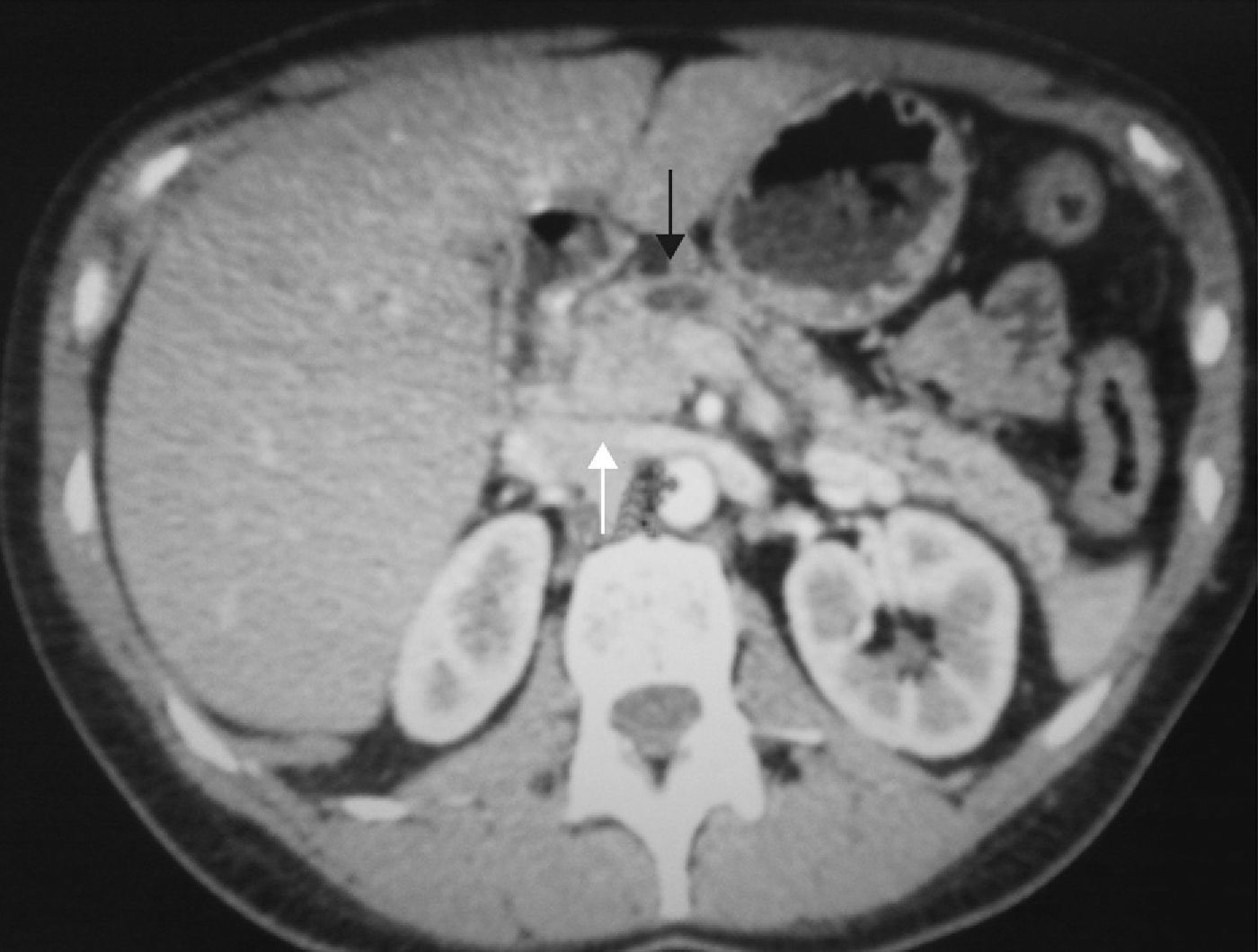
Case report: A 43-year-old woman, without any prior medical history, consulted for epigastric abdominal pain and nausea of 9-month duration. Blood tests revealed an amylase of 183U/L. An abdominal ultrasound and abdominopelvic CT revealed a mass in the pancreatic head. The proximal segment of the superior mesenteric vein (of approximately 3cm length) was infiltrated and thrombosed and enlarged peripancreatic lymph nodes were seen (Fig. 1). An echoendoscopy was used to perform a biopsy of the mass that was positive for malignancy but was unable to define the histology; the suspicion was neuroendocrine tumor. An MRI confirmed the pancreatic mass, observing that it surrounded the superior mesenteric vein. An octreoscan showed uptake in the epigastric area.
