The purpose of this study was to analyze the relationship between preoperative serum levels of vitamin D and postoperative hypocalcemia after total thyroidectomy.
Material and methodsA prospective observational study was conducted on 113 patients treated by total thyroidectomy due to benign disease. Preoperative vitamin D serum levels and postoperative albumin-corrected calcium and parathormone (PTH) levels were determined. Sensitivity, specificity, positive predictive value and negative predictive value of vitamin D and PTH levels, respectively, in the diagnosis of postoperative hypocalcemia were calculated.
ResultsHypocalcemia was diagnosed in 44 (38.9%) patients. Vitamin D levels were significantly higher in the group of patients with normal postoperative calcium (median: 25.4pg/mL; range: 4–60), compared to those who developed hypocalcemia (median: 16.4pg/mL; range: 6.3–46.9) (P=.001). Postoperative hypocalcemia was more frequent in patients with vitamin D<30ng/mL (39/78) (50%), than among those with normal levels (5/35) (14.2%) (P=.001). Sensitivity, specificity, positive predictive value and negative predictive value were 88% and 68%, 43% and 82%, 50% and 71%, and 85% and 80% for vitamin D and PTH, respectively. Vitamin D and PTH showed independent prognostic values on the risk of hypocalcemia. The OR associated with vitamin D<30ng/mL was 4.25 (95% CI: 1.31–13.78) (P=.016), and the OR of PTH<13pg/mL was 15.4 (95% CI: 4.83–49.1) (P<.001).
ConclusionVitamin D deficiency is a risk factor of hypocalcemia after total thyroidectomy for benign goiter. The vitamin D level provides independent prognostic information, which is complementary to that given by PTH.
El objetivo de este estudio fue analizar la relación entre concentración sérica preoperatoria de vitamina D y la hipocalcemia tras tiroidectomía total.
Material y métodosEstudio prospectivo observacional que incluyó a 113 pacientes operados de tiroidectomía total por enfermedad benigna. Se determinaron las concentraciones preoperatorias de vitamina D y las concentraciones postoperatorias de calcio corregido por albúmina y hormona paratiroidea intacta (PTH). Se calcularon la sensibilidad, especificidad, valor predictivo positivo y valor predictivo negativo de los niveles de vitamina D y PTH para diagnosticar la hipocalcemia postoperatoria.
ResultadosDe los 113 pacientes, 44 (38,9%) presentaron hipocalcemia. La concentración preoperatoria de vitamina D fue superior en el grupo de pacientes con calcemia postoperatoria normal (mediana: 25,4ng/mL; rango: 4-60) que en los que desarrollaron hipocalcemia (mediana: 16,4ng/mL; rango: 6,3-46,9) (p = 0,001). La hipocalcemia fue más frecuente en los pacientes con vitamina D < 30ng/mL (39/78) (50%) que en aquellos con vitamina D normal (5/35) (14,2%) (p = 0,001). La sensibilidad, especificidad, valor predictivo positivo y valor predictivo negativo de la vitamina D y la PTH fueron 88 y 68%, 43 y 82%, 50 y 71%, 85 y 80%, respectivamente. La vitamina D y la PTH mostraron valor pronóstico independiente. La odds ratio de hipocalcemia para la vitamina D < 30ng/mL fue 4,25 (IC 95%: 1,31-13,78) (p = 0,016), inferior a la asociada con PTH < 13pg/mL, 15,4 (IC 95%: 4,83-49,1) (p < 0,001).
ConclusiónLa vitamina D es un factor de riesgo de aparición de hipocalcemia postoperatoria tras tiroidectomía total por bocio benigno. El nivel de vitamina D proporciona información predictiva independiente y complementaria a la aportada por la PTH.
Total thyroidectomy (TT) is the procedure of choice for the surgical treatment of benign multinodular goiter. Postoperative hypocalcemia is the most frequent complication. It is usually mild and transitory (in up to 50% of cases) and rarely permanent (5%). Nevertheless, it is always a concern and a challenge for surgeons, and for patients it entails the need for additional treatment.1,2
The etiology of postoperative hypocalcemia is multifactorial, although the most important component is surgical trauma to the parathyroid glands. TT may cause hypoparathyroidism due to the unnoticed removal of the parathyroid gland or damage to its blood supply. Several factors influence surgical trauma: experience of the surgeon, careful tissue manipulation, number of parathyroid glands detected and preserved, and extent of the surgical exeresis (intrathoracic goiter, central lymphadenectomy, reinterventions).1–3 Recent studies have highlighted the role of parathyroid hormone (PTH) levels as a predictive factor for post-thyroidectomy hypocalcemia.4–8 PTH concentrations are an indicator of the volume of functioning parathyroid tissue and objectively indicate the effect of surgery on parathyroid glands.
