Ductal plate malformations are embryonic anomalies of the intrahepatic bile ducts that cause several types of congenital hepatic diseases, such as hepatic microhamartomas, Caroli disease and mesenchymal hamartoma. Recently diagnosed multicystic biliary hamartomas (MCBH) are uncommon hamartomatous nodular lesions that affect adults. Their origin is unknown, but they are believed to derive from a malformation of the ductal plate.1–6 Although the name MCBH was used for the first time in 2006,3 Kobayashi et al.2 had previously described a type of hamartomatous nodular lesion of the liver with similar characteristics in 2005.
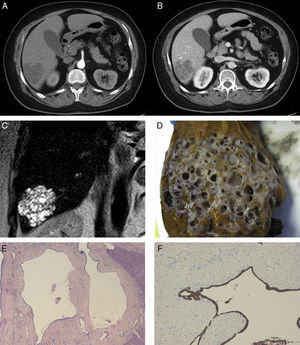
The following is a case report of MCBH and a review of the literature. This is the tenth case reported in the medical literature and the first case described in Spain (Table 1).
Clinical/Pathological Characteristics of the MCBH Cases Reported in the Literature.
| Case no. | Publication year | Author | Age (yrs)/sex | Location | Size (cm) | Symptoms | Treatment |
|---|---|---|---|---|---|---|---|
| 1 | 2005 | Kobayashi et al. | 30/M | Seg. VI | 3.6 | Incidental | Partial resection |
| 2 | 2006 | Zen et al. | 59/M | Seg. IV | 4.2 | Abdominal pain | Left hepatectomy |
| 3 | 2006 | Zen et al. | 70/F | Seg. III | 1.8 | Elevated transaminases, increased AFP | Segmentectomy |
| 4 | 2006 | Zen et al. | 69/F | Seg. III | 2.8 | Elevated transaminases | Segmentectomy |
| 5 | 2008 | Kai et al. | 55/M | Seg. VI | 5 | Incidental | Partial resection |
