The liver is the most common location of intraabdominal abscesses, accounting for 48% of these lesions. The main predisposing factors for their occurrence are: diabetes mellitus, immunosuppression, cholelithiasis, biliary tract infections, acute pancreatitis or liver transplantation. Hepatic actinomycosis is a rare clinical entity that is difficult to diagnose and requires complex treatment.1 There are very few cases of hepatic abscesses caused by Actinomyces spp. reported in the literature,1–3 and the most common locations are the cervicofacial area (50%–90%) and the thoracic cavity (15%–45%).4
We present the case of a 66-year-old male in treatment for diabetes, with good glycemic and lipemic control. He came to the emergency room for abdominal pain in the right hypochondrium that had been progressing over the course of a week. Total bilirubin was 2.69¿g/dL, gamma-glutamyl-transferase 1450¿U/L, lactate dehydrogenase 186¿U/L and alkaline phosphatase 211¿U/l. Abdominal ultrasound demonstrated cholelithiasis with no signs of cholecystitis or dilatation of the intrahepatic biliary tract. As it was impossible to rule out alterations in the extrahepatic bile duct due to the presence of gas, endoscopic ultrasound was conducted, which showed images compatible with choledocholithiasis. Therefore, endoscopic retrograde cholangiopancreatography (ERCP) was performed, resulting in the extraction of a small stone. The patient presented acute pancreatitis after the procedure but responded well to conservative medical treatment.
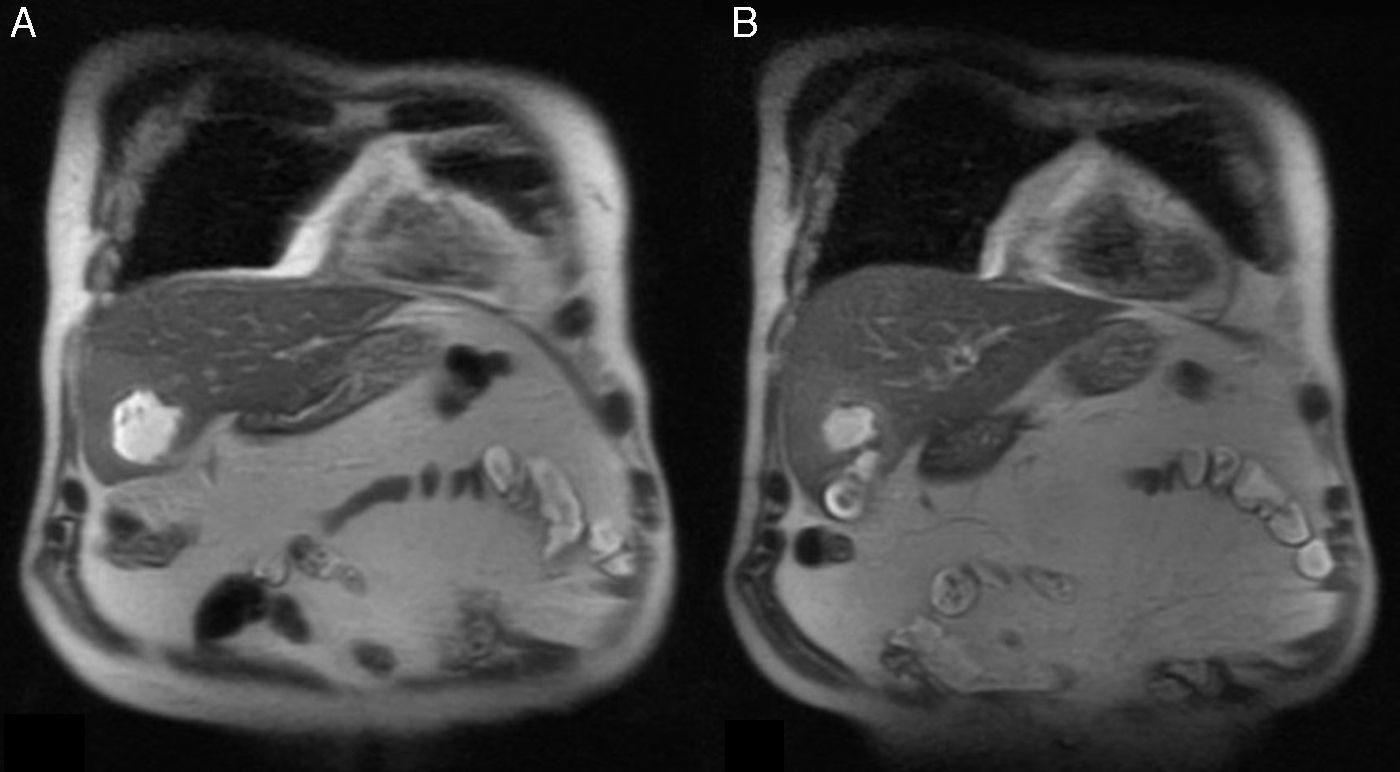
The follow-up computed tomography (CT) revealed 2 peripancreatic collections secondary to post-ERCP pancreatitis. Two months later, magnetic resonance cholangiopancreatography was performed prior to scheduled cholecystectomy, at which time an abscess was observed in hepatic segment V, measuring 4.4cm×5cm, that had not been seen on the previous CT scan; meanwhile, the peripancreatic collections had disappeared (Fig. 1). With these findings, we decided to hospitalize the patient, performing percutaneous drainage of the abscess and administering empirical intravenous antibiotic therapy with piperacillin/tazobactam. The cultures showed growth of Streptococcus anginosus and Staphylococcus epidermidis. A follow-up ultrasound performed 3 days after percutaneous drainage demonstrated a decrease in the size of the perivesical collection. The patient was discharged with oral antibiotic therapy, including ciprofloxacin and linezolid for 7 days. Subsequently, after obtaining the complete antibiogram of the culture performed and the finding of Actinomyces naeslundii, the patient was advised of the need to complete antibiotic treatment with intravenous ertapenem for 4 weeks more on an outpatient basis.