It has been observed that vitamin D deficiency favors the appearance of postoperative hypocalcemia in patients who undergo surgery for multinodular goiter or Graves’–Basedow disease.9–12 Vitamin D plays a central role in the homeostasis of calcium,13–15 favors the intestinal absorption of calcium and phosphate, diminishes the secretion of PTH and stimulates the differentiation of osteoclasts.13,14 The organism synthesizes its active form in the kidneys (1-25[OH]D3) through a process controlled by PTH, and therefore, by increasing vitamin D levels, the secretion of PTH is reduced. If this connection between preoperative vitamin D deficiency and postoperative hypocalcemia is confirmed, vitamin D levels could be a good indicator of this risk that could be easy to measure and correct before surgery.
The objective of the present study was to analyze the value of preoperative vitamin D as an indicator of risk for developing hypocalcemia after TT due to benign goiter and to compare the results with those provided by clinical data and by PTH determination.
Material and MethodsWe present a prospective, observational study of risk factors and evaluation of diagnostic tests, carried out between December 2009 and December 2011 in the General Surgery Department at the Hospital Príncipe de Asturias in Alcalá de Henares, Spain.
Considered for study were those patients who underwent TT due to benign thyroid disease. We did not include patients who were treated for thyroid cancer or those who presented concomitant parathyroid disease, or those who underwent reintervention for the total removal of the gland. A total of 136 patients participated in the study, 23 of whom were later excluded because one of the analytical parameters had not been determined. The final analysis included 113 patients: 95 with bilateral multinodular goiter and 18 with Graves’–Basedow disease; 95 women (84%) and 18 men (16%), with a mean age of 51 (range: 18–77 years.). All underwent bilateral TT. During surgery, a special effort was made to locate and identify the parathyroid glands and recurrent nerves. When compromised vascular supply was observed in one of the glands, autotransplantation was performed in the homolateral sternocleidomastoid muscle.
Preoperative studies determined the serum concentrations of creatinine, TSH, calcium, albumin and 25-hydroxyvitamin D3 (vitamin D). In the postoperative period, calcium levels were determined at 24 and 48h after the intervention and the amount of calcium was calculated and corrected for the level of albumin. PTH levels were determined in the blood sample obtained on the morning of the day after surgery.
An electro immunochemiluminescence method was used for the determination of vitamin D concentrations (Liaison®, DiaSorin, Saluggia, Italy). For this study, the lower limit of normal was set at 30ng/mL in accordance with previous publications.15,16 For the analysis of PTH, a commercial kit was used based on the immunochemiluminescence technique (Immulite Intact PTH, Siemens Healthcare Diagnostic, IL, USA). A value of 13pg/mL was considered the lower limit of normal.8
The Chvostek and Trousseau signs and the appearance of postoperative hypocalcemia symptoms (paresthesias, muscle spasms) were evaluated from surgery up until discharge. Postoperative hypocalcemia was diagnosed when the concentration of calcium corrected for albumin was less than 8mg/dL. For the replacement of calcium, the following protocol was followed: calcium >8mg/dL, no treatment; calcium 7–8mg/dL, oral calcium 1.5–2g/days; calcium <7mg/dL, iv calcium gluconate, 0.5–1.5mg/kg/h, adjusting the dosage according to symptoms and calcium levels, together with oral calcium 2–4g/day and calcitriol 0.5mcg/day.
The following clinical predictive factors were registered for each patient: age, sex, preoperative diagnosis, type of operation, number of preserved parathyroid glands, intrathoracic goiter and final histology. The patients were followed-up in our outpatient clinic. Calcium concentrations were determined one month, 6 months and one year after surgery.
Statistical AnalysisThe correlation between predictive factors and postoperative hypocalcemia was analyzed. Two patient groups were established: patients with hypocalcemia and patients with normal calcemia. The characteristics of each group were analyzed and compared. For categorical variables, the number of observations and percentages was determined. To compare results, the Chi-squared test was used; for continuous variables, a normal distribution was analyzed (Kolmogorov test); and the means and range (minimum and maximum) were reported. To compare the results, the Mann–Whitney and Kruskal–Wallis tests were used.
