The discharge report is a basic document at the end of a care process, and is a key element in the coding process, since its correct wording, reliability and completeness are factors used to determine the hospital production.
Materials and methodsFrom a hypothesis based on the analysis of the consistency between the discharge report and data collected from the routine clinical notes during admission, we should be able to re-code all those mis-coded, thus placing them in a more appropriate diagnosis-related group (DRG). A total of 24 patient outliers were analysed for the correct filling in of the type and reason for admission, personal history, medication, anamnesis, primary and secondary diagnosis, surgical procedure, outcome, number of diagnostic and procedures cited, concordance between discharge report and history and recoding of the DRG.
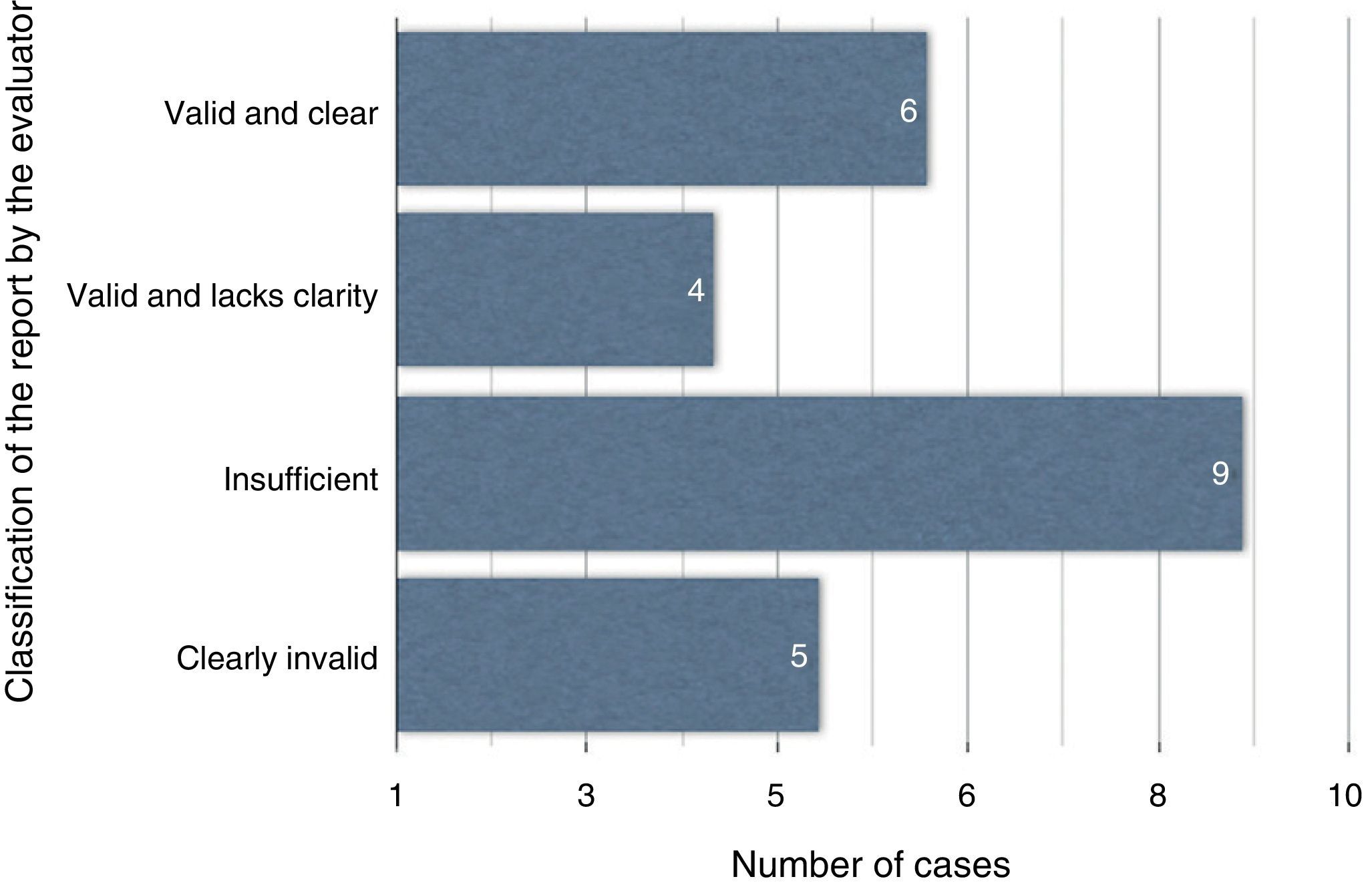
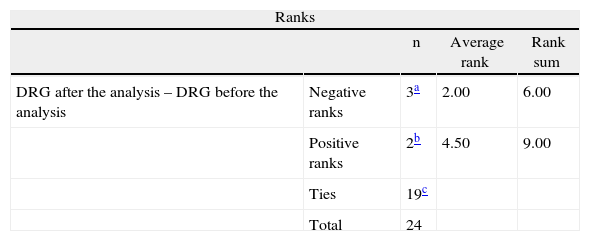
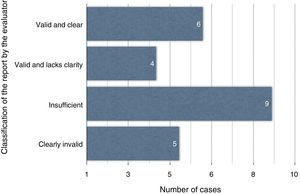
ResultsFrom a total of 24 episodes, 6 had precise and valid reports, 4 were valid but not precise enough, 9 were insufficient, and 5 were clearly invalid. The recoded DRG after the documentation review was not significantly different, according to the Wilcoxon test, being changed in only 5 cases (P=.680).
ConclusionQuality in discharge reports depends on an adequate minimum data set (MDS) in concordance with the source documentation during admission. Discordance can change the DRG, despite it not being significantly different in our series. Self-audit of discharge reports allows quality improvements to be developed along with a reduction in information mistakes.
El informe de alta es un documento básico al finalizar un proceso asistencial, y es un elemento clave en el proceso de codificación. De su correcta redacción, fiabilidad y exhaustividad dependerán los datos que sirvan para determinar la producción hospitalaria.
Material y métodosPartimos de la hipótesis de que, analizando la concordancia del informe de alta con los datos cotejados en la documentación del episodio, podremos recodificar todos aquellos casos infracodificados, imputándolos así a un grupo relacionado por el diagnóstico (GRD) más adecuado. Analizamos en 24 pacientes outliers la correcta cumplimentación de tipo y motivo de ingreso, antecedentes personales y medicación, resumen del episodio, diagnósticos principal y secundarios, procedimiento quirúrgico, evolución durante el episodio y número de diagnósticos y procedimientos enumerados, concordancia con la información real del episodio y los cambios teóricos entre los GRD antes y después del análisis.
