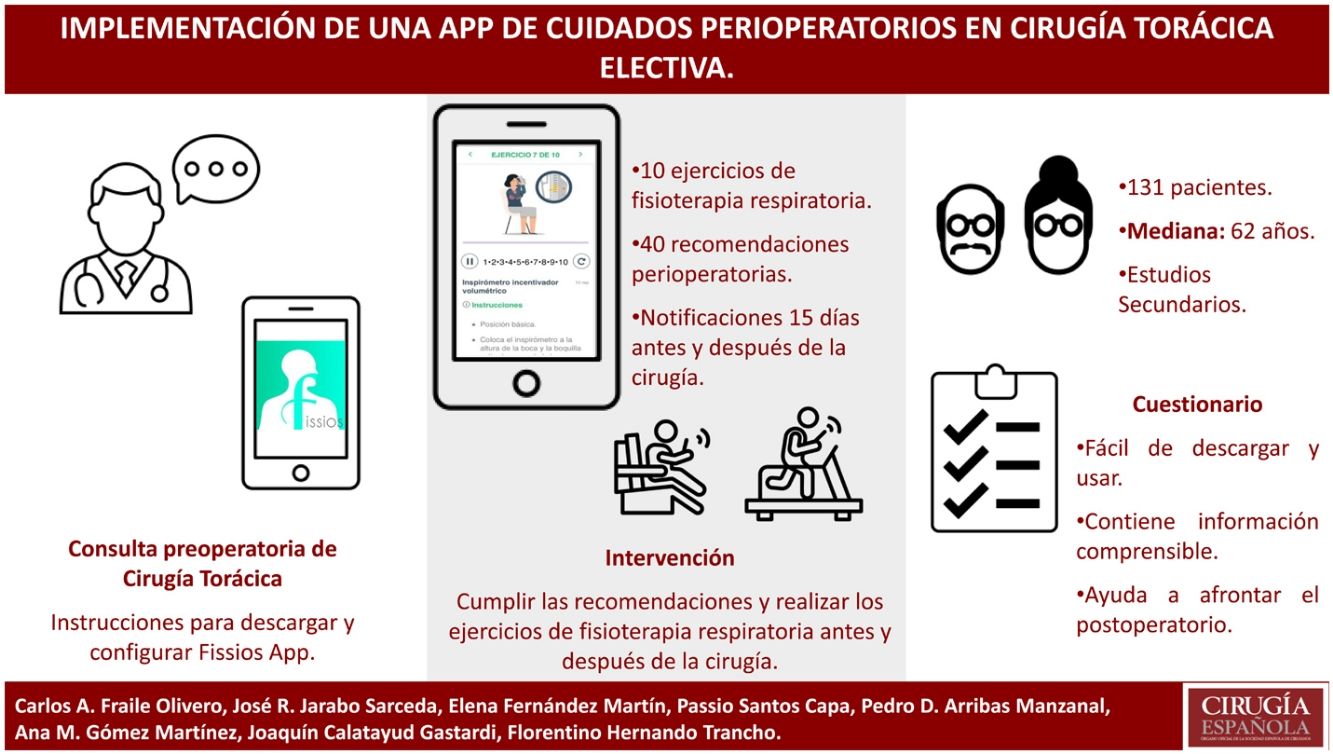
The design and implementation inconsistency of perioperative care programs limits their universalization, and it is where e-Health can standardize these processes. The objective of the study is to create a Smartphone App with a perioperative care program, implement it in a group of patients scheduled for a thoracic surgical procedure, and evaluates its use.
MethodsA prospective and descriptive study. We created a Smartphone app (Fissios App) which contains 40 perioperative recommendations and 10 chest physical exercises. Patients were recommended to use it before and after surgery; to measure its use, we created and applied a questionnaire. A descriptive analysis of patient variables and questionnaire responses was performed and their association evaluated.
ResultsOne hundred four patients were included, 60.3% were men with a median age of 62 years (51–71), and 26.72% had completed high school. The 89.3% of patients highlighted the ease of downloading and setting up the app. More than 90% of patients positively assessed clarity in explaining chest physical exercises and perioperative recommendations. One hundred four (79.4%) patients highlighted the contribution of the use of the app during the preoperative period to face the postoperative period.
ConclusionsWe created a Smartphone app (Fissios App) with a perioperative care program and it was successfully implemented regardless of the age or educational level of patients. The tool clearly explains the information contained and the patients reported that its use before surgery helped them to face the postoperative period, with an appropriate level of physical demand and time of use.
La inconsistencia en el diseño e implementación de los programas de cuidados perioperatorios limita su universalización, y es aquí donde las tecnologías en salud pueden estandarizar estos procesos. El objetivo del estudio es crear una app para smartphone con un programa de cuidados perioperatorios, implementarla en un grupo de pacientes programados para un procedimiento quirúrgico torácico y evaluar su utilización.
MétodosEstudio prospectivo y descriptivo. Se creó una app (Fissios App) que contiene 40 recomendaciones perioperatorias y un programa de 10 ejercicios de fisioterapia respiratoria. A los pacientes se les recomendó utilizarla antes y después de la cirugía; para medir su utilización se creó y se aplicó un cuestionario. Se realizó un análisis descriptivo de las variables de los pacientes, las respuestas del cuestionario y se evaluó su asociación.