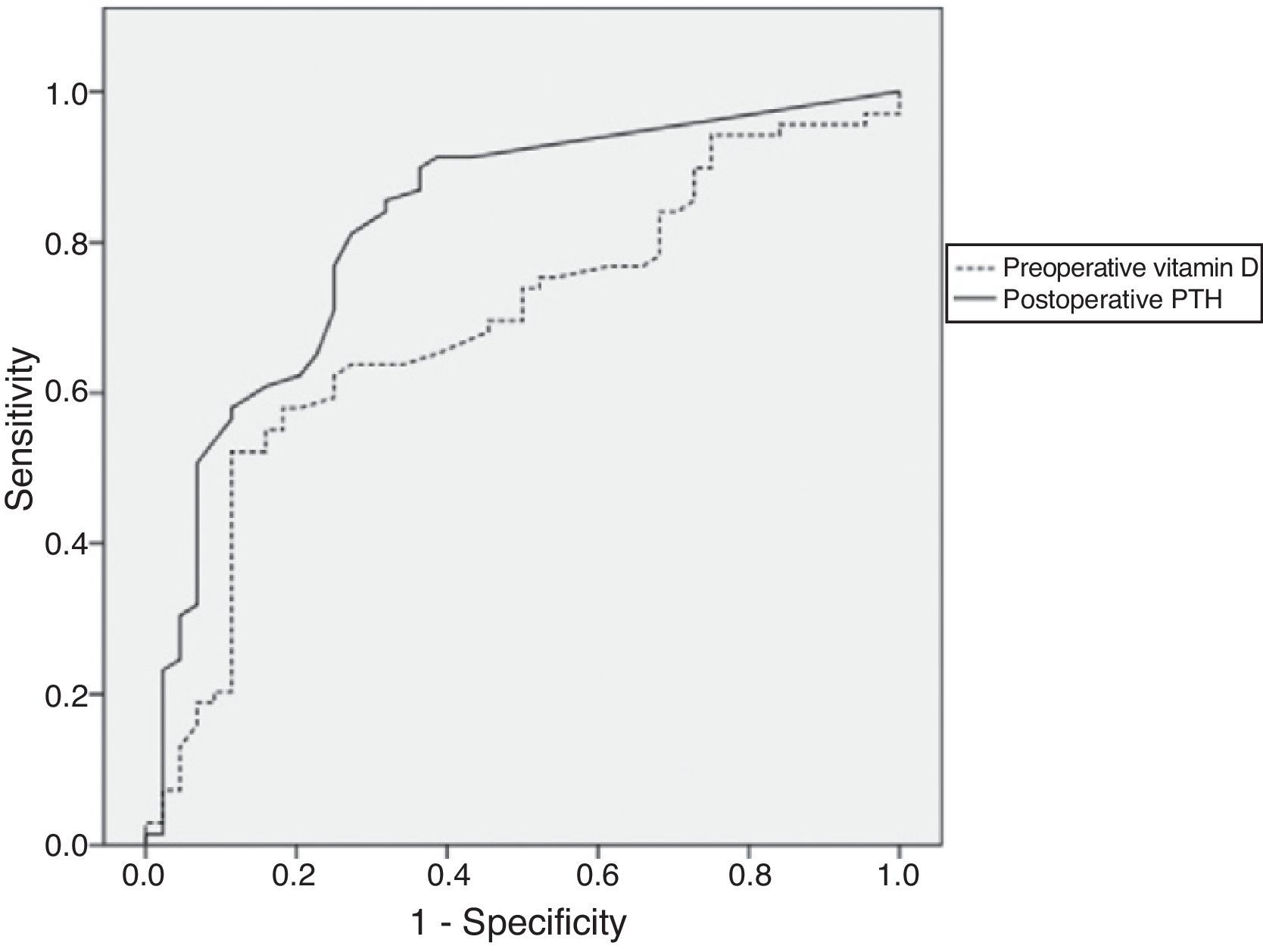
To study the value of postoperative PTH and preoperative vitamin D as predictors for hypocalcemia, we developed receiver operator characteristic (ROC) curves and calculated the areas under the curve. Sensitivity, specificity and predictive values were calculated. A logistic regression analysis was done to determine the effect of each prognostic factor on hypocalcemia. The effect of each variable was estimated with odds ratios (OR) and 95% confidence intervals. For the statistical analysis, SPSS 15.0 software for Windows (SPSS Inc., Chicago, IL, USA) was used.
