Adhesions are the most important cause of intestinal obstruction. Approximately 25% of surgical admissions for acute abdominal conditions are due to intestinal obstruction. Better diagnostic and treatment methods of intestinal obstruction could potentially reduce mortality rate to 5%–10%. Gastrografin® could contribute to this achieve this.
AimTo present a protocol to treat adhesion intestinal obstruction with Gastrografin® that is safe, and allows shorter hospital stays and shorter time between admission and surgery.
Material and methodsAll patients with adhesion intestinal obstruction without symptoms of strangulation were treated with Gastrografin®, intravenous fluids and nasogastric tube. Those in whom contrast reach the colon in 8, 12 or 24h were considered to have partial obstruction, and were fed orally. If Gastrografin® failed in the following 24h, a laparotomy was performed.
ResultsOut of a total of 211 episodes (164 patients), 170 episodes received contrast and in 142 cases Gastrografin® reached the colon (104 episodes at 8h, 11 at 12h, and 27 at 24h). A laparotomy was required in 28 patients because of failed treatment, and in another 5 for other causes.
ConclusionsA management protocol for adhesion intestinal obstruction with Gastrografin® is safe, reduces morbidity and mortality, and leads to a shorter hospital stay.
Las adherencias son la causa más importante de oclusión intestinal, suponen un 25% de las consultas por dolor abdominal. Con un correcto manejo de este cuadro, la mortalidad asociada puede ser menor de un 5–10%. El Gastrografin® puede ayudar a ello.
ObjetivoLa aplicación de un protocolo de manejo de la oclusión intestinal adherencial con Gastrografin® es segura y permite disminuir la estancia hospitalaria y el tiempo de indicación de cirugía por fallo del tratamiento conservador.
Material y métodoEstudio prospectivo observacional, siguiendo un protocolo preestablecido. Una vez diagnosticado el cuadro, descartadas otras causas de oclusión y la presencia de sufrimiento intestinal, se administra Gastrografin® y se inicia tratamiento conservador. Si el Gastrografin® pasa al colon en el control de las 8, 12 o 24h posteriores a su administración, se considera la oclusión como parcial, se inicia dieta oral y se evalúa el alta. Si no pasa el contraste a las 24 h, se indica cirugía.
ResultadosDesde enero de 2009 hasta diciembre de 2011, se trataron 211 episodios (164 pacientes). En 170 episodios se administró contraste con llegada del mismo al colon en 142 episodios (104 episodios a las 8h, 11 a las 12h y 27 a las 24h) Se intervien a 28 pacientes por fallo del tratamiento conservador y a 5 por otras causas.
ConclusionesLa aplicación de un protocolo en el que se incluye el uso de Gastrografin® en la oclusión intestinal adherencial es seguro y permite tomar decisiones terapéuticas con mayor celeridad y con una menor estancia hospitalaria.
Intestinal obstruction is a frequently seen entity in the Emergency Department that represents 25% of abdominal pain consultations.1 The most frequent causes of intestinal obstruction are postoperative adhesions followed by neoplasms and hernias.2 The estimated rate of adhesions is around 94%–95% after laparotomy. It has recently been demonstrated that this rate is much lower in laparoscopic procedures, although the exact percentage is not known.3 Before the 1990s, the mortality rate associated with intestinal obstruction was 30%–50%, depending on the series.4 Nowadays, the correct diagnosis of symptoms and adequate treatment can lower the mortality rate to 3%–5%.4–6
During the management of intestinal obstruction, the patient should initially be made to fast and intravenous therapy should be administered, in addition to intestinal decompression with a nasogastric tube. Most of the symptoms will respond to conservative treatment. The indication for surgery is clear when there are data to suspect ischemia or intestinal suffering: fever, tachycardia, abdominal pain, peritonitis and acidosis. The problem lies in knowing how much time should pass before we decide whether the patient is responding to conservative treatment and, therefore, when surgery should be indicated.
There have been several attempts at trying to improve the management of this entity: one of the most well-known has been the administration of water-soluble contrast.7 The use of these contrasts gives a more precise diagnosis of the partial or complete obstruction4 according to whether the contrast passes into the colon and, therefore, facilitates the decision for surgery in those obstructions that do not improve with medical treatment.8 The therapeutic effect of these water-soluble contrasts is not clear, although some studies say they can demonstrate it when the contrasts are administered more than 24h after the conservative treatment.9 Based on these studies, our department has used an algorithm for cases of adhesive intestinal obstruction (AIO) in order to demonstrate that it provides safe management of the symptoms, is able to improve surgical indication time and also improves hospitalization times, without increasing adverse effects.
