Laryngotracheal surgery has an inherent risk of injury to the recurrent laryngeal nerves (RLN). These complications go from minor dysphonia to even bilateral vocal cord paralysis. The intraoperative neuromonitoring of the RLN was developed in the field of thyroid surgery, in order to preserve nerve and vocal cord function. However, tracheal surgery requires in-field intubation of the distal trachea, which limits the use of nerve monitoring using conventional endotracheal tube with surface electrodes. Given these challenges, we present an alternative method for nerve monitoring during laryngotracheal surgery through the insertion of electrodes within the endolaryngeal musculature by bilateral puncture.
La cirugía laringotraqueal conlleva un riesgo inherente de lesión de los nervios laríngeos recurrentes (NLR). Estas complicaciones incluyen desde una disfonía menor hasta una parálisis bilateral de ambas cuerdas vocales. La neuromonitorización intraoperatoria de los NLR se desarrolló en el campo de la cirugía tiroidea con la finalidad de preservar la función de los nervios y de las cuerdas vocales. Sin embargo, la cirugía traqueal precisa una intubación intracampo de la tráquea distal, lo que limita el uso de la neuromonitorización mediante los tubos endotraqueales convencionales con electrodos de superficie. Expuesto este reto, presentamos un método alternativo para la neuromonitorización intraoperatoria de los NLR durante la cirugía laringotraqueal mediante la inserción de electrodos en la musculatura intralaríngea a través de una punción bilateral del cartílago tiroides.
Intraoperative neuromonitoring (IONM) of the vagus nerve (VN) and the recurrent laryngeal nerves (RLN), is a well-established technique utilized in many fields. IONM can provide nerve identification and preservation, as well as guidance for intraoperative and postoperative surgical decision making. The purpose of our paper is to present a novel application of IONM in the context of laryngotracheal resection for an idiopathic subglottic stenosis.
TechniqueThis technique was used in a 43-year-old woman with idiopathic subglottic stenosis. Preoperative bronchoscopy showed the affected area in the anterior and posterior mucosa of the cricoid cartilage and the first tracheal rings. The area of maximal stenosis was 7mm in diameter and 2.5cm in length. She had intact vocal cord function. Preoperative computed tomography (CT) scan showed an unaffected cricoid cartilage.
The patient was placed in a supine position with cervical hyperextension. Ventilation after induction was performed through orotracheal intubation. Regardless of this, once the trachea was opened, ventilation was changed into an in-field intubation of the distal trachea.