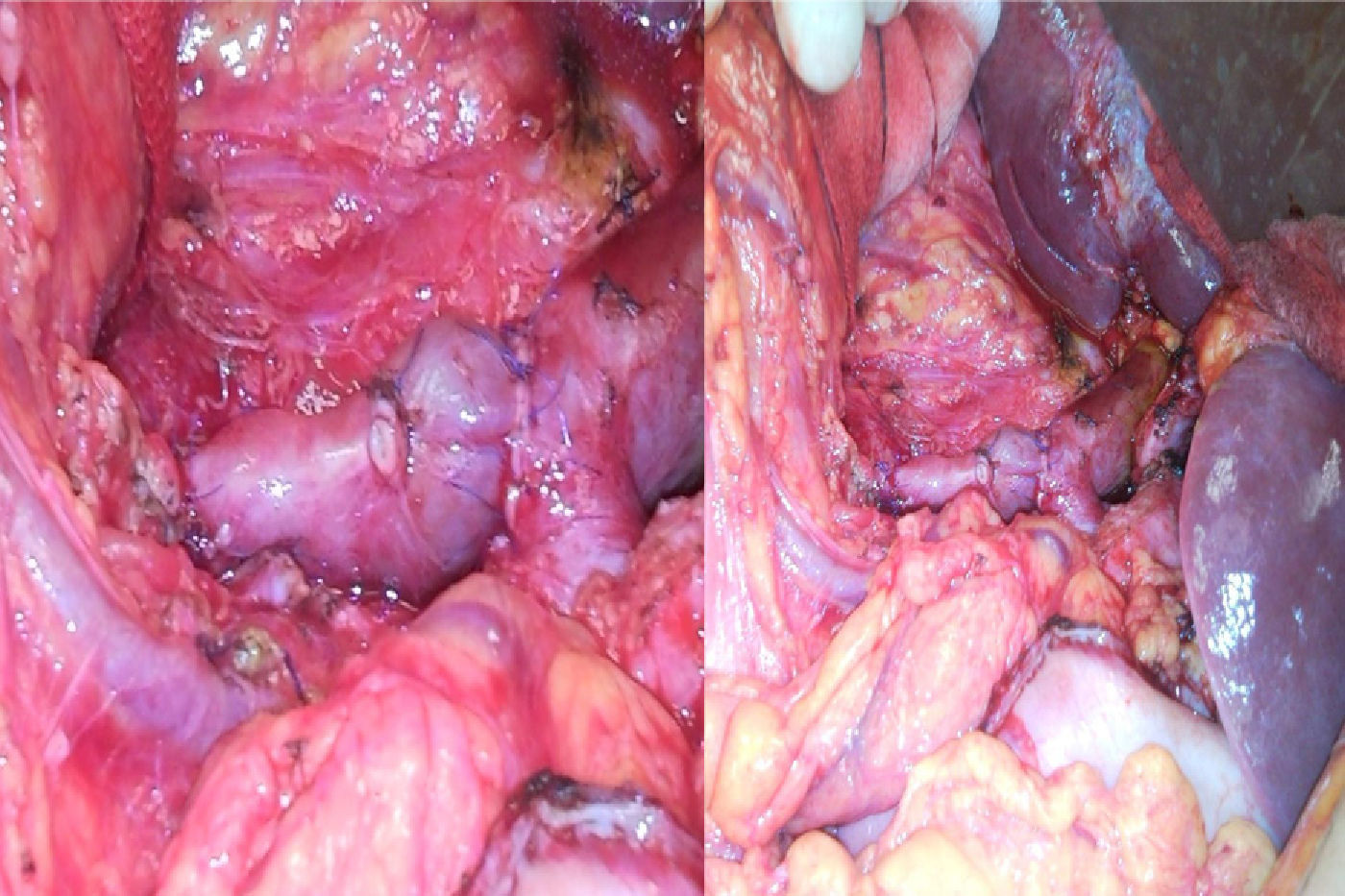
Surgery was scheduled and a tumor in the pancreatic head infiltrating the superior mesenteric vein was observed. A Whipple's cephalic duodenopancreatectomy was performed with an en bloc resection of the superior mesenteric vein and reconstruction by interposition of the previously resected left renal vein (Fig. 2).