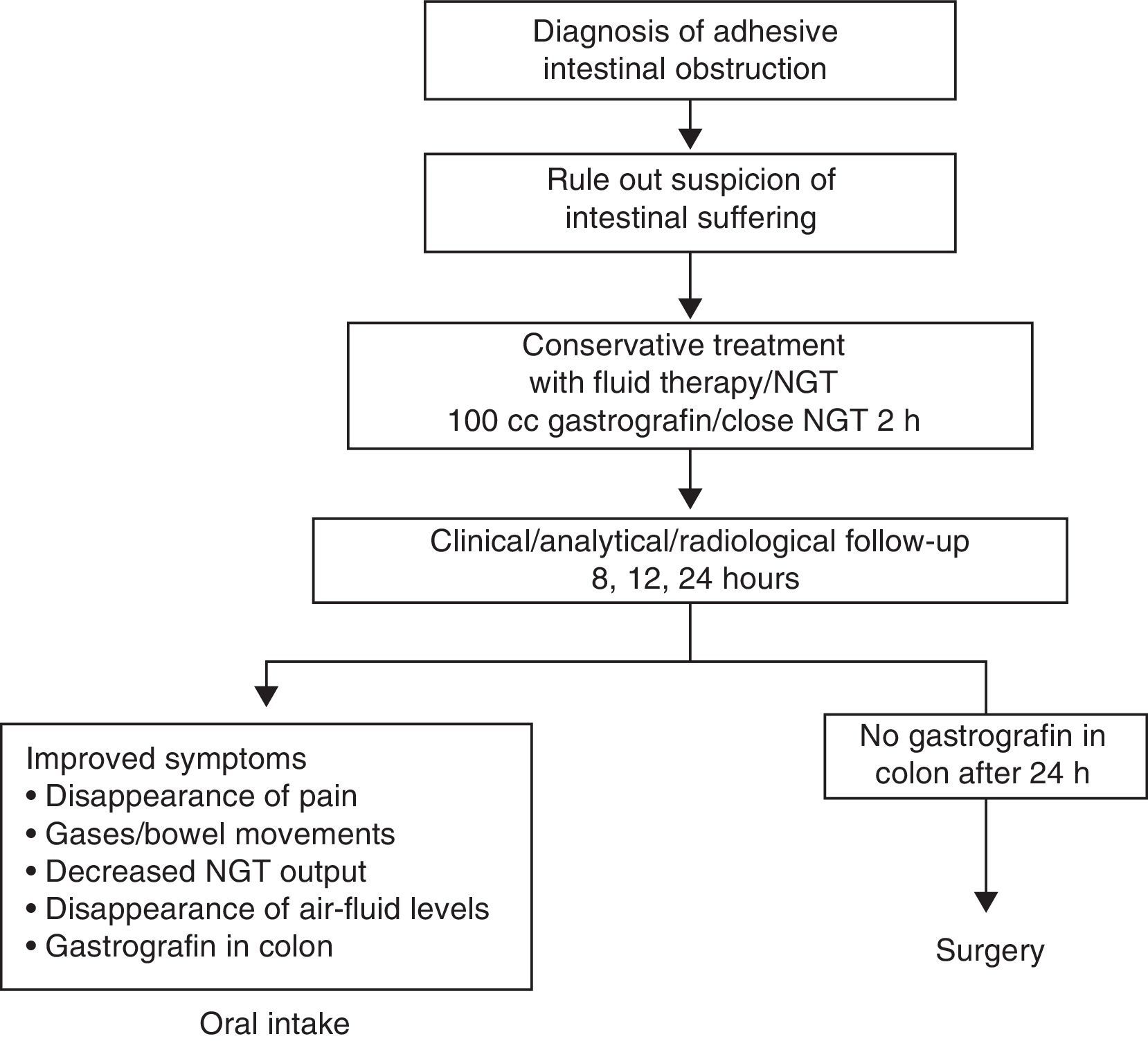
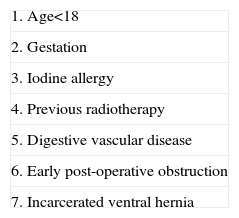
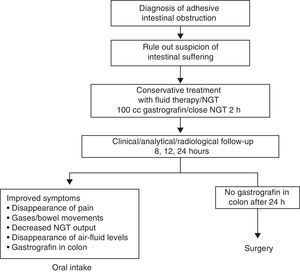
Material and MethodsThis descriptive, prospective and observational study was carried out from January 2009 to December 2011. Following the protocol described in Fig. 1 at our hospital, when a patient presents with clinical symptoms compatible with intestinal obstruction (Fig. 2) and has a history of surgery, the first suspected diagnosis is AIO. All patients undergo detailed abdominal examination in order to rule out the presence of other causes for the obstruction. Afterwards, an abdominal radiograph is ordered along with analyses including blood work-up, biochemistry and acid-base balance. If the patient fulfills the inclusion criteria (symptoms and radiology compatible with obstruction and history of abdominal surgery with an interval of more than one month), he/she is included in the AIO protocol. If, contrarily, the patient presents exclusion criteria (Table 1), he/she is not included in the protocol and management is determined by the characteristics of each case.
