The use of tissue adhesives can be an alternative to suture fixation of the mesh, but experience in their use is very limited.
Material and methodsA prospective descriptive study was conducted on a group of 35 patients with inguinal hernias repaired by sutureless hernioplasty (20 by open and 15 by endoscopic), the prosthesis was fixed with a synthetic adhesive (n-hexyl-α-cyanoacrylate). This group was compared with another 35 patients for hernia repair with fixation sutures. All patients were scheduled for outpatient surgery. Peri-operative variables were recorded. The patients were followed up at one week, one month, 6 months and one year after surgery.
ResultsThere was no morbidity associated with the use of tissue adhesive (bruising, infection or skin necrosis). During a median follow-up of 15 months, no complications or recurrences were detected. In the open hernioplasty using adhesive significantly reduced surgery time (30min versus 70min, P=.001), postoperative pain (from 2.4 to 4.5 at one week, P<.001) and analgesic consumption (7–14 days, P<.001). In the laparoscopic approach are demonstrated significant differences in favor of the adhesive in pain (P=.001 at 24h), and in analgesic use (P<.001) was observed using the laparoscopic approach. The adhesive did not alter the morbidity or the relapse rate at one year in any of the two approaches, and the financial analysis showed an annual savings of 117461.2 euros (about 460 hernias).
ConclusionThe use of a synthetic tissue adhesive (n-hexyl-α-cyanoacrylate) is safe as a means of fixation in uncomplicated hernia and patients without comorbidity, and with good postoperative results.
El uso de adhesivos tisulares puede ser una alternativa a la sutura en la fijación de la malla, pero su experiencia clínica es muy limitada.
Material y métodosEstudio prospectivo y descriptivo en un grupo de 35 pacientes con hernias inguinales operados mediante hernioplastia sin sutura (20 vía abierta y 15 vía endoscópica); la prótesis se fijó con adhesivo sintético (n-hexil-α-cianoacrilato). Este grupo se ha comparado con uno control operado mediante hernioplastia utilizando suturas. Todos los pacientes seguían protocolo de cirugía mayor ambulatoria. Se han registrado variables peri- y postoperatorias. El seguimiento se realizó a la semana, al mes, a los 6 meses y al año.
ResultadosNo ha existido morbilidad asociada con el uso del adhesivo tisular. Durante una mediana de 15 meses no se han detectado complicaciones ni recurrencias. En la hernioplastia abierta el uso del adhesivo disminuye de forma significativa el tiempo quirúrgico (30min versus 62min, p = 0,001), el dolor postoperatorio (de 2.4 a 4.5 a la semana, p < 0,001) y el consumo de analgésico (de 7 a 14 días, p < 0,001). En el abordaje laparoscópico se demuestran diferencias significativas a favor del adhesivo en el dolor (p = 0,001 a las 24h) y consumo de analgésicos (p < 0,001). El análisis económico demuestra un ahorro anual de 117.461,2 euros (sobre 460 hernias).
ConclusiónEl uso de un adhesivo tisular sintético (n-hexil-α-cianocrilato) es seguro como medio de fijación en las hernioplastias no complejas en pacientes sin comorbilidad, con buenos resultados postoperatorios.
Abdominal wall surgery is continuously changing. In recent decades, mesh has been accepted for repairing abdominal wall defects. We are currently witnessing a new cycle of changes as a consequence of the introduction of tissue adhesives, which are substances that can be used as hemostatics or adhesives in multiple medical-surgical processes.1–5 Hernia treatment represents an elevated expenditure of resources within a general surgery department and can reach 15% of its overall activity. Tension-free hernioplasty has become the standard method for treating inguinal hernias because it is an effective, easily reproducible intervention that provides good results for most surgeons. However, this surgery still presents an important rate of postoperative pain.6 This complication has been related to the use of sutures that may cause local compression (tissue ischemia), strangulation of muscle fibers, nerve damage, or foreign body reaction.
The purpose of this study is to assess the effectiveness of a synthetic tissue adhesive (n-hexyl-α-cyanoacrylate) in the treatment of inguinal hernia, with both open as well as laparoscopic approaches, as a substitute for sutures.