ResultadosSe incluyeron 131 pacientes, el 60,3% eran varones con una mediana de edad de 62 años (51–71), y el 26,72% habían completado estudios secundarios. El 89,3% resaltaron la facilidad para descargar y configurar la app. Más del 90% de los pacientes valoraron positivamente la claridad para explicar los ejercicios respiratorios y las recomendaciones perioperatorias. Ciento cuatro (79,4%) pacientes destacaron la contribución del uso de la app para afrontar el postoperatorio.
ConclusionesSe creó una app (Fissios App) con un programa de cuidados perioperatorios y se implementó satisfactoriamente sin importar la edad ni el nivel educativo de los pacientes. La herramienta explica claramente la información contenida, y su uso antes de la cirugía les ayudó a afrontar el postoperatorio, con un nivel adecuado de exigencia física y de tiempo de uso.
Respiratory complications are a frequent cause of postoperative morbidity and mortality after thoracic surgery1, increasing the hospital stay2 and healthcare costs associated with thoracic procedures3. Respiratory therapy as part of a preoperative patient training program can reduce the risk of developing postoperative complications and optimize the patient’s physical condition4. These exercises, together with other strategies, such as smoking cessation, oral hygiene, pain control or early ambulation, have been shown to have a synergistic effect, improving postoperative results5.
The heterogeneity in the design and implementation of physiotherapy programs makes it difficult to demonstrate their effectiveness and generalize their actual benefits6. It is here where new technologies can standardize and homogenize these programs to achieve the stated objectives; advances in mobile technologies and apps have made it possible to monitor compliance with an exercise program, induce changes in patient behavior, improve lifestyle habits, and even help them meet their goals7,8. Although several apps have been published in thoracic surgery, none is aimed at the development of a perioperative care program or the prevention of postoperative complications9.