In cases of AIO, the water-soluble contrast Gastrografin® was administered in our center. Prior to the administration of Gastrografin®, gastric decompression was performed with the placement of a nasogastric tube for approximately 2h in order to reduce the risk of vomiting and aspiration after the administration of the contrast. At the follow-up controls (at 8, 12, 24h), oral intake was initiated when the patient presented passage of the contrast material to the colon (Fig. 3), regardless of the time of the control.
The variables that were collected and analyzed were: age, sex, types and number of previous surgical interventions, need for surgery, need for intestinal resection during the episode and hospital stay.
For the statistical analysis, we used the SPSS 17.0 program. The quantitative variables are reported by means and standard deviation or median and range when the distribution was not normal. The categorical variables are described in absolute numbers and percentages.
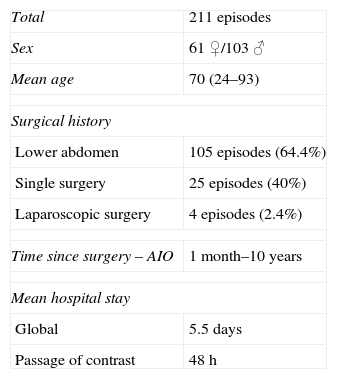
ResultsDuring the study period, 211 episodes of AIO were diagnosed in our hospital in 164 patients: 61 ♀ and 103 ♂, with a mean age of 70 (range 24–93).
As recorded in the medical files of the 164 patients, 105 (64.6%) had undergone lower abdominal surgery, 25 (40%) had a single previous surgery and only 4 patients out of the 164 (2.4%) had had prior laparoscopic surgery (Table 2).
Patient Characteristics.
| Total | 211 episodes |
| Sex | 61 ♀/103 ♂ |
| Mean age | 70 (24–93) |
| Surgical history | |
| Lower abdomen | 105 episodes (64.4%) |
| Single surgery | 25 episodes (40%) |
| Laparoscopic surgery | 4 episodes (2.4%) |
| Time since surgery – AIO | 1 month–10 years |
| Mean hospital stay | |
| Global | 5.5 days |
| Passage of contrast | 48h |
The time between the surgery and the episode of intestinal obstruction was very variable, ranging from 1 month to 10 years with a mean of 55 months.
Mean hospital stay was 5.5 days, and 48h in those patients in whom the contrast passed into the colon.
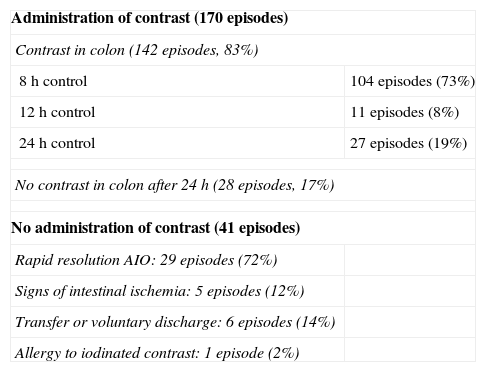
Contrast material was administered in 170 of the cases diagnosed. In the 41 episodes when contrast was not used, the causes were: rapid resolution of the symptoms in 29 episodes (72%), deterioration of the patient with signs of intestinal ischemia in 5 episodes (12%), transfer of the patient or voluntary hospital discharge in 6 cases (14%) and contrast allergy in one patient (2%). No adverse effects were observed related to the administration of the contrast.
In the 170 episodes in which contrast was administered, it passed to the colon in 142 (83%). The contrast was observed in the colon after 8h in 104 episodes out of the 142 (73%), after 12h in 11 episodes (8%) and after 24h in 27 episodes (19%). In 28 episodes out of the 170 (17%), the contrast had not passed into the colon after 24h and the patients presented no improvement in their symptoms, requiring surgery (Table 3).
Results of Application of the AIO Protocol.
| Administration of contrast (170 episodes) | |
| Contrast in colon (142 episodes, 83%) | |
| 8h control | 104 episodes (73%) |
| 12h control | 11 episodes (8%) |
| 24h control | 27 episodes (19%) |
| No contrast in colon after 24 h (28 episodes, 17%) | |
| No administration of contrast (41 episodes) | |
| Rapid resolution AIO: 29 episodes (72%) | |
| Signs of intestinal ischemia: 5 episodes (12%) | |
| Transfer or voluntary discharge: 6 episodes (14%) | |
| Allergy to iodinated contrast: 1 episode (2%) | |
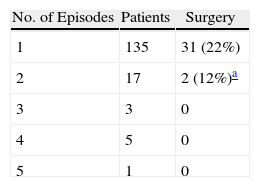
Table 4 reports the recurrence of the obstructive symptoms in our group.