MethodsStudy DesignThis prospective, descriptive, non-randomized study compares the study group with a control group during the time period from January 2008 to January 2011; 35 patients were included, all diagnosed with inguinal hernias treated with tension-free hernioplasty. All patients were evaluated by a multidisciplinary unit specialized in abdominal wall disorders, where a detailed clinical history was taken and patients underwent physical examination.
Tissue AdhesiveA monomer of cyanoacrylate was used (n-hexyl-α-cyanoacrylate, IfabondTM, Fimed, France), which is a very pure adhesive with low viscosity that, when applied over living tissue in a moist basic environment, polymerizes rapidly and forms a flexible adhesive polymer in seconds. After 30s, it provides strong fixation; its reabsorption is progressive and complete 3 months after application.
Inclusion/exclusion CriteriaThe inclusion criteria included: patients over the age of 17 with inguinal hernias without comorbidity (DRG 162) who understood the process and gave their informed consent. In the case of unilateral hernias, types ii and iii of the Nyhus classification were included and proposed for anterior open hernioplasty. Bilateral hernias were considered for endoscopic total extraperitoneal repair. Exclusion criteria included scrotal hernias, recurrences, emergency surgery, the presence of infection or lack of signed informed consent.
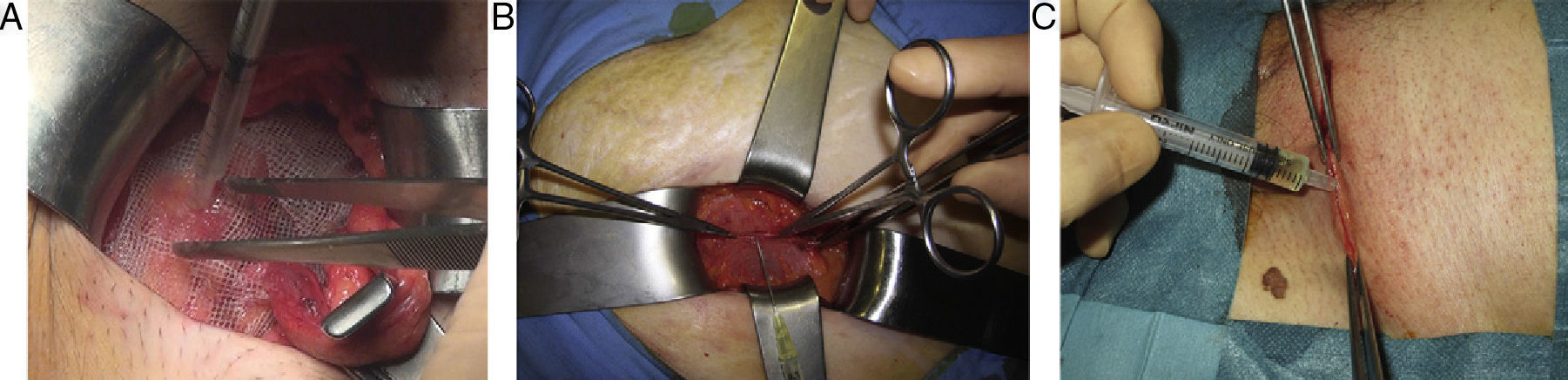
Surgical Technique(a) Open technique: under regional anesthesia, a Lichtenstein or Rutkow technique was performed. In the technique with sutures, a 5-cm plug was set with one stitch, and a flat polypropylene mesh measuring 15cm×7.5cm was placed using 2 size 2/0 polypropylene sutures (2/0 Prolene®, Ethicon, Chicago, USA), the aponeurosis of the external oblique muscle was likewise sutured with size 0, the subcutaneous tissue was closed with size 0 synthetic absorbable polyglycolic acid suture (SSA®, Ethicon, Chicago, USA) and the skin was closed with staples. In the technique without sutures, the surgical management of the region, hernia, sac and mesh position was the same, but both the plug as well as the flat mesh were attached with well-distributed drops of n-hexyl-α-cyanoacrylate, on the plug at the edge of the ring and on the flat mesh to the pubis, inguinal ligament and internal oblique muscle, keeping the area to be adhered dry and with previous identification of the inguinal nerves to avoid their contact during polymerization. The other planes (aponeurosis of the external oblique, fascia of scarpa and skin) were also closed with tissue adhesive (Fig. 1).