| 6 | 2010 | Ryu et al. | 45/M | Seg. VII | 2.0–3.5 (cases 6–8) | Incidental | Partial resection |
| 7 | 2010 | Ryu et al. | 58/M | Seg. III | – | Incidental | Partial resection |
| 8 | 2010 | Ryu et al. | 55/F | Seg. VI-VII | – | Incidental | Partial resection |
| 9 | 2012 | Song et al. | 52/M | Seg. III | 2.7 | Abdominal discomfort | Partial resection |
| Present case | 60/F | Seg. VI | 5 | Fever and abdominal discomfort | Partial resection |
F, feminine; M, masculine; Seg., segment.
Mean age=55 (range 30–70).
Male:female ratio=6:4.
Mean size ∫=3.6±1.1cm.
Most frequent location: segments III and VI.
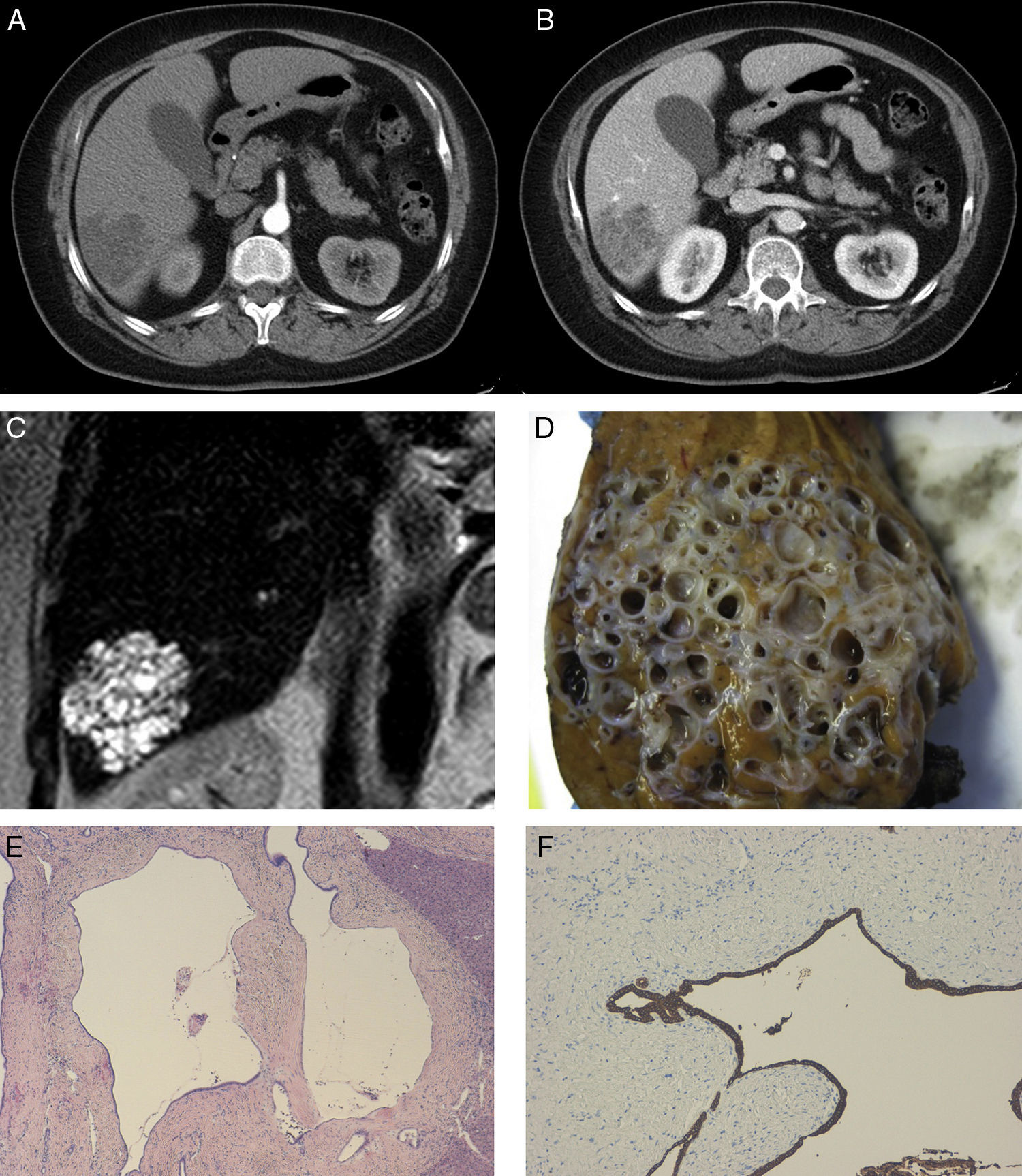
The patient is a 60-year-old woman who came to the Emergency Room with recurrent fever and abdominal discomfort in the right hypochondrium. Abdominal ultrasound showed evidence of a 6cm mass with heterogeneous structure situated in the right liver lobe. Lab work demonstrated normal levels for liver enzymes, coagulation and tumour markers (CEA 1.3, AFP 8), although Ca 19.9 levels were slightly elevated (69IU/mL). Serology was negative for HBV, HCV and HIV. CT with contrast (Fig. 1A, B) revealed a heterogeneous hypodense mass in liver segment VI measuring 5cm and millimetric bilobar lesions. Magnetic resonance cholangiopancreatography (Fig. 1C) showed the same findings. On PET-TC, the mass and small bilobar lesions had no metabolic increase. Histology study of a core needle biopsy of the mass observed a sample composed of hepatocytes and bands of biliary epithelium with no malignant characteristics, together with abundant extracytoplasmic bile pigment.
