The surgical strategy for treating intraductal papillary mucinous neoplasm (IPNM) of the peripheral branches continues to be controversial.1 The extension of the surgical resection is still under debate, especially in patients with non-invasive lesions.2 In these patients, the objective is to preserve as much of the remaining parenchyma as possible.
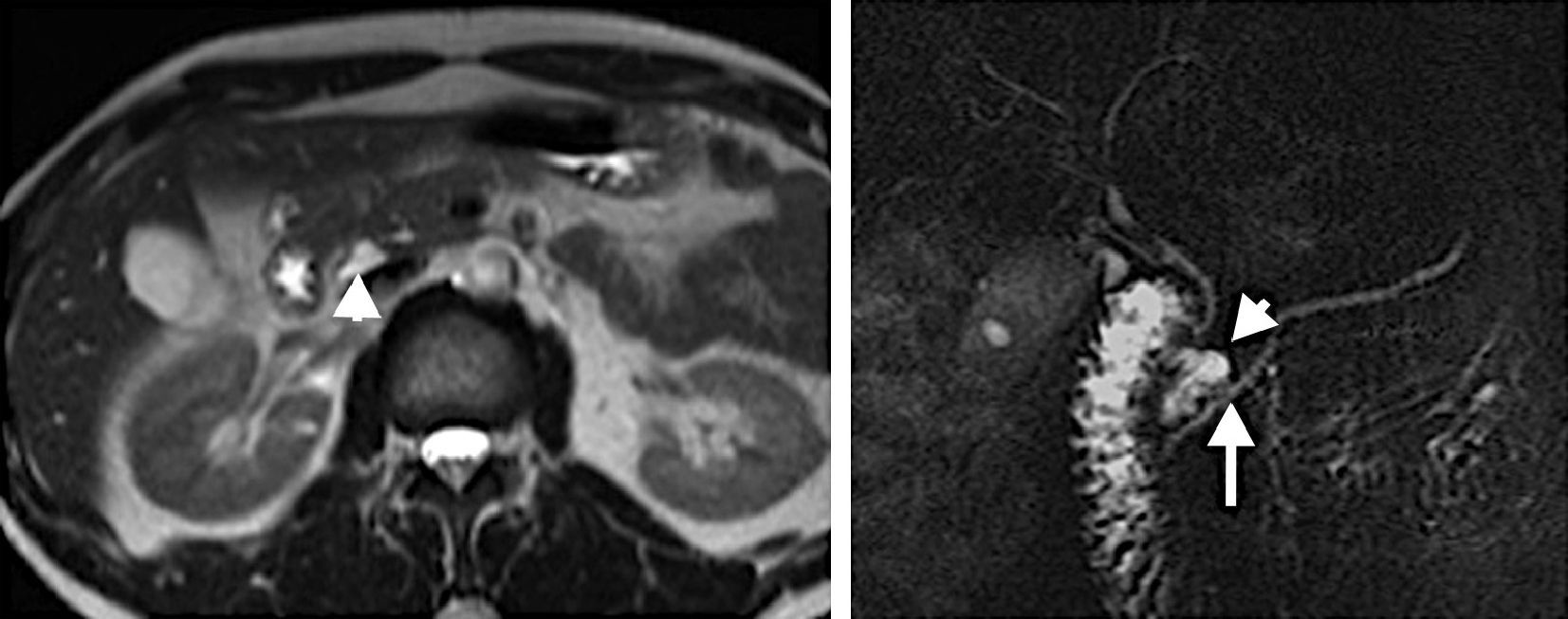
We present the case of a 39-year-old man with a history of recurring episodes of acute pancreatitis. Multislice computed tomography (MSCT) and magnetic resonance cholangiopancreatography (MRCP) showed a pancreatic cyst located in the posterior region of the head of the pancreas, which probably communicated with the main pancreatic duct (Fig. 1). The size of the tumor was 19mm. Serum levels of CA 19.9 and CEA were normal. The preoperative evaluation was completed with endoscopic ultrasound, which ruled out the presence of other nodules. With the diagnosis of IPNM of the peripheral branches, we decided to resect the lesion.
The patient was taken to the operating room with the intention of performing a laparoscopic Whipple procedure. An extended Kocher maneuver was done with complete mobilization of the head of the pancreas. Intraoperative ultrasound enabled us to precisely locate the lesion, which was protruding from the posterior side. At that time, we decided to perform enucleation with preservation of the pancreatic parenchyma and the duodenum.