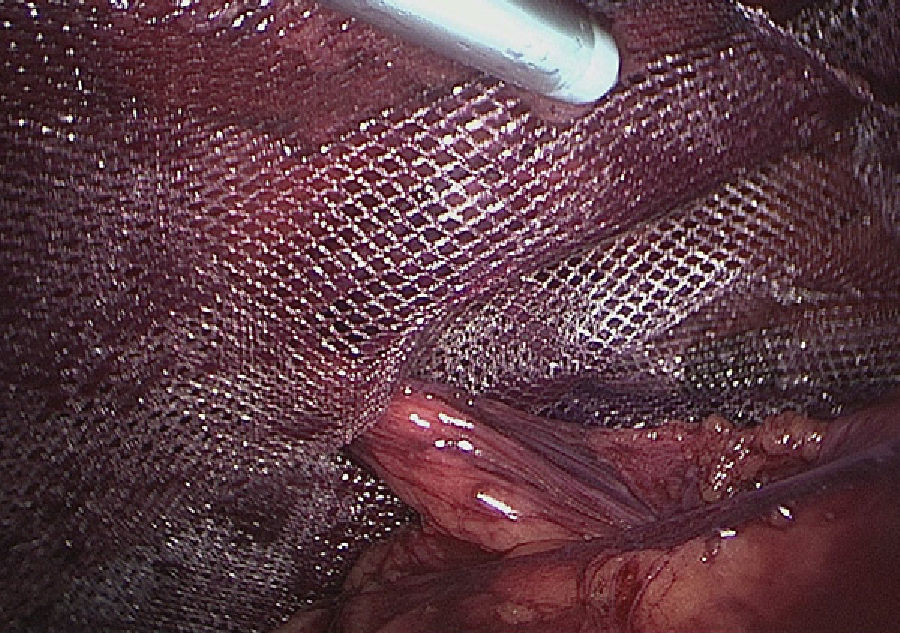
(b) Laparoscopic technique: following the standardized total extraperitoneal (TEP) technique, using a 15×15cm preformed, low-density, covered titanium mesh (35g/m2) and attached to the Cooper ligament with 2 reabsorbable sutures (Securestraps®, Ethicon, USA) in the control group, or with synthetic adhesive in the study group. The adhesive was introduced with a cannula and applied in drops, pressing the mesh with forceps against the posterior wall in order to guarantee contact during crystallization (Fig. 2).
Follow-upAll patients were included in a follow-up protocol and reviewed at the Abdominal Wall Unit outpatient clinic 1 week postoperatively, 1 month, 6 months and at the end of 1 year. The parameters evaluated were: clinical (age, sex and body mass index), peri- and early postoperative parameters (surgical time, morbidity [hematoma, seroma and surgical wound infection], number of participating surgeons and their experience) and follow-up (pain, consumption of analgesics and recurrence). Hematomas and seromas were defined clinically, the former as the accumulation of blood in the area of the surgical wound and the latter as the presence of a liquid collection that persisted for more than 4 weeks or caused local discomfort. Recurrences were determined by means of physical exploration and ultrasound. Pain was quantified in a standardized manner with a visual analog scale (VAS) from 0 to 10, 0 representing absence of pain and 10 the maximum pain imaginable. The consumption of analgesics was written down by the patients on cards they were given at discharge, which they filled out each day. All patients completed the 12-month follow-up.
Control Group – Comparative AnalysisDuring the same study period, the same number of patients with inguinal hernias and comparable clinical variables were randomly selected for the comparative study. Due to department organizational factors, they were not randomized for either the classical approach or the laparoscopic approach in the case of bilateral hernias.
Economical AnalysisA basic study was done of the hospital costs of the process according to treatment, using the computer data provided by the hospital for the year 2010. All the expenses generated by each patient in the day hospital were reviewed.