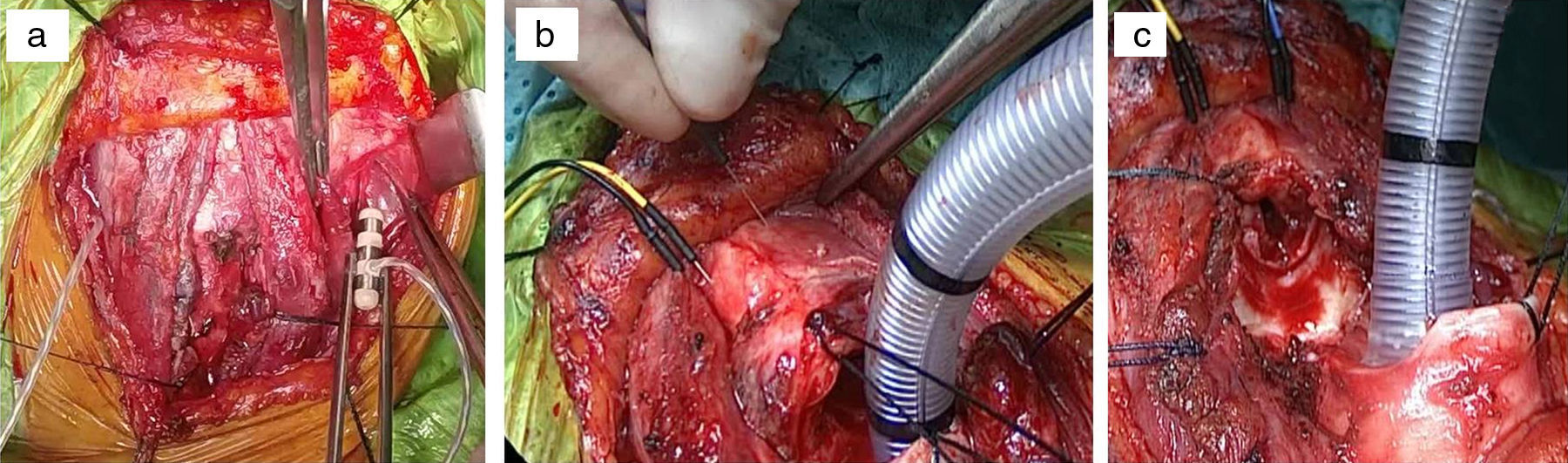
The procedure began via an anterior cervical Kocher incision, followed by dissection and exposure of the laryngotracheal axis. Bilateral neurovascular bundles (internal jugular vein, carotid artery and VN) were dissected, in order to place the VN stimulators,1 and then insertion by direct punction of the recording electrodes within endolaryngeal musculature (Fig. 1a,b). Posterior mapping of the RLN aided its visual location to decrease the risk of injury. Identification of neuromiotonic discharges over the vocal cord muscles secondary to manipulation of neural structures, thermal mechanism or bleeding, also alerted us about the risk of injury. Once the IONM electrodes were placed, we did proceed to resection of the cricoid ring mucosa and cartilage, the mucosa of the cricoid plate and the first 4 tracheal rings (Fig. 1c), followed by a reconstruction according to the previously described technique by Grillo2 (as shown in the animation “Online resource 1”). At the end of the procedure as no Montgomery T tube was necessary, we exchanged the in-field distal tracheal tube for a nasotracheal tube with surface electrodes for clinical and neurophysiologic monitoring.
(a) Placement of stimulators following bilateral dissection of the neurovascular bundles. (b) Insertion of electrodes within endolaryngeal musculature by bilateral puncture of the thyroid cartilage near the vocal cords area. (c) Resection of the cricoid plate mucosa, cricoid ring and the first 4 tracheal rings. In field distal tracheal intubation.
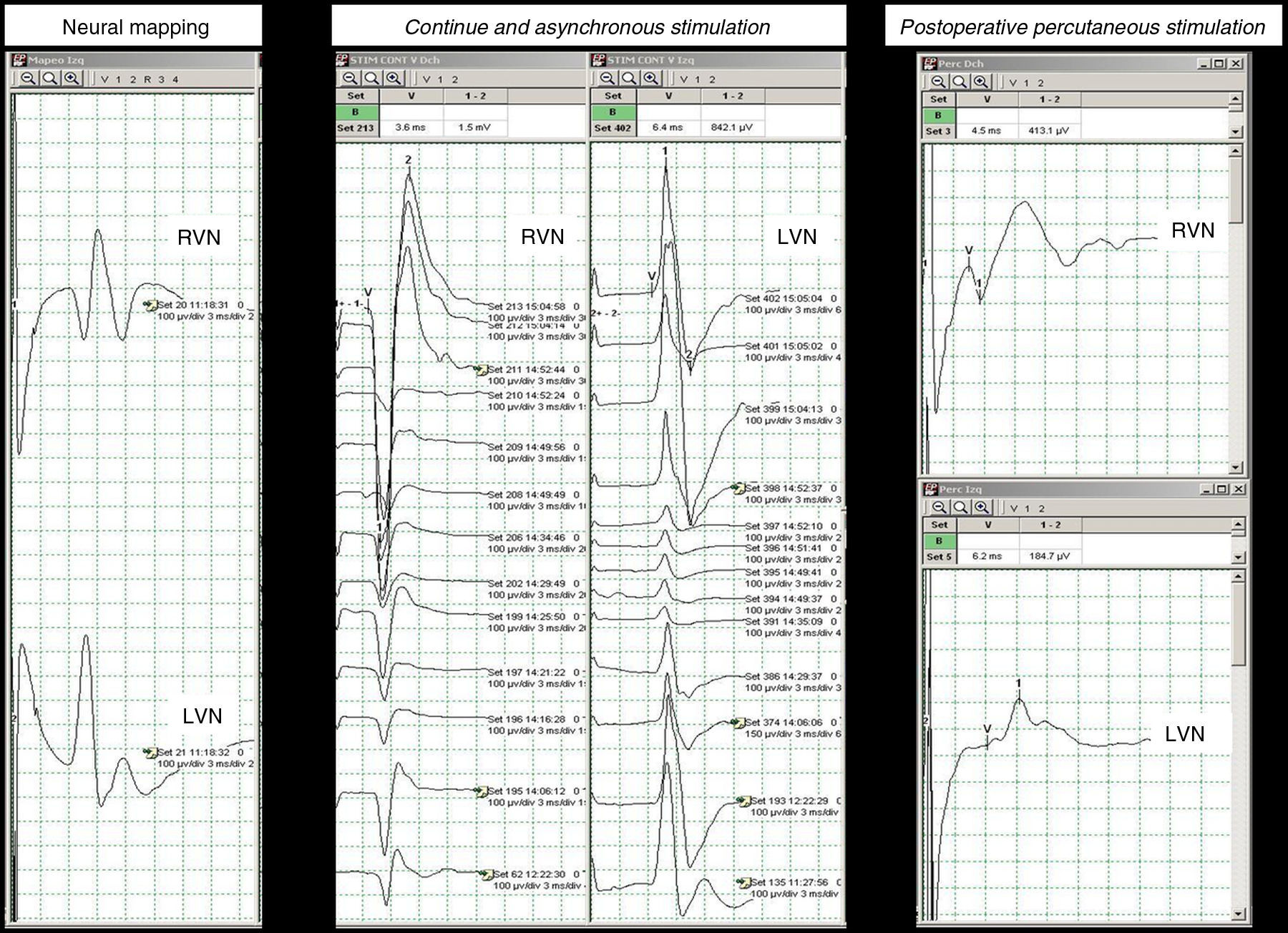
The loss of signal during IONM is defined as motor response <100μV with stimulation of the VN, and this is interpreted as neural injury in the absence of technical problems or anesthetic changes3 (absent in our case). Motor responses of higher amplitude (>100μV) are related to preservation of VC and RLN function, which must be proven at the end of the procedure via stimulation of the VN.4 In our case, the amplitude at the end of the procedure was: right VN 1500μV; left VN 800μV.
During the surgery, no functional damage was recorded to the VC. We monitored VC function using bilateral and asynchronous stimulation of the VN with the previously placed electrodes (Fig. 2). This method would have allowed to identify the mechanism of injury, as well as, defining the type of injury which would have helped us to establish a functional prognosis for the patient just in case it was needed. If a bilateral loss of signal had been registered and depending on the type of insult, we would have recommended delayed and controlled extubation and/or additional surgical maneuvers depending on VC position and surgeon's experience, being endoscopic laser VC cordotomy followed by temporary tracheal tutoring the most effective one.