ResultadosDe 24 casos, 6 informes son válidos y claros; 4, válidos aunque poco claros; 9 son insuficientes y 5, claramente inválidos. La comparación de los GRD recalculados tras la interpretación de los datos del episodio no muestra diferencias significativas, mediante test de Wilcoxon, encontrándose tan solo modificaciones en 5 casos (p = 0,680).
ConclusionesLa calidad del informe de alta depende de la correcta inclusión de todos los datos del CMBD, en concordancia con el episodio. Las discordancias historia/informe pueden modificar el GRD que, en nuestra serie, no es estadísticamente significativo. La autoauditoría del informe de alta hospitalaria permite establecer líneas de mejora, al disminuir los errores de información.
The hospital discharge report1,2 (HDR) is a basic document of a patient's clinical history. It is issued by the physician in charge at the end of the care process in a hospital. In this document, a summary of the medical history, the care provided, the main diagnosis, secondary diagnoses and recommended treatment is provided. The HDR contains essential information that improves the interoperability among heterogeneous systems; it is an excellent communication tool between the clinician who writes it and a variety of users, such as the patient and his/her relatives, the primary care physician, members of the same service as the physician who wrote the report, other specialists, the emergency medical service, clinical coders, nurses, social workers, researchers, care activity evaluators and health and law authorities.3
The HDR contains essential information that facilitates the continuity of care from a hospital setting to an outpatient setting. It improves efficiency, reduces the amount of time spent seeking information, avoids repeated diagnostic tests and reduces medication errors. It is a key element in the coding process because relevant data that determine hospital productivity depend on the correct drafting, reliability and exhaustiveness of the HDR.4 It enables administrators and doctors to know the main indicators of hospital production.
