remaining 60%, it closes before the end of the first year of life.2
Persistent peritoneal-vaginal duct in males (Canal of Nuck in females) is a cause of indirect inguinal hernias (Fig. 2), with an incidence ranging between 0.8% and 4.4%. In premature babies, the incidence may reach 30% because the closure of the duct can take place during the first months of life. In 60% of cases, the right side is affected, in 30% the left side and in 10% the hernias are bilateral.3 Congenital inguinal hernia repair basically consists of the ligation of the hernia sac at the internal inguinal ring. It is not usually necessary to repair the inguinal floor. Communicating hydrocele is secondary to the complete permeability of the vaginal process and should be repaired in the same manner as an indirect inguinal hernia. Non-communicating hydrocele can sometimes be observed, and the need for surgical intervention can be assessed in cases with deficient resolution and increasing size.4
Peritoneal dialysis is a technique equivalent to hemodialysis for renal failure that provides patients with a greater quality of life. There are, however, a series of contraindications, such as peritoneal leaks or irreparable hernias, as they increase the risk of infections.5 Furthermore, the complications derived from the use of the technique include infections and increased intraabdominal pressure, the latter of which can lead to the appearance of hernias (inguinal, umbilical, diaphragmatic, obturator, peri-catheter) and hydrocele or genital edema,6 as in the case described.
In conclusion, persistence of the peritoneal-vaginal duct can cause congenital pathologies of the inguinal-scrotal region and its non-obliteration can remain clinically silent for life or only become evident in special cases, such as the start of peritoneal dialysis. Thus, based on this case we can conclude that before including a patient in a peritoneal dialysis regime, the inguinal region should be examined in detail. When complications appear in patients who are undergoing ambulatory peritoneal dialysis, the imaging technique to be used is CT peritoneography, which offers excellent tissue contrast and multiplanar images for correct evaluation.7,8
Please cite this article as: Estalella L, Rodríguez-Otero C, Garriga J, Doñate T, Targarona E. Hidrocele tras diálisis peritoneal: Persistencia del conducto peritoneo-vaginal. 2014;92(6):443–444.