Respiratory therapy is an important strategy to reduce the risk of postoperative complications, and many limitations for its correct execution can be overcome with a healthcare tool supported by information technologies (e-Health). Thus, our aim was to create an app for smartphones, implement it in a group of surgical patients treated by the thoracic surgery service of a tertiary care hospital in Spain, and subsequently evaluate its use.
MethodsDevelopment of the ideaWe created a multidisciplinary working group of 7 thoracic surgeons, 2 physiotherapists, and a specialist in physical medicine and rehabilitation. We conducted a bibliographic review of respiratory therapy research during the perioperative period in order to design a homogeneous exercise program in terms of types of exercises, repetitions and duration. This also included a review of the strategies used to reduce the risk of developing postoperative complications. A consensus document was subsequently created with 10 exercises and 40 pre- and postoperative recommendations, which was unanimously approved (Appendix B, Supplementary material 1).
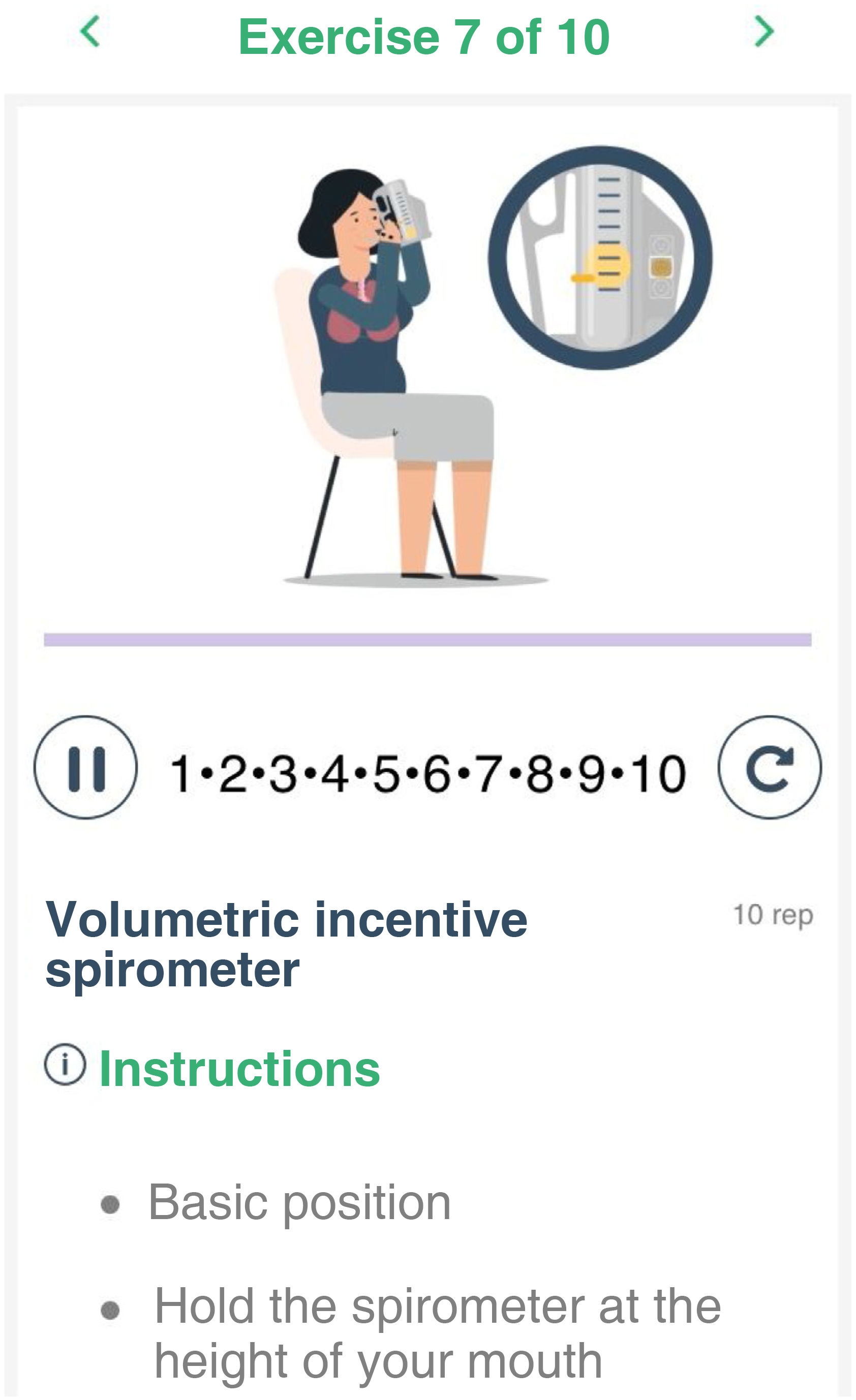
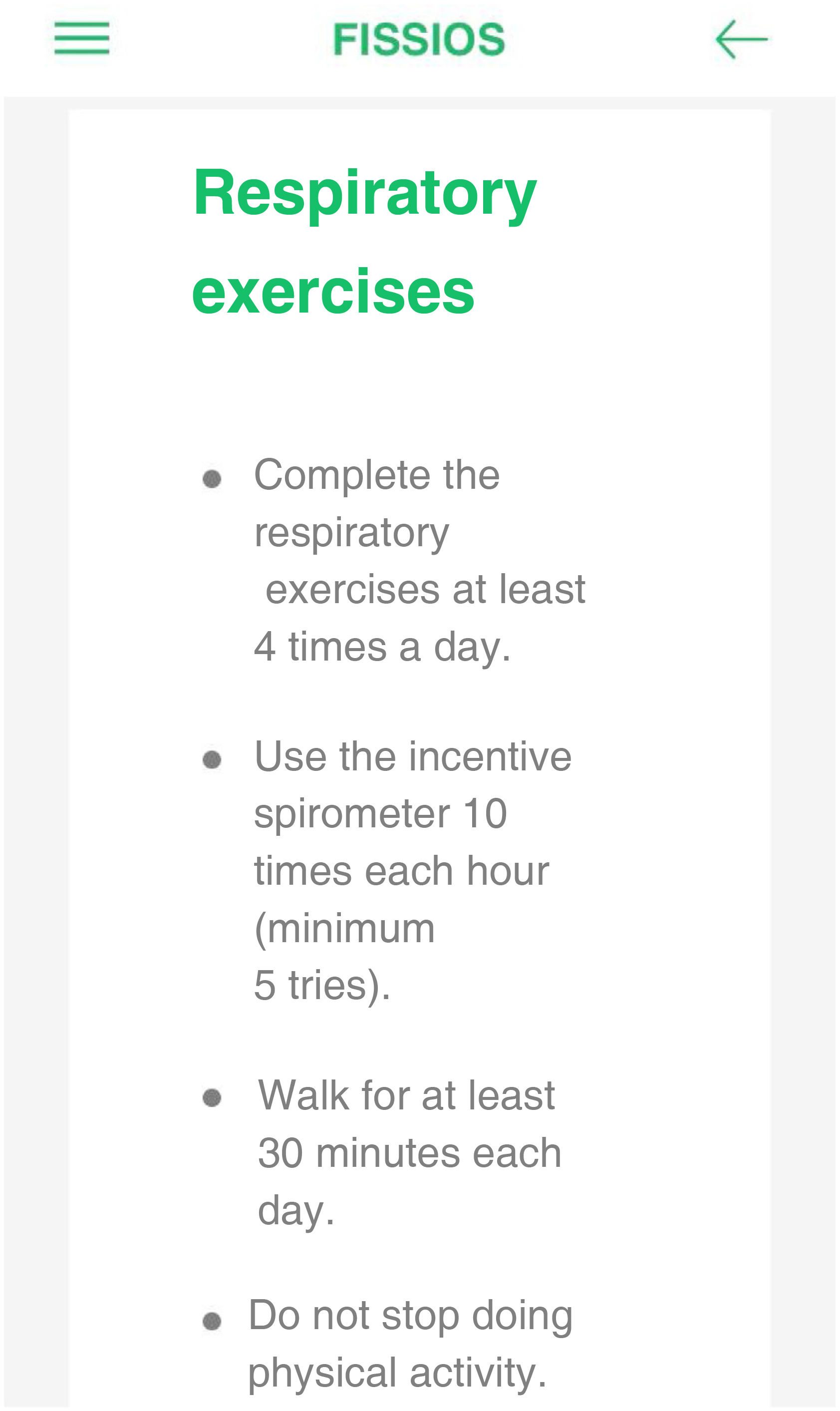
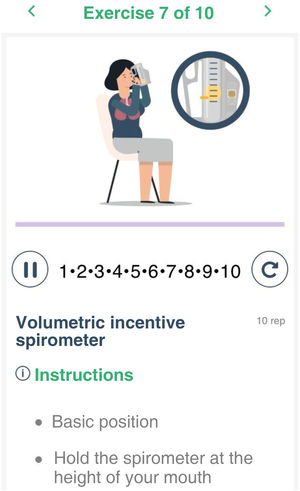
Creation of the appOnce the content was defined, we hired a specialized software engineering firm to program a multi-platform app that would be intuitive, easy-to-use and visually attractive for patients. Respiratory therapy exercises are explained with animated illustrations and a text panel. Each exercise has a duration and a set number of repetitions, controlled by a clock (Fig. 1). The pre- and postoperative recommendation sections are designed as drop-down windows and arranged in 10 sections (Fig. 2). A 22-megabyte app (Fissios App) was created, available for iOS® and Android® devices.