ResultsOut of the 113 patients included in the study, 44 (38.9%) presented postoperative hypocalcemia. In 6 (5.3%) patients, the hypocalcemia was asymptomatic and in 38 (33.6%) it was symptomatic. In one patient (0.8%) PTH remained undetectable after one year (permanent hypoparathyroidism). The incidence of transitory vocal cord paralysis was 5.3% (6/113). No cases of permanent paralysis were recorded. The histopathology study detected the existence of previously undetected differentiated cancer in 11 patients (in 7 cases with a diameter <1cm and in 4 from 1 to 1.5cm).
The frequencies of PTH and vitamin D values did not follow a normal distribution. In the total population studied, the mean concentration of vitamin D was 20.4ng/mL (range: 4–60ng/mL). In the patients with normal postoperative calcemia, the concentrations of calcium, vitamin D and PTH were significantly higher than in those who developed hypocalcemia (Table 1). The distribution of frequencies of the clinical variables was similar between the 2 groups.
Characteristics of the Patient Groups According to Postoperative Calcemia.
| Normal calcemia(n=69) | Hypocalcemia(n=44) | P | |
| Age | 55 (20–77) | 52 (18–75) | .75a |
| Sex | |||
| Women (n=95) | 55 (57.9%) | 40 (42.1%) | .091b |
| Men (n=18) | 14 (77.3%) | 4 (22.2%) | .607b |
| Diagnosis | |||
| Multinodular goiter, n=95 | 58 (61%) | 37 (39%) | .001b |
| Basedow disease, n=18 | 11 (61.1%) | 7 (38.9%) | .447b |
| Preoperative vitamin D, ng/mL | 25.4 (4–60) | 16.4 (6.3–46.9) | .087a |
| Endothoracic goiter, n=20 | 13 (65%) | 7 (35%) | .609a |
| Serum creatinine, mg/dL | 0.99 (0.94–1.29) | 0.98 (0.69–1.24) | |
| N of parathyroid glands identified | 2 (0–4) | 2 (0–4) | |
| Postoperative calcium, mg/dL | 9 (8.2–9.5) | 7.7 (7–7.9) | .001a |
| Postoperative PTH, pg/mL | 25 (3–85) | 3 (3–78) | <.001a |
The values are expressed as means (range).
In 78 patients (69%), the concentration of vitamin D was lower than 30ng/mL, adopted as a normal limit. Among them, 39 (50%) developed postoperative hypocalcemia. Contrarily, out of the 35 patients with normal vitamin D, 5 (14.2%) presented hypocalcemia (P=.001) (Table 2). Furthermore, in the patients with normal vitamin D, the postoperative concentrations of PTH and calcium were significantly higher (Table 2).
Characteristics of the Groups of Patients According to the Preoperative Concentration of Vitamin D.
| Vitamin D>30ng/mL (n=35) | Vitamin D<30ng/mL (n=78) | P | |
| Postoperative calcemia postoperative, mg/dL | 8.9 (7.6–9.5) | 8.05 (7–9.5) | .001a |
| Frequency of hypocalcemia | 5 (14.2%) | 39 (50%) | .001b |
| Postoperative PTH, pg/mL | 24 (3–72) | 15 (3–85) | .02a |
| Age | 50 (28–73) | 55 (18–77) | .201a |
PTH, intact parathyroid hormone.
The values are expressed as means (range).
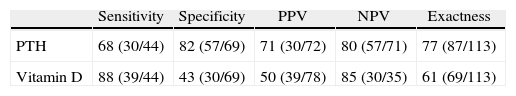
Fig. 1 presents the ROC curves that reflect the correlation between sensitivity and specificity for the detection of hypocalcemia. The area under the curve for PTH was 0.82 (95% CI: 0.741–0.904), which was higher than that registered for vitamin D (0.690) (95% CI: 0.590–0.790). The vitamin D value used as a cut-point for normal range (30ng/mL) correlated with the appearance of postoperative hypocalcemia: sensitivity 88%, specificity 43%, positive predictive value 50%, negative predictive value 85% and overall exactness 61% (Table 3). These same parameters for PTH were 68%, 82%, 71%, 80% and 77%, respectively.