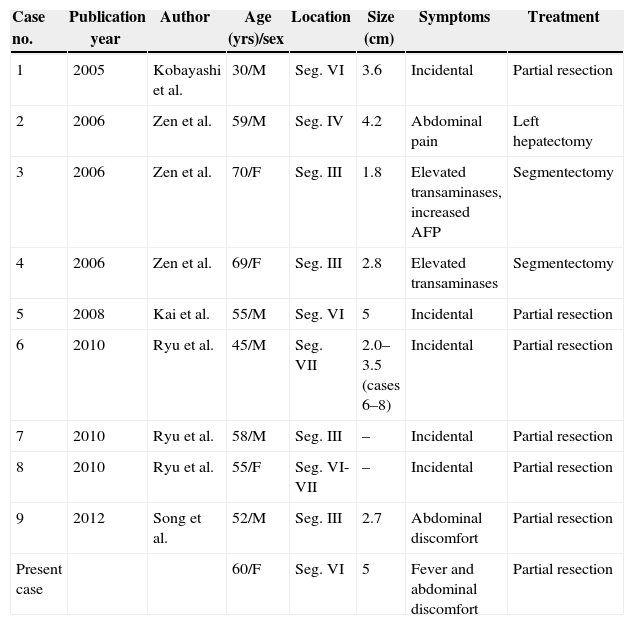
(A) Abdominal CT in arterial phase; (B) abdominal CT in portal phase with hypodense image in liver segment VI and mild intratumour contrast uptake forming septa in portal phase; (C) MRI image in T2 showing a hyperintense tumour in segment VI; (D) macroscopic image of the lesion showing the typical beehive pattern of a multicystic lesion with interposed liver parenchyma; (E) microscopic image (×4) showing dilated ductal structures with fibrosis and chronic periductal inflammation; (F) microscopic image with immunohistochemistry staining positive for CK7 and CK19.
During surgery, the mass in liver segment VI measured 5cm and had a whitish surface. Intraoperative biopsy of the tumour was solid/cystic, and the histology results were suggestive of biliary hamartoma. Tumourectomy of the lesion was performed with resection margins greater than 1cm. The definitive pathology study of the surgical specimen (Fig. 1D–F) observed macroscopically that the lesion was multicystic and had dilated ductal structures in a honeycomb pattern, with stroma and interposed liver parenchyma. Microscopically, the mass was comprised of ducts with benign characteristics that were dilated and had biliary-type material inside, with periductal glands and fibrohyaline stroma, nonspecific chronic mild inflammation and positivity of the ductal and glandular epithelium for CK7 and CK19, and negativity for Muc2, Muc5Ac and Muc6, compatible with MCBH. The patient presented an uneventful postoperative period and is currently disease free.
MCBH is a rare benign liver lesion, of which there are only 9 cases published in the literature. The clinical/pathological characteristics of these cases, including our patient, are summarised in Table 1.
As for the diagnosis based on imaging studies, abdominal ultrasound reveals a lesion with multiple small hypoechoic masses with hyperechoic septa in the interior. CT with contrast demonstrates a hypodense mass with multiple internal septa that are enhanced with contrast. On MRI in sequence T1, findings are seen that are similar to ultrasound and CT; meanwhile, in T2, MCBH is a conglomerate of small hyperdense cystic nodules.3,5,6
Histologically, the macroscopic study shows a well-defined tumour that is solid/multicystic and similar to a beehive pattern.2–6 It is characterised by: (1) subcapsular location close to the falciform ligament, most frequently in segment III, although it can be found in peripheral areas of the right liver lobe, more frequently in segment VI,2,5 and cases of intrahepatic locations have also been reported4; (2) protrusion from the liver; (3) a composition of ductal structures, periductal glands and fibrous connective tissue, which may include hepatocytes; (4) material similar to bile inside the ducts, with a variable degree of biliary xanthogranulomatous inflammation, which can reach the stroma; and, finally (5) cytokine expression of the biliary epithelium (CK7 and CK19), with negativity for Muc2, Muc5 and Muc6.2–6
The differential diagnosis should essentially include mesenchymal hamartoma, ciliated cyst of the anterior bowel and biliary cystadenoma/cystadenocarcinoma. Mesenchymal hamartomas are unique lesions comprised of ducts similar to MCBH, although they mainly affect children; histologically, they have a lax mesenchyme, distorted bile ducts and hepatocyte cords.3,6 The ciliated cyst of the anterior intestine is frequently located around the falciform ligament and close to the liver capsule, but histologically it presents a cystic wall with a pseudostratified ciliated columnar epithelium.5,6 Last of all, biliary cystadenomas have a characteristic presence of ovarian-like stroma.
Treatment involves tumourectomy with free margins, although major segmentectomies and hepatectomies have been done because of preoperative suspicion of malignant tumour (especially cholangiocarcinoma, as in our case) or due to the tumour size/location.3
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Fernández-Carrión MJ, Robles Campos R, López Conesa A, Brusadín R, Parrilla Paricio P. Hamartoma biliar multiquístico intrahepático: presentación de un caso clínico. Cir Esp. 2015;93:e103–e105.