The quality of the information contained in an HDR has been the subject of few publications, most of which have focused on internal medicine services. For this reason, we consider the study of HDR quality in surgical services of great interest.
The main objectives were first, to search for a line of improvement in the quality of the discharge reports and second, to assess the impact that a low-quality report has on coding. The main hypothesis of the study is that a considerable percentage of cases that are considered outliers (extremely atypical) would not be if they were correctly coded at discharge. Therefore, correct coding and the reconsideration of outlier conditions would reclassify these cases into an adequate diagnosis-related group (DRG), where mean stays would be compared to a more appropriate standard.
Materials and MethodsWe performed a consistency analysis between the electronically archived HDR and the paper copy of the medical history, which was requested specifically from the hospital archive for this study, to assess all the outliers that were reported by the documentation service for a period of one trimester in the General and Digestive Tract Surgery Service of the Virgen Macarena University Hospital and Area (currently the management unit). The cases that were considered outliers were those with a hospital stay over the 90th percentile out of the 713 codified discharges (3.36% of outlier cases) calculated according to the multihospital standard for its corresponding DRG.
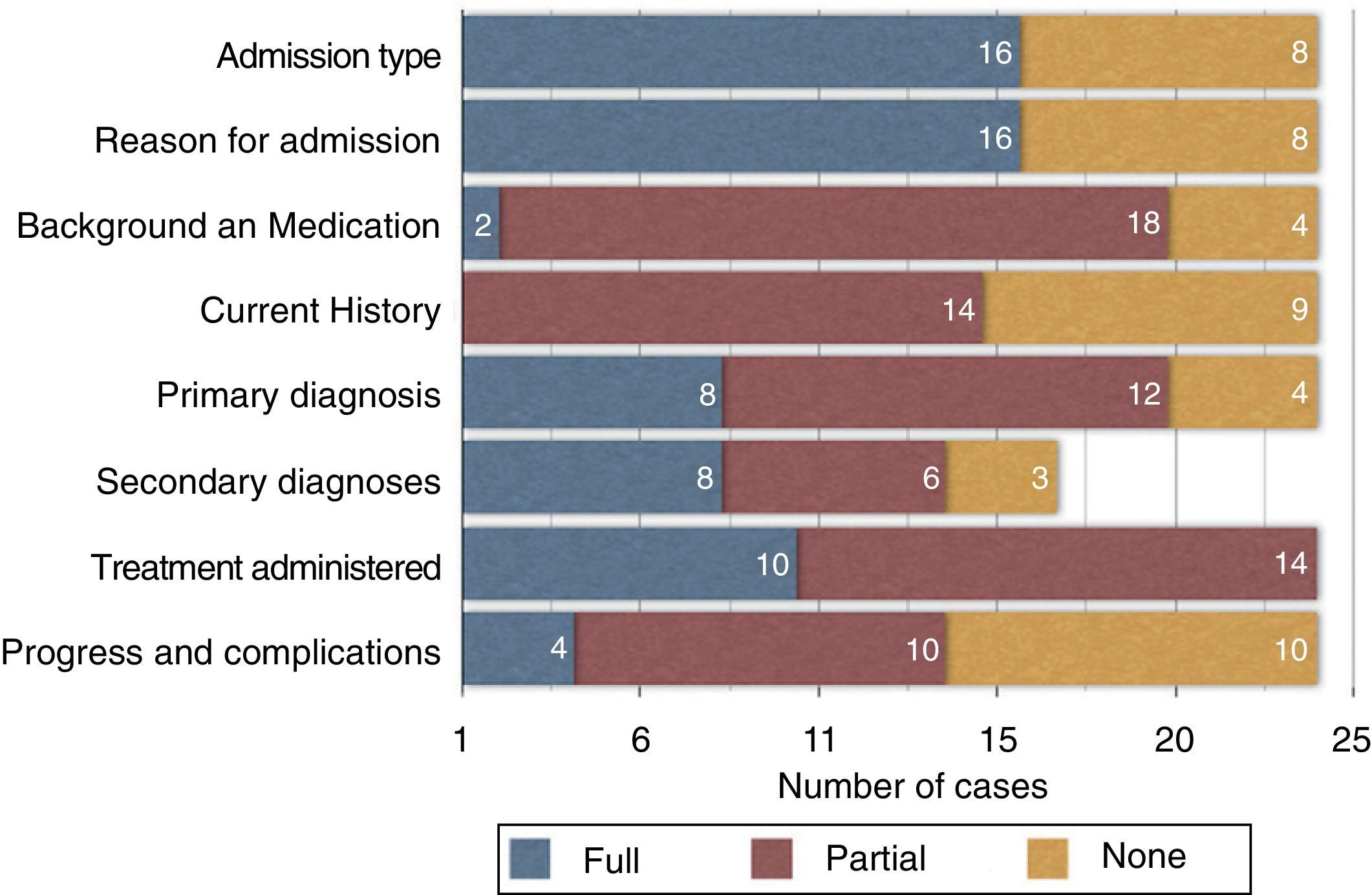
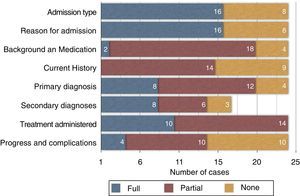
The correct completion of the following items was evaluated as an indicator of quality of the information on the reports: type of admission, reason for admission, personal and medication history, episode summary, main and secondary diagnoses, surgical procedure, evolution of the episode and number of outlined diagnoses and procedures.
In addition, the opinion of the evaluator and the report-history discrepancies was analysed, as were the theoretical changes in the DRG before and after the analysis.
The evaluator's opinion was based on the following criteria:
- -
Valid and clear report: The report is well structured, with independent sections; after reading it, the independent evaluator obtained the same conclusions that they did when reading the complete documentation of the episode.
- -
Valid, unclear report: Despite a poor structure and form defects, the report generates the same conclusions that were drawn from the complete documentation of the episode.
- -
Insufficient report: When, for whatever reason, the conclusions that the evaluator obtains from the report, though not very different from those obtained when analysing the episode in its totality, can modify the report's coding and thus the DRG.
- -
Clearly invalid report: The report does not comply with the minimum quality criteria for a basic minimum data set (BMDS). Additionally, the examiner's conclusions drawn from the report are different from those that were obtained after the complete documentation was read and resulted in a change in the DRG.
A 95% statistical significance level was established. The chi-square test was used for qualitative variables, and the non-parametrical rank test (Wilcoxon test) was used to examine 2 related values when comparing the consistency between the number of diagnoses and procedures before and after the complete documentation of the episode was analysed. The consistency of the DRG was studied using the McNemar non-parametric test.