Screenshot of the app: respiratory therapy exercises. The upper panel makes it possible to change the exercises. The animation shows the ranges of movement of the exercise. The clock shows the number of repetitions or time that the patient should complete, with icons to start, pause or restart the clock. In the lower part, the text panel explains the instructions of the exercises.
A descriptive and prospective study was conducted in the thoracic surgery service of a tertiary care hospital in Spain from June 2017 to December 2018. The patients under study were all over 18 years of age, had an indication for elective thoracic surgery for diagnostic or therapeutic purposes, possessed a ‘smartphone’ mobile device, and were willing to use the tool to participate in the study. The exclusion criteria were defined as: (1) not having a compatible smartphone; (2) respiratory therapy exercises were contraindicated; (3) physical or psychological impediment of the patient to perform the exercises; and (4) refusal to participate in the study. We conducted a consecutive, non-probability sampling and followed the STROBE10 guidelines for reporting observational studies.
Sample sizeBased on the number of elective surgeries performed in 2017 (265 patients), the expected participation in the use of the tool (80%), an accuracy of 5% and a confidence level of 95%, it was necessary to include at least 128 patients.
Ethical considerationsAll patients included in the study signed an informed consent form. The study was approved by the Clinical Research Ethics Committee (CP-CI 16/117-E) and complies with the ethical principles for medical research involving human beings stipulated in the AMM Declaration of Helsinki.
ProcedurePatients were offered the possibility to participate in the study and use the app as an added complement to the preparation for surgery. Once their participation was accepted, verbal and written instructions were given on how to download and configure the app. All patients were assessed by the physical medicine and rehabilitation unit, following the standard protocol, and they attended face-to-face classes where they were trained to carry out respiratory therapy exercises. The intervention consisted of recommending the use of the app and urging patients to comply with the medical recommendations and with the respiratory therapy exercise program, with no restrictions regarding the time of usage, throughout the preoperative and postoperative period. At hospital discharge, patients were asked to complete the questionnaire.
Data collectionA 5-question questionnaire was created with 5 response options categorized by the Likert scale and ordered hierarchically (not at all, somewhat, moderately, very and extremely) (Table 1). Positive, neutral, or negative evaluations were interpreted according to the content of the question and the response options proposed.
Definitive questionnaire given to participating patients.