Postoperative PTH and Preoperative Vitamin D Levels as Predictive Tests for Postoperative Hypocalcemia.
| Sensitivity | Specificity | PPV | NPV | Exactness | |
| PTH | 68 (30/44) | 82 (57/69) | 71 (30/72) | 80 (57/71) | 77 (87/113) |
| Vitamin D | 88 (39/44) | 43 (30/69) | 50 (39/78) | 85 (30/35) | 61 (69/113) |
NPV, negative predictive value; PPV, positive predictive value; PTH, intact parathyroid hormone.
The area under the ROC curve for PTH in patients with vitamin D levels below 30ng/mL was 0.783 (95% CI: 0.679–0.887), somewhat lower than that observed in patients with normal vitamin D: 0.9 (95% CI: 0.679–1.033).
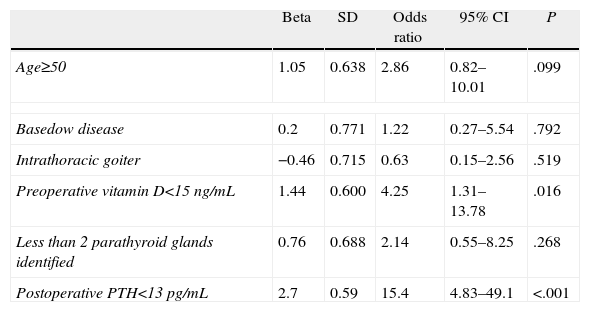
The logistic regression analysis showed that only vitamin D and PTH presented independent predictive value as indicators for high risk of postoperative hypocalcemia (Table 4). The OR associated with preoperative vitamin D<30ng/mL was 4.25 (95% CI: 1.31–13.78) (P=.016). In contrast, the OR associated with postoperative PTH<13pg/mL was higher: 15.4 (95% CI: 4.83–49.1) (P<.001).
Multivariate Analysis of the Risk Factors for Hypocalcemia After Total Thyroidectomy.
| Beta | SD | Odds ratio | 95% CI | P | |
| Age≥50 | 1.05 | 0.638 | 2.86 | 0.82–10.01 | .099 |
| Basedow disease | 0.2 | 0.771 | 1.22 | 0.27–5.54 | .792 |
| Intrathoracic goiter | −0.46 | 0.715 | 0.63 | 0.15–2.56 | .519 |
| Preoperative vitamin D<15ng/mL | 1.44 | 0.600 | 4.25 | 1.31–13.78 | .016 |
| Less than 2 parathyroid glands identified | 0.76 | 0.688 | 2.14 | 0.55–8.25 | .268 |
| Postoperative PTH<13pg/mL | 2.7 | 0.59 | 15.4 | 4.83–49.1 | <.001 |
95% CI, 95% confidence interval; PTH, intact parathyroid hormone; SD, standard deviation.
In recent years, it has been observed that vitamin D deficiency has implications in several musculoskeletal and cardiovascular pathological processes, neoplasms, defective lipid metabolism and diabetes.17–21 Nevertheless, more information is still needed because it is not known whether this is just an epiphenomenon or whether there is a causal relationship. The range of normal values provided by the laboratories is 40–100ng/mL. Recent studies have questioned the use of these reference values since the vitamin D levels necessary to avoid the appearance of disease seem to be lower. It has been observed that persistent vitamin D concentrations below 18ng/mL constitute a risk factor for cardiovascular disease19 and that 30ng/mL is a risk factor for developing non-vertebral bone fractures.20 It has also been reported that levels higher than 30ng/mL are needed to prevent secondary hyperparathyroidism.13,14,17
In our study, a high percentage of patients presented vitamin D deficiency. Sixty-nine percent of cases had preoperative concentrations <30ng/mL, which is considered a normal limit. The results coincide with previous publications.9–12 It seems that this frequent vitamin D deficiency is not specific to thyroid disease but is instead a reflection of its high prevalence in the general population, especially in women and in those over the age of 60.21 In a Spanish publication, only 30% of a general population sample presented levels higher than 18ng/mL.22 Older age is associated with alterations in the metabolism of vitamin D: lower cutaneous concentrations of 7-dehydrocholesterol (which is converted into previtamin D3 by ultraviolet radiation), reduced renal 1-alpha hydroxylase activity and decreased intestinal absorption of calcium.23 In addition, it is usually accompanied by poor nutrition and less exposure to sunlight.17
According to our results, the appearance of postoperative hypocalcemia was more frequent in patients with vitamin D deficiency. These findings coincide with those obtained in previous studies done in patients with multinodular goiter.9–12 In the study by Erbil et al.,9 83% of the patients with vitamin D lower than 14ng/mL developed symptomatic hypocalcemia versus 25% of patients with normal levels. In another study performed in surgically treated women by Basedow,24 symptomatic hypocalcemia was more frequent in patients with vitamin D<10ng/mL. In contrast, Chia et al.25 found no correlation between vitamin D concentrations and calcemia. In this study, however, the population was heterogeneous as it included diverse thyroid processes, parathyroid adenomas and hyperplasia, and the surgical technique was not uniform.