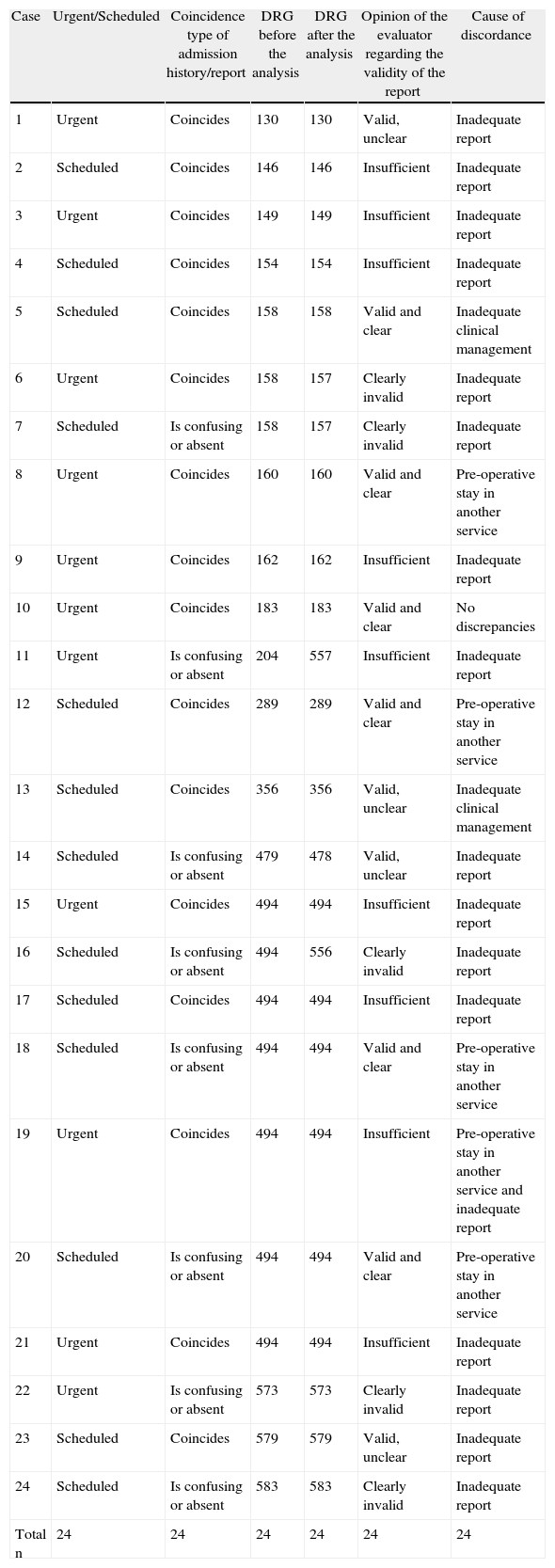
ResultsAs Table 1 shows, we included a total of 24 cases, 13 scheduled admissions and 11 urgent admissions. The data from the discharge report and from the episode were consistent for 9 urgent cases and 7 scheduled cases; for 2 urgent cases and 6 scheduled cases, the data were not specified, or may lead to confusion, showing a non-significant difference (P=.148). The cause of hospitalisation was consistent in 72% of the urgent cases compared with 61% of the scheduled cases, a value that also had no statistical significance (P=.562).
Detailed Summary of the Cases.
| Case | Urgent/Scheduled | Coincidence type of admission history/report | DRG before the analysis | DRG after the analysis | Opinion of the evaluator regarding the validity of the report | Cause of discordance |
| 1 | Urgent | Coincides | 130 | 130 | Valid, unclear | Inadequate report |
| 2 | Scheduled | Coincides | 146 | 146 | Insufficient | Inadequate report |
| 3 | Urgent | Coincides | 149 | 149 | Insufficient | Inadequate report |
| 4 | Scheduled | Coincides | 154 | 154 | Insufficient | Inadequate report |
| 5 | Scheduled | Coincides | 158 | 158 | Valid and clear | Inadequate clinical management |
| 6 | Urgent | Coincides | 158 | 157 | Clearly invalid | Inadequate report |
| 7 | Scheduled | Is confusing or absent | 158 | 157 | Clearly invalid | Inadequate report |
| 8 | Urgent | Coincides | 160 | 160 | Valid and clear | Pre-operative stay in another service |
| 9 | Urgent | Coincides | 162 | 162 | Insufficient | Inadequate report |
| 10 | Urgent | Coincides | 183 | 183 | Valid and clear | No discrepancies |
| 11 | Urgent | Is confusing or absent | 204 | 557 | Insufficient | Inadequate report |
| 12 | Scheduled | Coincides | 289 | 289 | Valid and clear | Pre-operative stay in another service |
| 13 | Scheduled | Coincides | 356 | 356 | Valid, unclear | Inadequate clinical management |
| 14 | Scheduled | Is confusing or absent | 479 | 478 | Valid, unclear | Inadequate report |
| 15 | Urgent | Coincides | 494 | 494 | Insufficient | Inadequate report |
| 16 | Scheduled | Is confusing or absent | 494 | 556 | Clearly invalid | Inadequate report |
| 17 | Scheduled | Coincides | 494 | 494 | Insufficient | Inadequate report |
| 18 | Scheduled | Is confusing or absent | 494 | 494 | Valid and clear | Pre-operative stay in another service |
| 19 | Urgent | Coincides | 494 | 494 | Insufficient | Pre-operative stay in another service and inadequate report |
| 20 | Scheduled | Is confusing or absent | 494 | 494 | Valid and clear | Pre-operative stay in another service |
| 21 | Urgent | Coincides | 494 | 494 | Insufficient | Inadequate report |
| 22 | Urgent | Is confusing or absent | 573 | 573 | Clearly invalid | Inadequate report |
| 23 | Scheduled | Coincides | 579 | 579 | Valid, unclear | Inadequate report |
| 24 | Scheduled | Is confusing or absent | 583 | 583 | Clearly invalid | Inadequate report |
| Total n | 24 | 24 | 24 | 24 | 24 | 24 |
The patient's medical background and previous medications were not described in 4 cases and coincided for only 2 patients. The remaining 18 cases coincided to a greater or lesser extent. Regarding the consistency between the description in the registered medical history in the report (interview and episode exploration) compared with the description obtained from all of the episode's documentation, we identified only one case in which the descriptions matched and 9 cases in which the description was insufficient or absent. The main diagnosis was not listed in 4 cases, while secondary diagnoses were omitted in 8; however, there was a greater consistency for the main diagnosis (8 cases) than for the secondary diagnoses (3 cases). The main surgical procedure was described in 9 cases as it was stated on the surgical sheet, while the surgical descriptions were discordant in 14 cases (one patient's surgery was not performed as described on the discharge report). The clinical course, including complications, was not specified in 10 out of the 24 cases, and coincided completely in 4 cases. There was no significant difference between the urgent and scheduled admissions on the above-mentioned items. When we compared the number of diagnoses and procedures collected on the discharge report with those gathered from the history, we found significant differences in the diagnoses (P=.004) but not in the procedures; the procedure descriptions coincided in 17 cases (P=.380). However, 16 patients had fewer diagnoses reported (mean=2.25) in the discharge reports than in the complete report of the episode (mean=3.92).