The patient remained asymptomatic over the course of 4 months, during which imaging tests demonstrated the resolution of the hepatic abscess, until a laparoscopic cholecystectomy was performed, which was conducted without incident. The pathology study showed a gallbladder with xanthogranulomatous areas, signs of chronic cholecystitis and adenomyomatous hyperplasia. At the same time, a sample of the gallbladder contents was sent for culture, which was negative.
Actinomycosis is a chronic granulomatous infection caused by Gram-positive bacteria that make up the oropharyngeal, digestive and female genitourinary tract flora.1,2 Intra-abdominal infection is usually polymicrobial in nature, and Actinomyces israelii is the most frequently isolated species in cultures from intra-abdominal organs.3 It is an uncommon cause of hepatic abscesses, and it is usually secondary to processes involving disruption of the digestive tract mucosa, such as acute perforated appendicitis, gastrointestinal tumors or traumatic procedures (biopsies or surgeries).1,3,5 There have been some thirty case reports,2 in which the right hepatic lobe is the most frequent location and solitary lesions are the most common form of presentation. The finding of Actinomyces naeslundii in hepatic abscesses is extremely rare, and only one case has been previously reported.1
The clinical diagnosis of this entity is complex because it presents nonspecific symptoms (low-grade fever, constitutional syndrome, pain in the right hypochondrium, etc.) and due to its inherent nature that mimics other gastrointestinal pathologies. In the differential diagnosis, it is important to consider the possible existence of hydatid cysts, tuberculosis and even neoplasms, due to their tendency to form masses and invade neighboring organs.3,5–8 Liver resections are sometimes performed if it is not possible to correctly identify the infection.3,8 For adequate diagnosis, imaging tests (CT, MRI or ultrasound) are recommended, accompanied by drainage of the collection to obtain material for microbiological and cytological examination prior to surgery.2,3
Definitive treatment involves correct drainage of the abscess and a long cycle of antibiotics, including penicillin, amoxicillin, ampicillin or clindamycin, for a period that varies from 3 to 12 months, depending on the patient's progress.2 Occasionally, the patient's course may be torpid in spite of the treatment, and it can be necessary to repeat the drainage of any recurrences that may arise after the initial improvement, and surgical intervention may even become necessary.4
In short, although liver abscesses are considered common, infections by Actinomyces are atypical. The diagnosis is usually made incidentally because its nature mimics other processes such as neoplasms, and the specific treatment required is often prolonged.
FundingThe authors have received no funding for the completion of this article.
Please cite this article as: Correa Bonito A, Mora-Guzmán I, García-Sanz I, di Martino M, Martín-Pérez E. Absceso hepático post-colangiopancreatografía retrógrada endoscópica con presencia de Actinomyces naeslundii. Cir Esp. 2017;95:51–52.