Bronchial adenoid cystic carcinoma (ACC) is a rare infiltrative neoplasm that has a tendency for local recurrence and the ability to metastasis. Surgery is usually the best therapeutic option and there may be an indication for adjuvant radiotherapy, as in the cases that we present below.
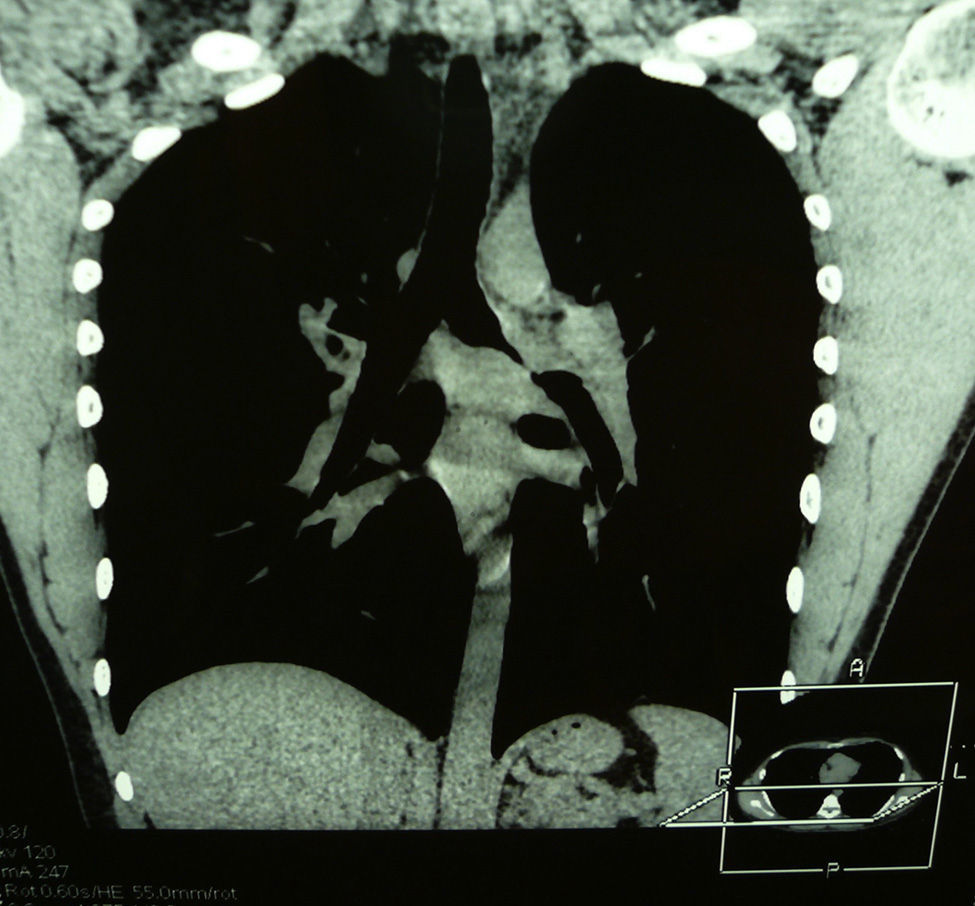
Case 1A 19-year-old male with a history of pneumonia in the left lung and, since then, dyspnoea and bronchial hyperreactivity, which led to the diagnosis of asthma. Computed tomography (done after the appearance of pleuritic pain) identified a well-defined mass in the left pulmonary hilum (35mm×23mm×30mm), that encompassed the main bronchus (Fig. 1). Bronchoscopy showed a near total obstruction of the primary bronchus by a mammillated mass that extended 3–4cm into the lumen and reached the carina. Bronchial biopsy determined it was an ACC.