Statistical AnalysisThe patients were analyzed according to surgical treatment (with or without sutures) and type of approach. For the description of quantitative variables, means and standard deviation were used; for qualitative variables, the proportion was used. In order to study the normalcy of the quantitative variables, the Kolmogorov–Smirnoff test was used. For the comparison of means when the quantitative variable did not follow a normal distribution, the Mann–Whitney U test was used, and Student's t test for the quantitative variables with normal distribution normal and equal variance between the 2 groups. The Chi-square test, with Fisher's exact correction, was used for the analysis of the qualitative data. A P<.05 was considered statistically significant. All the calculations were done using the SigmaStat statistical program (Jandel Scientific, Carlsbad, CA, USA).
ResultsThe mean age of the patients who underwent inguinal hernia repair by means of hernioplasty without sutures, and with synthetic tissue adhesive was 57, with a predominance of men (66%) over women (34%). The types of hernias were 60% Nyhus type III and the remaining 40% type II. The Rutkow technique was used in 10 cases (50%). All patients were discharged in accordance with the ambulatory protocol, with no required hospitalization or later readmittance during the follow-up period. There has been no morbidity associated with the use of synthetic tissue adhesive (hematomas, wound infections or skin necrosis). During follow-up, the evolution was satisfactory in all cases, with no complications or recurrences up to the end of the study. Mean follow-up was 16 months, with a range from 12 to 26 months.
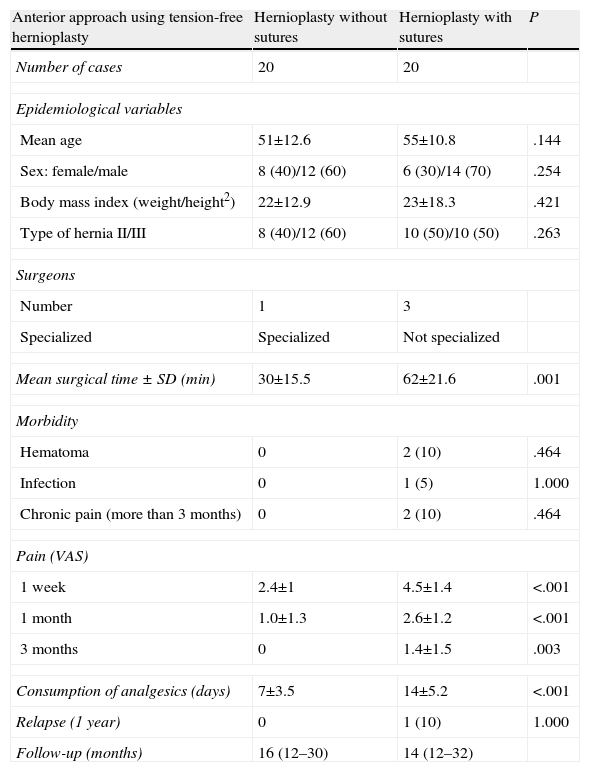
Comparative Study – Open ApproachThe comparative analysis of inguinal hernia treatment with the anterior approach is shown in Table 1. The control group was treated by 3 experienced surgeons (not residents) who are not exclusively dedicated to abdominal wall surgery. The surgical time was significantly shorter with the non-suture technique (30min in hernioplasty with adhesive versus 62min using sutures, P=.001). Postoperative morbidity was similar from a statistical standpoint, although in the group with adhesive no complications were found, while in the suture group there were 2 cases of hematomas and pain for more than 3 months and one case of superficial infection of the wound. The pain and analgesia variables were statistically different, favoring the non-suture group (P<.001). During follow-up, recurrence was detected in the suture group in one patient who had been operated on by a surgeon who was not specialized in abdominal wall surgery, which was diagnosed 6 months post-op and confirmed by ultrasound.