The consistency between the discharge report and the documents of the episode for all analysed items can be assessed in Fig. 1, where each percentage distribution is shown graphically.
The evaluator considered 6 reports valid and clear, 4 reports valid but unclear, 9 reports insufficient and 5 clearly invalid (Fig. 2). The comparison of the recalculated DRG after the interpretation of the episode's data showed no significant differences using the Wilcoxon test, with modifications observed in only 5 cases (P=.680; Table 2).
DiscussionIn an environment where clinical management, evaluation of results and efficiency analysis are conducted, it is important to consider the development of improvement lines, many of which are based on self-assessment and aim towards greater efficacy and efficiency. The design of self-auditing programmes or internal auditing in management units is an effort towards improvement and thus an increase in quality.
Currently, technical solutions make interoperability between heterogeneous information systems possible. One of the essential steps required to achieve this is to agree on the relevant data that must be included in the different clinical reports of the health processes performed on specific individuals in any centre or service of the National Health System. This homogeneity is one of the standardisation elements that improve the different systems’ exchange of information, to the benefit of the citizens.5
In our country, since 1984, a hospital discharge clinical report has been required by law for all patients seen in a health care facility. The minimum content of the discharge report is regulated by several national and other regional legal norms, such as Law 41/2002 of 14 November 2002 regarding the autonomy of patients and their rights and obligations regarding clinical information and documentation. Article 15 of this law regulates the minimum content of each patient's clinical record. In their exercise of health management competence, autonomous regions have been implementing different medical history/health record models and solutions for internal use in their centres and services. In recent years, those models have replaced the traditional paper format with a digital or electronic format. The current degree of electronic medical history implementation in the centres and services of the National Health System almost reaches full implementation in all Primary Healthcare Facilities. It is foreseeable that soon, a similar level of implementation in Specialised Care and Medical Emergency Centres will be reached.5 Other regulations include Organic Law 15/1999 of 13 December on the Protection of Personal Data, General Health Law 14/1986 and the Ministerial Order of 6 September 1984, which regulates the discharge report.6
Patients have the right to receive an HDR, and the attending physician is obligated to provide one. The HDR includes special protection data that limit its access and use. The report includes a series of minimum requisites that constitute the BMDS. This database shows the complexity of the medical care process that should be summarised in the HDR and indicates the comprehensive code sequencing used by a clinical coder who develops patient classification systems using computer programmes. At present, the most widely used system is the DRG, which classifies the groups according to diagnosis and allows cost analyses and comparisons of the hospital product among centres to evaluate centres’ efficacy and add consistency criteria related to different aspects. The quality and exhaustiveness of clinical coding are closely related to HDR quality. This report should contain the main and secondary diagnoses; co-morbidities; clinical evolution, including complications during the stay; and the performed procedures. The main indicators of hospitalisation management will be generated from this information. The BMDS is not just an administrative database that generates health management information; it is also a useful research project design tool for clinicians.7
However, as described in the study by Reyes et al.,8 only 2.8% of HDRs contain adequate information; there is an important variation in terms of the completion of the analysed data, reflecting significant completion differences among hospitals and patients and often providing more information for younger men with fewer co-morbidities.