The patient had an uneventful postoperative course. On the 6th postoperative day and control angio-CT and Doppler ultrasound were performed and permeability of the renal arteries and superior mesenteric arteries were checked. She was discharged on postoperative day 11 asymptomatic and tolerating an oral diet.
The pathology study revealed an endocrine tumor of 3.5cm×3.5cm. The resection margins were free of neoplasia and six isolated lymph nodes were also free of neoplasia. A tumoral thrombus was found in the superior mesenteric vein with histology compatible with a well-differentiated trabecular tumor.
One month and a half after surgery the patient continues well, and a control CT scan shows permeability of the superior mesenteric vein and left kidney of a normal size and morphology. A follow-up blood test revealed chromogranine 115.1. All other parameters were normal.
A complete resection is the only potentially curative treatment for neuroendocrine tumors. Frequently these tumors are malignant, and local invasion at the time of diagnosis can prevent a radical removal of the tumor; in these cases a cytoreductive approach can be proposed. An aggressive surgical approach in cases of advanced disease can prolong survival, and it is therefore justified, including, if necessary, resection of adjacent organs (stomach, colon, kidneys, adrenal glands) and/or main vessels.5–7
The reconstruction of the resected vein can be performed by a primary anastomosis 8 in approximately 88% of cases) or by using grafts, both synthetic or autologous (splenic, jugular, gonadal, iliac, femoral, saphenous or umbilical veins). The reconstruction with an autologous venous graft should be considered only in selected cases: when the resection of the superior mesenteric-portal vein is larger than 3cm, when the portal-superior mesenteric confluence is involved or when it is not possible to perform a tension-free anastomosis.4
Reconstruction using an autologous left renal vein graft is a technically possible, simple and durable option.1–3 The renal vein is easily exposed during hepatobiliary operations and is even more accessible during duodenopancreatectomies, without the need to extend the incision. It provides sufficient length and has a similar calibre to the SMV.1,2 The renal vein has many collateral veins and can be ligated without compromising the venous drainage of the kidney. Preservation of the gonadal and azygos veins is essential during the resection of the left renal vein. Therefore, the renal vein should be resected from the junction of the vena cava and the left renal vein to the distal portion just distal to the azygos vein.1,2,8 The collateral vessels will drain the venous return of the left kidney and will preserve its function.2
To prevent graft occlusion, it is important to select an autologous renal vein with an adequate size and length.2 The graft should not be redundant or left with tension. An intraoperative and postoperative Doppler should be performed to evaluate its permeability.1 Anticoagulant therapy is also necessary.2
In conclusion, an aggressive surgery with major vascular resection is justified in selected patients with pancreatic cancer,3 in whom a segmental resection can be performed safely without an increase in morbidity or mortality rates when compared to a standard duodenopancreatectomy1,4 the use of an autologous graft of left renal vein is a feasible and reproducible technique with good long-term results.3
Please cite this article as: Markinez Gordobil I, Ruiz Montesinos I, Arteaga Martín X, Medrano Gómez MÁ, Beguiristain Gómez A. Duodenopancreatectomía cefálica con resección de vena mesentérica superior y reconstrucción mediante interposición de vena renal autóloga. Cir Esp. 2013;94:269–271.