Intraoperative and Postoperative Morbidity of the Patients Operated on for Inguinal Hernia (DRG 162) According to Technique.
| Anterior approach using tension-free hernioplasty | Hernioplasty without sutures | Hernioplasty with sutures | P |
| Number of cases | 20 | 20 | |
| Epidemiological variables | |||
| Mean age | 51±12.6 | 55±10.8 | .144 |
| Sex: female/male | 8 (40)/12 (60) | 6 (30)/14 (70) | .254 |
| Body mass index (weight/height2) | 22±12.9 | 23±18.3 | .421 |
| Type of hernia II/III | 8 (40)/12 (60) | 10 (50)/10 (50) | .263 |
| Surgeons | |||
| Number | 1 | 3 | |
| Specialized | Specialized | Not specialized | |
| Mean surgical time±SD (min) | 30±15.5 | 62±21.6 | .001 |
| Morbidity | |||
| Hematoma | 0 | 2 (10) | .464 |
| Infection | 0 | 1 (5) | 1.000 |
| Chronic pain (more than 3 months) | 0 | 2 (10) | .464 |
| Pain (VAS) | |||
| 1 week | 2.4±1 | 4.5±1.4 | <.001 |
| 1 month | 1.0±1.3 | 2.6±1.2 | <.001 |
| 3 months | 0 | 1.4±1.5 | .003 |
| Consumption of analgesics (days) | 7±3.5 | 14±5.2 | <.001 |
| Relapse (1 year) | 0 | 1 (10) | 1.000 |
| Follow-up (months) | 16 (12–30) | 14 (12–32) | |
The numbers in parentheses are percentages.
SD, standard deviation; VAS, visual analogical scale.
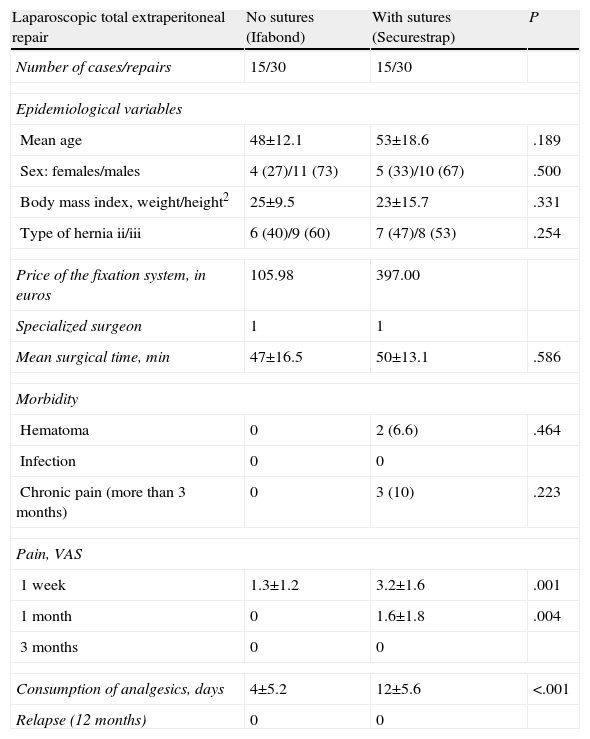
The comparative study of bilateral inguinal hernia surgery with a laparoscopic total extraperitoneal approach is shown in Table 2. Both groups were operated on by the same surgeon who is highly specialized in abdominal wall surgery (exclusive dedication for more than 15 years and 500 laparoscopies performed). We have found no significant differences in surgical time or in postoperative morbidity, although from a descriptive standpoint the percentage of hematoma or pain was higher in the group where the mesh was attached with mechanical suture (13.3% and 20%, respectively). Significant differences were demonstrated between the two forms of mesh placement in the variables of pain (P=.001 at one week) and consumption of analgesics (P<.001), which were lower in the group with synthetic tissue adhesive. We have detected no recurrences in either of the 2 groups.
Intraoperative and Postoperative Morbidity of Patients who Underwent Bilateral Inguinal Hernia Repair With Laparoscopic Total Extraperitoneal Approach, According to Technique.