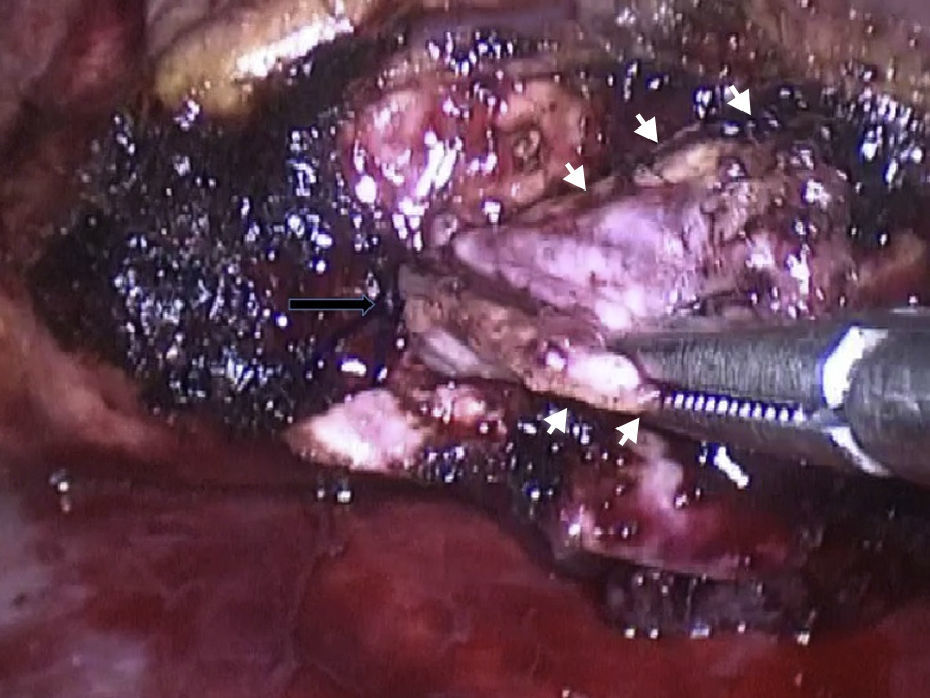
The cyst was dissected with an electroscalpel, and the communicating duct was identified and ligated while preserving the main pancreatic duct and enucleating the tumor (Fig. 2). The frozen histology sections of the cyst showed low-grade dysplasia. The patient recovered without complications and was discharged from the hospital on the fifth day post-op. The definitive pathology report determined the lesion to be a borderline IPNM. The patient has been symptom-free after 4 months of follow-up.
The extension of the pancreatic resection for the surgical treatment of peripheral branch IPNM continues to be a topic of debate.3 In patients with non-invasive tumors, the long-term results in terms of endocrine and exocrine pancreatic insufficiency should be taken into special consideration.4
Conservative procedures seem to be an alternative to major pancreatic resections in this type of disease. Central and distal spleen-preserving pancreatectomies have become common treatments in cystic tumors and IPNM of peripheral branches without suspected malignancy.5 But preservation of the pancreatic parenchyma can be difficult for lesions located in the head of the pancreas or in the uncinate process, for which pancreaticoduodenectomy continues to be the traditional approach. For this reason, enucleation can be useful in these difficult locations.
Little has been published in the international literature with regards to the enucleation of benign peripheral branch IPNM. Hwang presented 14 patients with small IPNM (<3cm) in the head of the pancreas. Four of them were enucleated and 10 patients underwent pancreaticoduodenectomy. A significant decrease was seen in surgical time, as well as in blood loss in the enucleation group, with no differences in disease recurrence between the 2 groups.6
Turrini has also demonstrated shorter operative time and less blood loss in patients with IPNM of the peripheral branches that were enucleated when compared with those who underwent pancreaticoduodenectomy. Although it is not statistically significant, the enucleated patients in this series tend to present a greater incidence of postoperative pancreatic fistulas. Nonetheless, other studies have shown that grade B or C pancreatic fistulas are uncommon after enucleation.7,8This group proposes certain criteria for selecting patients with IPNM who would be candidates for enucleation:
- 1.
No previous pancreatic surgery.
- 2.
IPNM of the peripheral branches located in the head of the pancreas or uncinate process.
- 3.
No dilation of the main pancreatic duct.
- 4.
No mural nodules or thickening of the cystic wall.
- 5.
The main pancreatic duct can be preserved.
In order to avoid a pancreatic fistula, the identification and ligation of the communicating duct is essential. Intraoperative ultrasound is necessary for this purpose as it aids in identifying and preserving the integrity of the main pancreatic duct.
The largest series of IPNM treated with enucleation was published by Blanc. This series reported 26 cases that had been treated with open enucleation for patients with IPNM of peripheral branches. When performing enucleation, special attention should be paid to the intra-surgical evaluation of the resection margins.9 If the pathologist detects an invasive or carcinoma in situ, the resection should be completed with oncologic criteria.10
The laparoscopic approach is an option for performing this surgery. To our knowledge, there are no publications that mention laparoscopic enucleation of an IPNM of the peripheral branches. This approach could be beneficial for these patients, since it adds the benefits of minimally invasive surgery to the preservation of the pancreatic parenchyma.
Please cite this article as: Mazza O, de Santibanes M, Cristiano A, Pekolj J, de Santibañes E. Enucleación laparoscópica de una neoplasia intraductal papilar mucinosa de ramos periféricos localizada en la cabeza del páncreas. Una nueva alternativa. Cir Esp. 2014;92:291–293.