| Questionnaire to evaluate the use of the app | |
|---|---|
| Question | Response |
| How easy was it for you to obtain the app and initiate it? (install, personalize and use) | Not easy |
| Somewhat easy | |
| Moderately easy | |
| Rather easy | |
| Extremely easy | |
| How would you rate the clarity of the app to explain the respiratory exercises? | Not clear at all |
| Somewhat clear | |
| Moderately clear | |
| Very clear | |
| Extremely clear | |
| How would you rate the clarity of the general recommendations made by the app? | Not clear at all |
| Somewhat clear | |
| Moderately clear | |
| Very clear | |
| Extremely clear | |
| In general, how did the postoperative use of the app contribute towards your recovery? | Not at all |
| A little | |
| Adequately | |
| A lot | |
| Too much | |
| In general, would you consider the physical level and time of use of the app demanding? | Not at all |
| A little | |
| Adequately | |
| A lot | |
| Too much | |
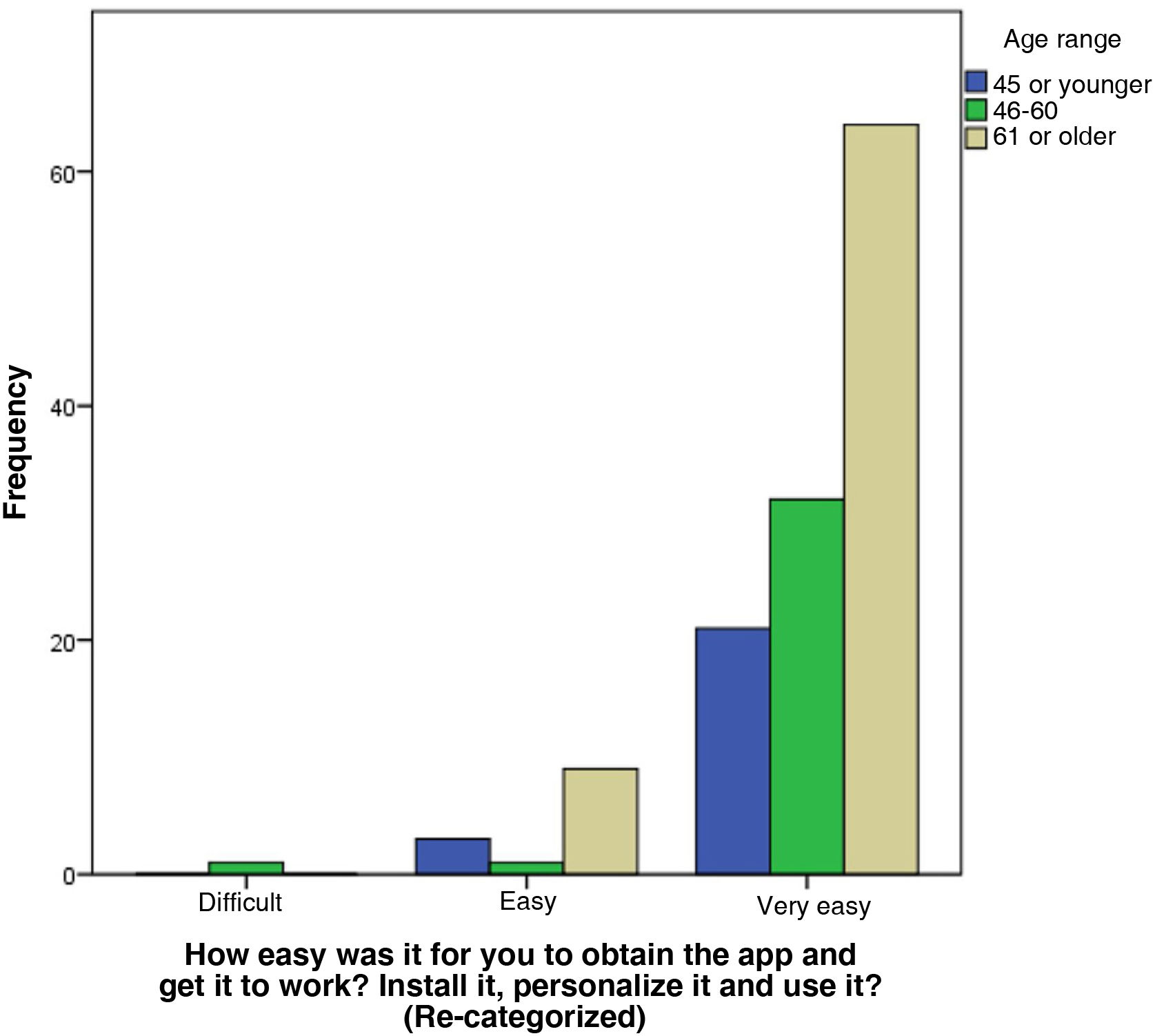
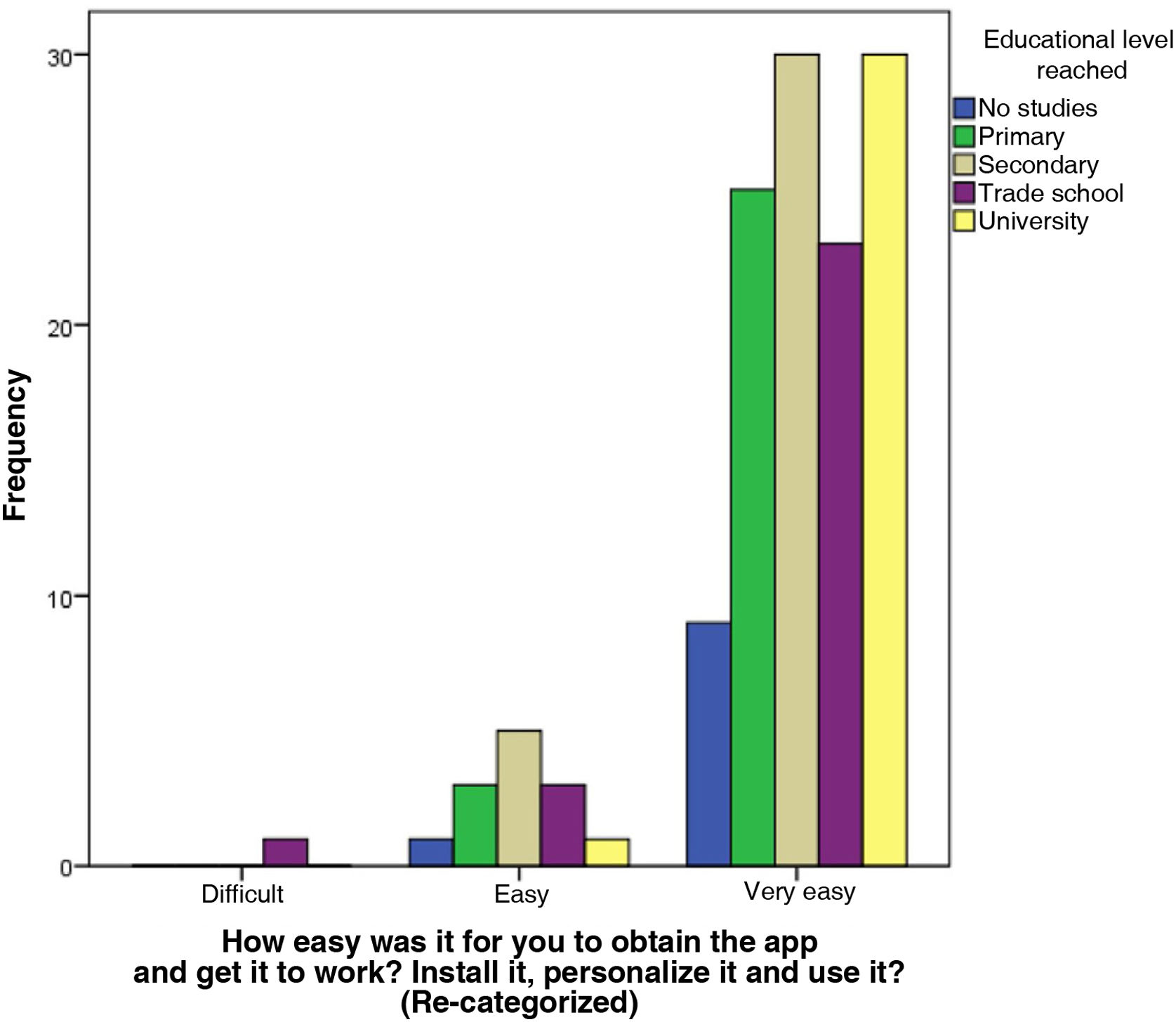
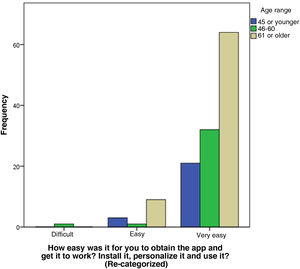
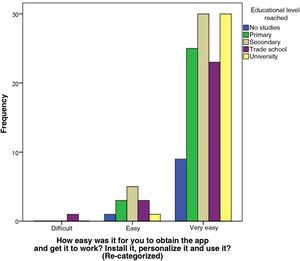
We performed a descriptive analysis of the categorical and quantitative variables associated with the demographic characteristics of the patients and the responses to the questionnaire. The ‘age’ variable was divided into 3 groups (18–45 years, 46–60 years, and ≥61 years) based on the age ranges established in other areas that study the use of computer tools11,12. In question 1, the 5 response options presented were modified into 3 categories (‘not at all easy’ or ‘somewhat easy’ into ‘difficult’; ‘moderately easy’ into ‘easy’; and ‘quite easy’ or ‘extremely easy’ into ‘very easy’) for correlations with other variables. Qualitative variables are presented with their distribution of