| Laparoscopic total extraperitoneal repair | No sutures (Ifabond) | With sutures (Securestrap) | P |
| Number of cases/repairs | 15/30 | 15/30 | |
| Epidemiological variables | |||
| Mean age | 48±12.1 | 53±18.6 | .189 |
| Sex: females/males | 4 (27)/11 (73) | 5 (33)/10 (67) | .500 |
| Body mass index, weight/height2 | 25±9.5 | 23±15.7 | .331 |
| Type of hernia ii/iii | 6 (40)/9 (60) | 7 (47)/8 (53) | .254 |
| Price of the fixation system, in euros | 105.98 | 397.00 | |
| Specialized surgeon | 1 | 1 | |
| Mean surgical time, min | 47±16.5 | 50±13.1 | .586 |
| Morbidity | |||
| Hematoma | 0 | 2 (6.6) | .464 |
| Infection | 0 | 0 | |
| Chronic pain (more than 3 months) | 0 | 3 (10) | .223 |
| Pain, VAS | |||
| 1 week | 1.3±1.2 | 3.2±1.6 | .001 |
| 1 month | 0 | 1.6±1.8 | .004 |
| 3 months | 0 | 0 | |
| Consumption of analgesics, days | 4±5.2 | 12±5.6 | <.001 |
| Relapse (12 months) | 0 | 0 | |
The amounts in parentheses are percentages.
SD, standard deviation; VAS, visual analogical scale.
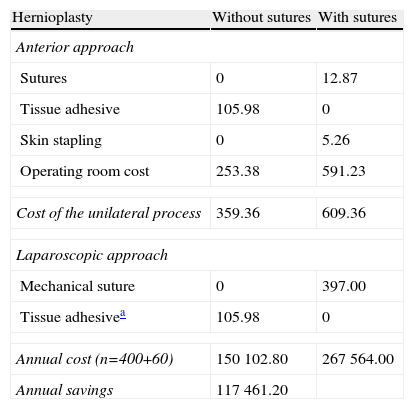
The detailed cost analysis of the process is shown in Table 3. The total cost in our hospital of anterior hernioplasty with sutures was 609.36 euros, versus 359.36 euros when using an adhesive (difference: 250 euros). The difference in price between the groups with sutures and without sutures using the anterior approach can be attributed to operating room expenses, which is more than double in the suture group. The use of tissue adhesive in the laparoscopic approach for bilateral hernias did not modify surgical time, and the difference in cost was due to the system of fixation, with a savings of 291 euros per patient. With an annual number of 400 unilateral hernias and 60 bilateral hernias (hospital data from 2010), with this process alone in an Abdominal Wall Unit the potential savings would be 117461.2 euros (Table 3).
Cost Analysis (in euros) at our Hospital of Unilateral Inguinal Hernia Surgery Without Complications (DRG 162) and Bilateral Hernias, According to Technique.
| Hernioplasty | Without sutures | With sutures |
| Anterior approach | ||
| Sutures | 0 | 12.87 |
| Tissue adhesive | 105.98 | 0 |
| Skin stapling | 0 | 5.26 |
| Operating room cost | 253.38 | 591.23 |
| Cost of the unilateral process | 359.36 | 609.36 |
| Laparoscopic approach | ||
| Mechanical suture | 0 | 397.00 |
| Tissue adhesivea | 105.98 | 0 |
| Annual cost (n=400+60) | 150102.80 | 267564.00 |
| Annual savings | 117461.20 | |
The sutures used were: polypropylene 2/0 (n=2) and 0, and absorbable polyglycolic acid 2/0 synthetic suture. The number of annual unilateral inguinal hernia was 400 and 60 were bilateral.
The results of this study show that, in patients without comorbidity, a synthetic tissue adhesive (n-hexyl-α-cyanoacrylate) is able to substitute the use of sutures in the treatment of surgical wounds smaller than 5cm in any plane of the abdominal wall (fascia, muscle, aponeurosis or skin). Abdominal wall surgery is constantly changing. Prostheses were the first revolution in hernia surgery and laparoscopy is the second important development, although it still has not become consolidated due to training problems, costs and because the results have not been as positive for hernia repair or the patients themselves. We are currently witnessing the dawning of a third revolution brought about by the development of tissue adhesives. In the next few years, these substances could change the way surgical techniques are performed and modify the traditional image that we surgeons portray (hands–port–suture).