Given the proximity of the resection to the VC and the possibility of postoperative laryngeal edema, we decided to keep the nasotracheal tube for 24h, allowing the patient to be awake with spontaneous ventilation. Prior to extubation we performed a transcutaneous test of the VN by stimulating over the anterior edge of sternocleidomastoid muscle, with registry by the surface electrodes of nasotracheal tube localized at the level of VC. The result of this test was satisfactory (Fig. 2) corroborating the immediate postoperative findings. We also performed a flexible laryngotracheoscopy, which confirmed the movement of the VC, no evidence of laryngeal edema or problems related to the anastomosis. She was discharged on postoperative day 21, and is currently doing well. She has normal tracheal caliber and has no alterations in phonation, deglutition or ventilation after a 9-month follow-up.
CommentThe use of IONM in laryngotracheal surgery is very important since nerve injury can exist despite macroscopic nerve integrity. The most common mechanism of nerve injury is still traction and thermic injury, resulting in a transient neurapraxia.
The use of standard tracheal tubes with surface electrodes used in other procedures (e.g. thyroid surgery) is not feasible due to the implication of the subglottic area just below the VC, and the need of opening the trachea and in-field distal tracheal intubation, with subsequent malpositioning of the electrodes nearby the vocal cords area. This prompted us to perform the IONM via inserting the electrodes directly into the endolaryngeal musculature5 through the thyroid cartilage, as previously also described in animal experimental model,6 resulting in a safe and relatively simple method and without interfering with surgical maneuvers.
In conclusion, we believe that IONM of the RLN using the above described technique can be applied to the different methods of laryngotracheal reconstruction, including cases requiring laryngofissure. Our technique does not interfere with the operative field and provides real-time functional status of the VC decreasing the risk of RLN injury, and also a potential emergent situation once the patient is extubated.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Bolufer S, Coves MD, Gálvez C, Villalona GA. Neuromonitorización intraoperatoria en cirugía laringotraqueal. Cir Esp. 2017;95:342–345.