frequencies and 95% confidence interval (95% CI). The quantitative variables are summarized as mean and standard deviation (SD) in case of presenting a normal distribution, and those that presented a non-normal distribution were represented with median and interquartile range (IQR). The association between qualitative variables was evaluated with the chi-squared test. In the statistical hypothesis testing, the null hypothesis was rejected with a type I error or α error less than 0.05.
ResultsA total of 131 patients were included in the study, most of whom were men (60.3%), with a median age of 62 years (51–71). Regarding their educational level, 35 patients (26.7%) had completed secondary education. Out of the 131 surgical interventions, 115 were lung resections, and 50.4% of the procedures were performed using a minimally invasive VATS approach (Table 2).
Demographics and surgical procedure variables.
| Variables | n = 131 |
|---|---|
| Sex | |
| Males | 79 (60.3%) |
| Females | 52 (39.7%) |
| Age range | |
| 18–45 years | 24 (18.3%) |
| 46–60 years | 34 (26%) |
| ≥61 years | 73 (55.7%) |
| Educational level | |
| No studies | 10 (7.6%) |
| Primary school | 28 (21.4%) |
| Secondary school | 35 (26.7%) |
| Trade school | 27 (20.6%) |
| University studies | 31 (23.7%) |
| Surgical procedure | |
| Lung resection surgery | 115 (87.8%) |
| Mediastinal tumor resection | 8 (6.1%) |
| Pleural biopsy | 4 (3.1%) |
| Drainage of pleural cavity | 2 (1.5%) |
| Rib resection | 2 (1.5%) |
| Surgical approach | |
| VATS | 68 (51.9%) |
| Conventional | 63 (48.1%) |
All of the included patients (100%) downloaded and used the app; 77 (58.8%) used it more than 4 weeks before surgery, with a median of 31 days (21–40). During the study period, no incidents were reported in the download, configuration, or use of the tool.
