Infections caused by Listeria monocytogenes, a mobile gram positive bacillus, are usually associated with immunosuppresed states. Most cases present as meningitis or primary bacteraemia. Other types of presentations are extremely rare.
We report the case of a 57 year old man, with a prior history of type 2 diabetes mellitus treated with oral antidiabetic medication and cholecystectomy in 1990. He presented a 3-month history of general malaise and fever of up to 40°. He consulted 2 weeks after the start of the symptoms, due to persistence of malaise, intermittent fever, associated with myalgias, anorexia and weight loss. The first time he came to the emergency department he was treated with endovenous analgesia and was discharged. Subsequently, he consulted three different doctors and was finally admitted to complete the study of his symptoms. A CT scan of the abdomen and pelvis revealed 2 hypodense hepatic lesions of 25mm in segment VIII and another two in segments VII and VI of 52 and 59mm, respectively, displacing the portal vessels. In the mid third of the right kidney a solid image of 25mm maximum diameter was observed, compatible with a renal cell carcinoma. He was then transferred to the Hospital Militar in Santiago de Chile for management.
He was initially evaluated by urology, and a staging study of renal cancer was started. Blood tests revealed leukocytes 7.4K/μL, neutrophils 11%, ESR 75mm/h, alkaline phosphatase 195U/L, AST 117U/L.
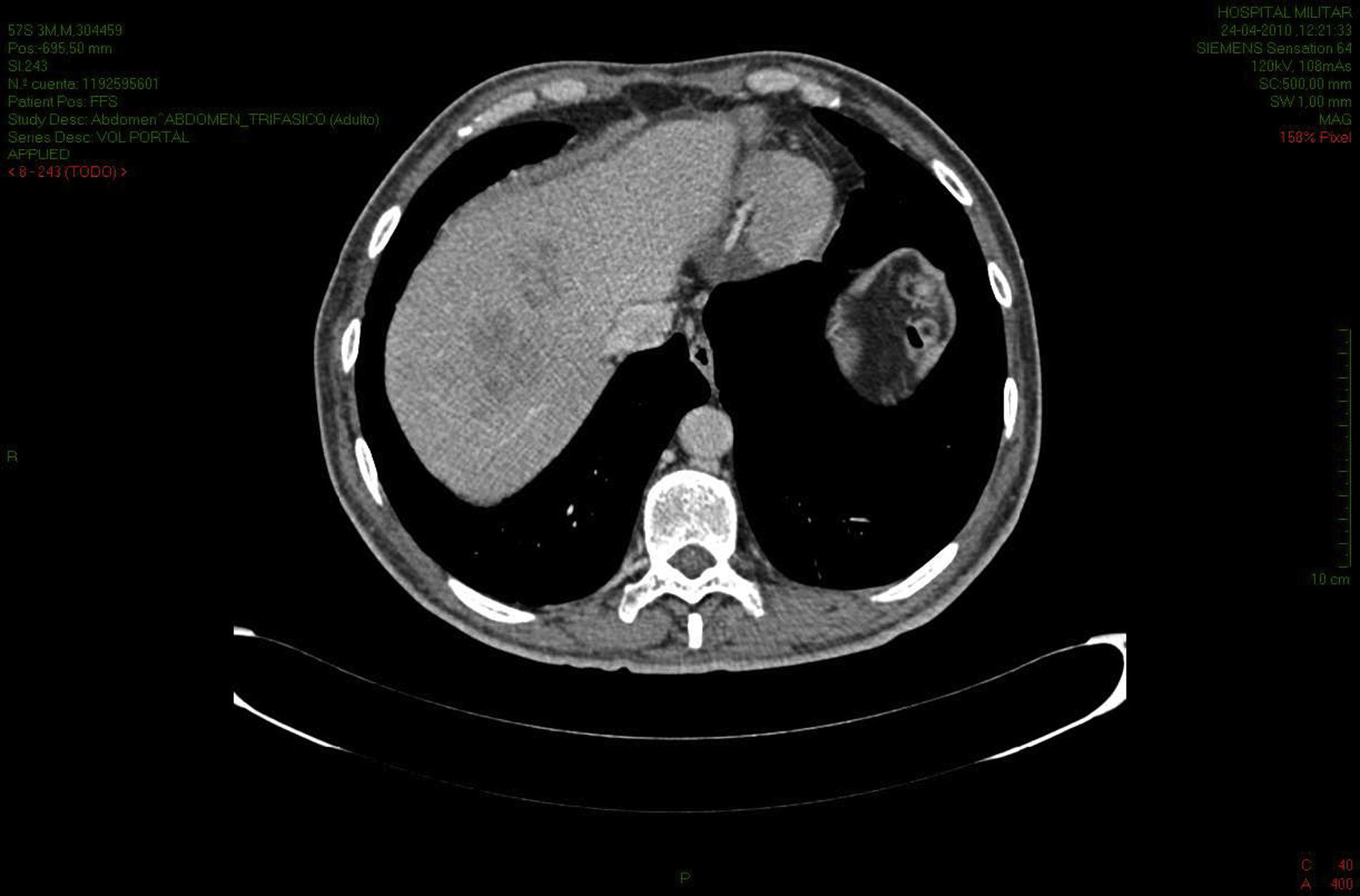
A CT scan revealed a heterogeneous liver with the presence of ill-defined hypodense focal lesions in the VII y VIII segments (8cm), caudate (2.5cm) and VI and VII (8cm), this last lesion presented a focal area of 9mm that was more hypointense (Fig. 1). In the anterior aspect of the middle third of the right kidney a solid nodule of hypodense structure was revealed with a 2.7cm diameter. The patient was evaluated by a digestive surgeon who decided hospitalization and treatment. Serologies for viral hepatitis were negative, blood cultures were negative, alfa fetoprotein and carcinoembryonic antigen were negative. Empiric antibiotic treatment was started using intravenous 2g ceftriaxone/24h and 500mg metronidazol/8h. A CT guided fine-needle aspiration of a liver lesion was performed, obtaining 15ml of foul smelling purulent