In our study, the efficiency of postoperative PTH levels for predicting the appearance of hypocalcemia was superior to using vitamin D. In addition, the ROC curve (which reflects the sensitivity/specificity balance) for PTH (OR=0.80) was higher than that registered for vitamin D (OR=0.698). These data demonstrate that vitamin D possesses a limited value as a predictor for the appearance of hypocalcemia that is lower than that of PTH. Few previous publications have determined both vitamin D and PTH in a parallel manner. In the study by Erbil et al.,9 vitamin D was the prognostic factor that best correlated with postoperative calcemia, with an OR of 558 (95% CI: 27–11291), which is higher than that reached with PTH (OR=16; 95% CI: 1.8–143).
In the studies by Kirby-Bott et al.11 and Sam et al.,12 the vitamin D levels conditioned the predictive value of PTH. In these reports, PTH only correlated with postoperative calcemia in patients with vitamin D levels over 15ng/mL. The patients with vitamin D insufficiency presented higher pre- and postoperative PTH concentrations due to the secondary hyperparathyroidism derived from the vitamin D deficiency. In our study, postoperative PTH levels correlated with the appearance of hypocalcemia regardless of the level of vitamin D, although the area of the ROC curve was higher in the patients with normal vitamin D levels.
The regulation of PTH secretion by the parathyroid glands is a complex mechanism that does not only depend on calcium and phosphate levels.17,26 Vitamin D is an important regulator of PTH secretion and the proliferation of parathyroid cells. The parathyroid glands have vitamin D receptors (VDR) and calcium receptors that function synchronically as a system of negative feedback on the release of PTH.13,14,27 If there is vitamin D deficiency, the maintenance of calcium levels mainly depends on PTH. Patients with vitamin D deficiency absorb less calcium in the intestine, which makes them dependent on bone and renal reabsorption mediated by PTH.26 Any circumstance that damages the parathyroid glands, such as surgical manipulation, temporarily reduces the secretion of PTH and predisposes the patient to hypocalcemia.
In the multivariate analysis, the prognostic factor that was associated with a higher risk of hypocalcemia was PTH. The risk attributable to the presence of PTH<13pg/mL was 15.4. Vitamin D<30ng/mL also presented an independent predictive value, although with a lower OR (4.25). Clinical factors showed no statistically significant relation, possibly due to the fact that the effect of the number of parathyroid glands preserved and the presence of intrathoracic goiter was already reflected in the PTH concentration. Basedow disease was not shown to have an independent effect, possibly due to the smaller number of patients with this disease. The data indicate that the most important factor for preventing the appearance of postoperative hypocalcemia is a surgical technique that preserves parathyroid gland function, which is represented by the postoperative PTH concentration. But, even if the surgical technique is correct, hypocalcemia may appear if there is vitamin D deficiency. The predictive information that vitamin D provides complements the PTH information because each predicts a risk with a different physiopathological origin.
The advantage that vitamin D may have as a prognostic factor for postoperative hypocalcemia is that, as it is assessed in the preoperative period, any deficiencies that may exist before the surgical intervention can be corrected. It seems reasonable that the minimum desirable preoperative level of vitamin D should be 30ng/mL. Future prospective studies should investigate whether the correction of a vitamin D deficiency is accompanied by a lower incidence of hypocalcemia. It would have been interesting to have had available for this study a larger number of patients with Basedow disease and to have been able to analyze what occurred in each disease.
Vitamin D deficiency is a risk factor for the appearance of postoperative hypocalcemia after TT due to benign goiter. The concentration of vitamin D provides independent predictive information that complements the information provided by PTH.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Díez M, Vera C, Ratia T, Diego L, Mendoza F, Guillamot P, et al. Efecto de la deficiencia de vitamina D sobre la hipocalcemia tras tiroidectomía total por bocio benigno. Cir Esp. 2013;91:250–256.