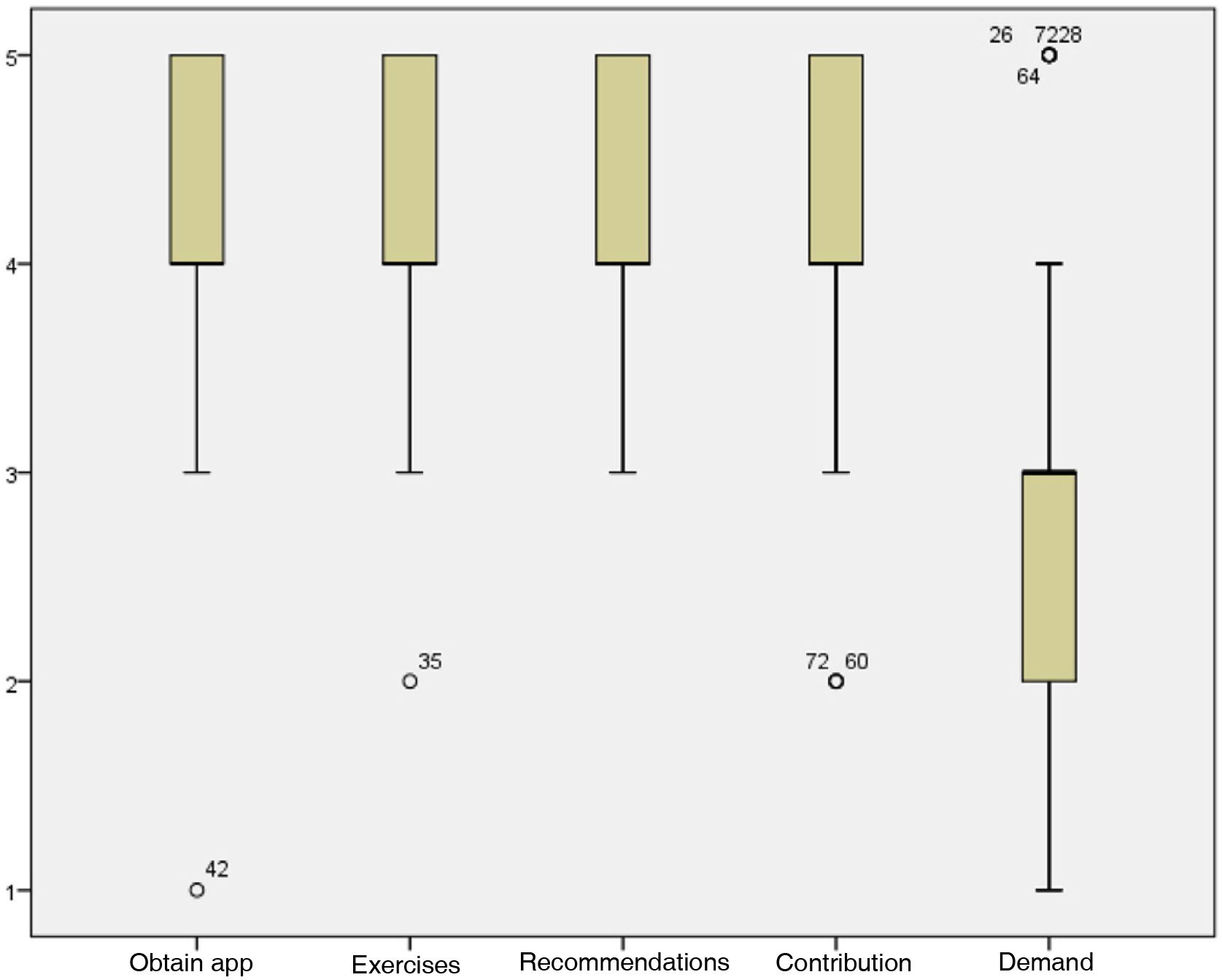
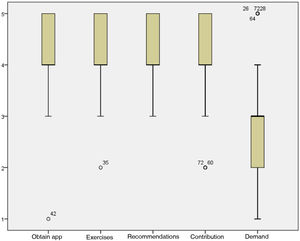
All patients answered the questionnaire. Fig. 3 shows the distribution of the responses obtained. A total of 117 (89.3%) patients rated positively the ease of downloading the app and starting it up; 123 (93.9%) rated positively the clear explanations of the respiratory therapy exercises, and 37 (28.2%) gave the maximum rating of ‘extremely clear’. Regarding the clarity of the general recommendations, 125 (95.4%) gave a positive rating. In terms of the subjective perception of the tool’s contribution towards preparing for surgery and coping with the postoperative period, 104 (79.4%) patients assessed it positively. Lastly, 73 (48.1%) patients rated the level of physical demand and the time of use necessary to meet the objectives set by the app as ‘adequate’.