Surgical treatment involved initial bronchotomy in the carina; tumour infiltration was thus confirmed in both lobar bronchia, superior and inferior. Left pneumonectomy was then performed, and no tumour remains were observed. The pathology study reported a mass measuring 6cm×1cm that infiltrated the entire bronchial wall, reaching the adjacent fat. The subcarinal and hilar lymph nodes were negative, but the bronchial resection edge was infiltrated by tumour.
We opted for adjuvant radiotherapy on the left bronchial bud, carina, distal trachea and right bronchial tree, with a total dose of 5940cGy. After 6 years of follow-up, the patient has presented no signs of recurrence.
Case 2A 29-year-old male with symptoms of persistent cough and dyspnoea with wheezing was diagnosed with bronchial asthma. Chest CT scan detected a tumour in the left pulmonary hilum that compressed the superior pulmonary vein and main bronchus, which was partially surrounded.
Bronchoscopy showed concentric stenosis of the primary bronchus 2cm from the tracheal carina, with submucosal growth to the interlobar carina. Biopsy revealed ACC.
Surgery was indicated, during which we observed infiltration of both lobar bronchi that required left pneumonectomy. The pathology report described a tumour measuring 4cm×4cm that infiltrated the bronchial wall and extended through the lumen to the resection edge, with lymphatic embolisation and perineural infiltration. Hilar and mediastinal lymphadenopathies did not present tumour.
The patient received adjuvant radiotherapy with a total dose of 5940cGy. Follow-up CT scan 5 years after surgery showed no signs of recurrence.
DiscussionBronchial adenoid cystic carcinomas represent 0.2% of lung cancers.1 Their nature seems more aggressive than tracheal ACC and, therefore, prognosis is worse.2 Their relationship with smoking is uncertain. There seems to be a similar distribution in both sexes, and the most typical age at presentation is the fifth decade of life, although our patients were younger. These tumours are usually located in the proximal airway and direct transluminal extension is the most frequent, although there may be submucosal/perineural infiltration at a considerable distance from the main tumour mass.3 Lymph node metastases are associated in up to 55% of cases in some series; distant metastases are less common.2,4
Three histological subtypes have been identified: cribriform, tubular and solid. Their correlation with prognosis is controversial.5
Symptoms are usually latent and nonspecific, which results in important delays in diagnosis. This happened in our two cases, which were initially managed as bronchial asthma.
As for therapeutic alternatives, chemotherapy is not useful and endoscopic options do not guarantee complete resection: their role is fundamentally palliative or temporary prior to a definitive therapy.6,7
Complete surgical resection is the treatment of choice. In bronchial tumours, pneumonectomy is usually necessary, although bronchoplasty can be an option.
Macroscopically, if the tumour involves the tracheal carina, other non-surgical options should be considered, given the difficulty to obtain adequate resection margins and the elevated perioperative morbidity and mortality associated with “sleeve” pneumonectomy.8 In some studies, however, proximal extension of the tumour to the carina is observed in the microscopic study of the bronchial resection edges, as its tendency to infiltrate the submucosa can impede a precise diagnosis in the preoperative bronchoscopy, which occurred in our two patients. In these circumstances, prolonged survivals have been reported in spite of the microscopic involvement of the resection margins.3,4,9,10 The incidence of local recurrence in these cases can reach 50% if not associated with another treatment, so some authors currently consider adjuvant radiotherapy as standard.5
The 5-year survival of this disease is estimated at around 82% for complete resection and 77% for incomplete resections.8 The possibility of recurrence years after surgical exeresis should be taken into account.
In conclusion, we believe that incomplete surgery of bronchial adenoid cystic carcinoma associated with adjuvant radiotherapy is a valid therapeutic option in selected cases. Any future endobronchial recurrences can be treated by interventional bronchoscopy.
Please cite this article as: Figueroa Almánzar S, Arnau Obrer A, García del Olmo E, Pastor Martínez E, Guijarro Jorge R. Cirugía incompleta del carcinoma adenoide quístico bronquial: una alternativa terapéutica. Cir Esp. 2015;93:606–607.