Another issue to consider is report recovery and the consistency of the details about the episode, which could be improved through systematic report elaboration that gives the patient access to information more quickly and precisely.9
Thus, this study has been framed with the aim to work towards establishing efficiency. It is clearly stated in the literature7 that the HDR is very useful for patients, relatives or caregivers because it allows them to be informed about the patient's health status. It also aids the development of the outlined treatment plan and serves as a basic information and communication element among the different healthcare levels. Furthermore, the clinical coder transfers the diagnoses, diagnostic tests and surgical interventions from the medical history to codes from the International Classification of Diseases (ICD-9-CM). This allows for the proper statistical handling of the information that we as physicians provide via an adequate description of all of the details of the hospitalisation through our hospital discharge report. Training on how to elaborate an HDR during the training period must be better structured and supervised because the ability to write an accurate HDR is acquired in the physician's first years in the speciality.
It is essential for the HDR to be clear and concise, avoid ambiguous terms and ensure that all of the BMDS variables are completed and admission complications and treatment process are included. In light of coding services’ work overload, it seems commonly acceptable to code on the basis of the HDR rather than the complete medical history, as theoretically required. However, a poorly elaborated HDR would lead to insufficient coding, which would result in an inadequate DRG and thus an incorrect calculation of its complexity. Although our series found no significant differences in case recoding, it seems clear that discharge report errors, mainly in terms of data omission, would cause DRG modifications that, despite the lack of statistical significance, could result in a calculation of complexity in more extended series that is more consistent with the reality of this study.
The decision to perform an analysis mainly on outlier cases, which is justified by the initial hypothesis, should not be a bias factor precisely for this reason. The extension of the analysis to a significant sample of the total codified discharges for the analysis could offer broader information about the actual activity in the unit. In any case, the final decision has also been to select these cases because the fact that they are extreme cases means that the differences resulting from improvements would most likely be more evident and have a greater impact.
ConclusionThe quality of the hospital discharge report depends mainly on the correct inclusion of all the BMDS data consistent with the history of the episode.
History/report discrepancies may generate a modification of the DRG classification that could increase its complexity and better match the results to reality, although our study's findings were not statistically significant.
As a form of self-auditing, the critical analysis of the hospital discharge report in the surgical units allows the improvement of quality lines, with an increase in patient and a reduction in information errors.
Conflict of InterestsThe authors declare no conflict of interests.
María Sanchez-Ramirez worked in the General and Digestive Tract Surgery Clinical Management Unit, Virgen Macarena University Hospital, Seville when this manuscript was written.
Please cite this article as: Gomez-Rosado JC, Sanchez-Ramirez M, Valdes-Hernandez J, Capitan-Morales LC, del-Nozal-Nalda MI, Oliva-Mompean F. Importancia de la calidad del informe de alta en la gestión de una unidad clínica quirúrgica. Cir Esp. 2013;91:378–383.