In total, 117 patients found the app ‘very easy’ to obtain and configure. In this group, the majority (54.7%) were over 61 years of age, followed by 27.4% aged 46–60 years. These relationships were not statistically significant: chi-squared (4, N = 131) = 5.23, P = .23 (Fig. 4). Regarding the educational level attained, 25.6% of the patients who responded ‘very easy’ had university or secondary education, followed by those who had completed primary education (21.4%). These relationships were also not statistically significant: chi-squared (8, N = 131) = 6.28, P = .65 (Fig. 5).
A smartphone app was created with a perioperative care program, which was successfully implemented in a group of patients, regardless of their age or educational level. The tool clearly explains the information contained, and its use before surgery helps patients confront the postoperative period, with an adequate level of physical effort and time of use to meet the objectives set.
Perioperative care protocols are based on the application of a series of strategies that have proven to be effective in reducing the risk of developing postoperative complications1, shortening hospital stay4, reducing healthcare costs3, and improving the patient’s perception of the surgical process13. The objective is to implement them together to achieve a synergistic effect that has a positive impact on both the accelerated recovery of the patient and the restoration of their basal state5,14. The difficulty lies in uniting these different strategies from different specialties, which must be applied at different times of the perioperative period, into a single program that is easy to use, understandable, and encourages patients to complete it on as outpatients. The creation of a smartphone application turned out to be a valid option to overcome this challenge, allowing several strategies to be combined, while integrating a multidisciplinary perioperative care program into a single interactive tool that educates patients and prepares them for elective surgery.
Respiratory therapy exercises as part of perioperative physical exercise programs have been shown to reduce postoperative respiratory complications15–17. Some studies have reported a decrease in postoperative atelectasis, pneumonia, and length of hospital stay18,19. Others only improve aerobic capacity, physical condition and quality of life20–22. These differences are due to the fact that most studies have a limited number of patients and that there is a lack of homogeneity amongst respiratory physiotherapy programs or in the results measured6,23. With the app, a structured respiratory therapy exercise program was implemented, which includes: correct posture for performing the exercises, lung re-expansion maneuvers, techniques to mobilize secretions, expectoration techniques and aerobic exercise, with an established duration and number of repetitions. Thus, the tool can be used as an example to develop new research studies with a structured exercise program.
The app was created by a team of medical professionals based on information from scientific publications, including recommendations to modify patient behavior. In addition, as the software is used offline, no private health data are transmitted. All these characteristics resolve the limitations described with other health apps7, because although there is a boom in the creation of this type of projects, their regulation and control have not been fully implemented.24,25. The need to attend in-person classes at a hospital means that compliance with respiratory rehabilitation programs is not as expected26,27, but with the app we try to mitigate this problem. Personalized notifications appear 15 days before and after the date set on the patient’s device, with advice or positive reinforcement messages that encourage the patient to comply with the program while increasing the possibility of interaction with the tool. There are other similar initiatives, but these only contain physiotherapy exercises, are not marketed28, are not aimed at surgical patients29, or only focus on the preoperative phase30.
Evaluating the use of an app is essential for its correct implementation. Although there are validated instruments31, most studies do not publish these data32 or do not assess other factors, such as doctor-patient communication, the understandability of the information transmitted, or the patients’ opinions in terms of the actual benefit provided. Our data collection instrument assesses this information, and we also managed to demonstrate that age and educational level do not limit the implementation of new technologies in medicine. This is contrary to a previous report, where being under 45 years of age or having a high educational level were associated with better acceptance of a healthcare app12.
The main study limitation was the need to have a mobile device compatible with the application in order to participate. To overcome this limitation, we created a web version of the app with the same features and characteristics that could be accessed on a computer with Internet access. As for the study design, although it is descriptive, we developed it prospectively and included only thoracic surgery patients with homogenous patient preparation and postoperative management. In addition, the calculated sample size was met, and the sample of 131 patients is significantly larger than the samples of other publications33 and the samples contributed by each unit of a multicenter study34.
This study represents the first step in assessing the real value of applying the app in the healthcare setting. Patients are offered a tool to help them prepare for elective surgery that can be used without supervision, at any time, without the need to go to the hospital, and free of charge. For medical professionals, it is a complementary tool aimed at educating patients before surgery and a continuation of the postoperative care initiated in the hospital. Lastly, for the healthcare system, it does not represent any expense because it is a tool that has already been published. Our approach is to improve the performance of the tool and publish new research papers where the use of the app is able to establish causal relationships of its use with improved postoperative results.
ConclusionWe have developed a smartphone application with a perioperative care program that was successfully implemented in a group of patients undergoing elective surgery, regardless of their age or educational level. The tool clearly explains the information contained, and patients report that its use before surgery helps them cope with the postoperative period, with an adequate level of physical demand and time of usage.
FundingThis project has been partially financed by the Fundación Sociedad Española de Cirugía Torácica (SECT), awarded with a research project grant in the category of ‘Up-and-Coming Research Groups and/or Investigators’ in 2016.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors would like to thank Dr. Carlos Cerdán Santacruz for his collaboration in the revision of this article, Anna Strobl Bardo and Danny Mendonça Neto for the design of the graphic resources used, Leticia Fuentes Garrido for the design of the animations used, and Rafael Barriuso and Tribalyte Technologies for the programming of the application.