fluid. Aerobic and anaerobic cultures were performed, which were positive for L. monocytogenes. Antibiotic treatment was changed to ampicillin 1.000mg and sulbactam 500mg, 2 vials every 6h for 3 days, ampicillin 3g every 6h for 16 days. Ten days after staring treatment a control CT scan was performed, and a partial regression of the focal lesions was seen, with the appearance of a subcapsular collection of 4cm diameter in segment VI; a percutaneous drainage was performed and maintained for 5 days. Treatment was completed with oral amoxicillin 1g every 8h for four weeks. The patient responded favourable, without fever or symptoms, and the lesions progressively diminished on control scans (Fig. 2).
Liver infections caused by L. monocytogenes are exceptionally rare. Patients with this condition usually have comorbidities that cause a state of chronic immunosuppression.
Different mechanisms for this infection have been proposed: the arrival of the bacteria to the hepatic circulation after a bacteriemia, or a bacterial translocation to the venous portal system after enteric colonization.1 Clinical manifestations of this infection can imitate a neoplastic condition, and the diagnosis is often delayed. In previously described cases and in the present case, without extrahepatic manifestations, the clinical scenario was a group of non-specific symptoms, malaise, anorexia, weight loss, intermittent fever and night sweats, with over a week duration.2
There are three different patterns of liver infection: solitary abscess, multiple abscesses and hepatitis. In the literature, the case reports of solitary abscesses were all in patients with a prior history of diabetes mellitus. Patients reported with multiple abscesses have more severe clinical presentations, with systemic symptoms and extrahepatic manifestations. In patients with hepatitis, of the 3 case reports, 2 also presented meningeal manifestations.3–5 The cornerstone of treatment is prolonged antibiotic therapy (over 2 weeks), initially endovenous; however, the duration of treatment has not been clearly established. It is also not known if percutaneous drainage can reduce the time to resolution of the infection.1,2
Please cite this article as: Onetto C, Ríos H, Domenech A, Schiappacasse G, Estay C. Absceso hepático por Listeria monocytogenes. Cir Esp. 2013;94:267–269.