Synthetic tissue adhesives derived from cyanoacrylate have a common chemical structure and their physicochemical properties vary depending on the length of their alkyl chain, which determines biodegradation speed. Short-chain derivatives (methyl and ethyl) have been ruled out due to their histotoxicity, a consequence of their rapid biodegradation.1,2 The ideal synthetic tissue adhesive for use in hernia surgery should be biocompatible, fast-acting, easily applied and economical. Long-chain derivatives (butyl, hexyl or octyl) have demonstrated these properties and an absence of adverse effects by having a slower biodegradation (minimum local inflammatory response), which has extended its use to general surgery, traumatology, otorhinolaryngology, ophthalmology, maxillofacial and odontology, vascular surgery, urology, plastic surgery, plastic surgery, gynecology, etc.1–5
In hernia surgery, the first publications related to the use of a synthetic tissue adhesive were written by Farouk in 1996, with an anterior approach, and by Jourdan in 1998, using laparoscopy.7,8 Afterwards, other authors have published favorable results with both approaches.9,10 Our present study, however, is the first to use adhesives as a substitute for sutures in all the planes of the abdominal wall.11 Hernioplasty, regardless of the approach, can be associated with pain and paresthesia in a percentage of patients that may range between 10% and 30%.6 Testini, Brügger and others have published lower postoperative pain rates with tissue adhesives.12–14 This study confirms this clinical finding. This could be explained by the total lack of sutures, which could be the origin of the periosteal inflammation of the pubis, muscle fiber tension, nerve entrapment or injury, inflammation or rejection, reaction to a foreign body, granulomas, etc. The use of an adhesive may avoid these phenomena and give physiological support to the concept of the tension-free technique, which is usually done with sutures.
The use of a synthetic tissue adhesive in hernia repair may provide other clinical benefits such as a hemostatic effect. This study found a lower percentage of hematomas in the group treated with adhesives, in both approaches. Moreover, an antibacterial effect has also been reported, a fact that could reduce the risk of local infection.15–17 Another point to consider is the fact that, aside from the material used to hold the mesh or close a surgical wound, the “surgeon factor” is also a determinant of the final result. It is well known that a surgeon specialized in abdominal wall repair obtains better results than a non-specialized surgeon.18 This study supports this fact regardless of the approach used although this factor may mean an important bias in the interpretation of the results. The effect of the tissue adhesive can be compromised by certain local conditions, such as excess fat, the presence of blood, large wounds (>5cm) or low tension (cannot be approximated). In these cases, it is recommendable to use sutures but, if the surgeon has experience in the management of tissue adhesives, the author suggests that in selected patients and cases, mattress stitches every 4cm can be used and complete the rest of the wound with adhesive. The esthetic results seem to be better.
The total extraperitoneal laparoscopic approach is accepted as an alternative treatment in bilateral and recurrent inguinal hernias.19,20 Prior meta-analyses have demonstrated that the fixation of the mesh to the extraperitoneal plane is unnecessary in normal conditions.21–23 After a randomized study in 2004, the author has only used it for recurring and bilateral hernias,24 but this new study demonstrates that the substitution of mechanical fixation with synthetic tissue adhesive in the laparoscopic technique improves morbidity and reduces the cost of the process.
In the present socioeconomic situation, hospital expenses are one of the main concerns of the healthcare system. The management of healthcare resources becomes a priority and each department or management unit should collaborate as much as possible. The use of fibrin glue is much more expensive, requires previous preparation of the product, presents important risks and is not comparable with synthetic adhesives that are proposed alternatives to the traditional use of manual or mechanical sutures. Our cost analysis shows that the use of a synthetic tissue adhesive in the treatment of inguinal hernias can represent an important annual savings.
The limitations of the present study include the lack of randomization in its design and the inclusion of surgeons with different levels of experience and dedication, factors that could justify the differences in surgical time and morbidity.
In conclusion, n-hexyl-α-cyanoacrylate tissue adhesive is safe as a medium for fixation in non-complex hernioplasties and in patients without comorbidity, providing good postoperative results. Given that the design of this study has limitations based on the varying experience of the surgeons, a randomized study is necessary with a larger number of patients to confirm these results.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Moreno-Egea A. ¿Es segura la hernioplastia sin sutura como opción para tratar las hernias de pared abdominal? Estudio prospectivo con un adhesivo tisular sintético (n-hexil-α-cianoacrilato). Cir Esp. 2013;91:243–249.