Recurrences.
| No. of Episodes | Patients | Surgery |
| 1 | 135 | 31 (22%) |
| 2 | 17 | 2 (12%)a |
| 3 | 3 | 0 |
| 4 | 5 | 0 |
| 5 | 1 | 0 |
All patients were treated according to the AIO protocol.
Thirty-three patients required surgery: 28 cases due to failure of the conservative treatment and 5 cases in which, upon hospitalization or during their stay in the ER, the patients presented clinical or analytical signs of intestinal ischemia. Surgical findings included the presence of a solitary adhesion/band in 16 episodes out of 33 (48%) and multiple adhesions in 17 episodes (52%). Intestinal resection was only needed in 5 patients out of the 33 (3%).
DiscussionWe know that AIO is a frequent pathology seen in the Emergency Department. It presents an important mortality rate that can be reduced to 3%–5% with proper management of symptoms.4–6 It initially requires a conservative management with fluid therapy, fasting and decompression. More than 70% of cases will have a good response to this initial conservative management.10–12
When we observe the results obtained with the application of the protocol, we can confirm that our results corroborate the results of studies that administer water-soluble contrast medium after the diagnosis of AIO. The most important studies on the application of water-soluble media in intestinal obstruction due to bands and adhesions were initiated in the 1990s, and studies still continue today.13 They all try to demonstrate the diagnostic utility of contrasts and also their therapeutic utility. As for the diagnostic utility of these contrast materials, the studies all concur that they are able to determine the type of obstruction (either partial or complete) with a high sensitivity, specificity and positive and negative predictive value (87.5, 100, 100 and 97.9%, respectively).14 This high diagnostic precision enables physicians to improve the management of AIO from its initial diagnosis.
In these studies, there are differences with regard to radiological control times after the administration of the contrast. Some studies indicate surgery in the first radiological control after 4h.15 This seems an aggressive measure, however, especially when studies with a longer waiting period,16–19 like our study, have observed that most patients (104 patients out of 142 [73%]) who present partial obstruction respond within the first 8h. But there is a percentage, 28 episodes out of 142 (17%), that may respond within the first 24h and, therefore, surgery may be avoided in these cases. It is not recommended to lengthen the control times for longer than 24h because this has not been shown to improve the results and may increase patient morbidity and mortality.16
The diagnostic effect is able to streamline the treatment of partial obstructions, which shortens the hospital stays of patients, as observed in our case and in reports by other groups.20,21 Furthermore, the adverse effects related with hospital stay are also minimized. With regard to complete obstruction, the use of these contrasts is able to shorten the time between the hospitalization of the patient until the indication of surgery.22 Until now, contrast material has not been shown to have a therapeutic effect (meaning that they reduce the number of episodes requiring surgery), although in some studies it seems to do so.9,23 What we can affirm is that, although the reduction in the number of surgeries in this pathology is not clear, we do see a reduction in the number of patients requiring intestinal resection. Only 5 out of the 33 surgical patients (3%) required intestinal resection. This may be related to the rapid indication of surgery when conservative treatment fails. In our study, the patients who required surgery presented solitary as well as multiple bands with similar percentages.
Until now, we have not seen any adverse effects related with the administration of contrast material in our patients. Allergic reactions and aspiration pneumonitis have been reported24 related with the use of orally administered water-soluble contrast media. Of all the studies reviewed, there was only one report of an allergic reaction.25 We can therefore confirm that the administration of water-soluble contrast material in the management of AIO is safe.26
In conclusion, the protocol that we apply in our hospital is a safe protocol that provides proper management of AIO. In cases of partial obstruction, it reduces hospital stays and, in cases of total obstruction, it shortens the time before the indication of surgery. This leads to a lower percentage of intestinal resection in cases requiring surgery.
Conflict of InterestThe authors declare that they have no conflicts of interest.
We would like to thank all the members of the General Surgery Department, and especially the on-call teams, for their collaboration in carrying out this protocol. Thanks also to the Diagnostic Radiology Department for their participation in the radiological controls of these patients.
Please cite this article as: Mora López L, Serra-Aracil X, Llaquet Bayo H, Navarro Soto S. El uso de Gastrografin® en el manejo del cuadro de oclusión intestinal adherencial. Cir Esp. 2013;91:384–388.