Laparoscopic adjustable gastric banding (LAGB) is a safe and reversible procedure that entails low mortality and morbidity (approximately 0.05% and 11.3%, respectively).1 Even so, it has a high readmission and revision surgery rate of 52%.1 Late-onset postoperative complications are frequent and are probably not completely documented. Erosion and migration of gastric bands have an incidence of 0.6%–3%.1 We present a rare case of gastric band erosion through the stomach and later migration towards the ileum, while causing several bowel perforations.
The patient is a 51-year-old woman with a history of morbid obesity who had undergone a LAGB procedure one year before and had lost 25kg with 2 adjustments. She had sought treatment at the emergency room of another hospital due to diffuse abdominal pain and bilious vomiting. Analyses showed amylase 4000mg/dL and lipase 1100mg/dL; the patient was diagnosed with acute pancreatitis, which was classified as Balthazar B on computed tomography (CT) scan of the abdomen and pelvis with oral and intravenous (iv) contrast. The patient was immediately treated with NPO, intravenous hydration and analgesia; partial response was observed, but the abdominal pain and vomiting continued. An upper gastrointestinal series demonstrated a herniated fundus, and the gastric band was not visualised. She was finally transferred to our centre.
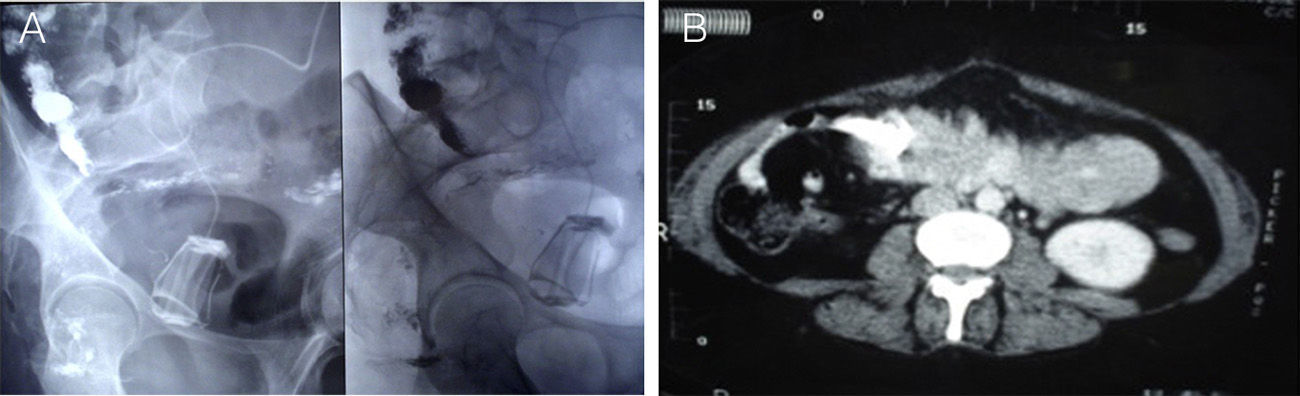
The patient continued to have abdominal pain, with no peritoneal irritation. Amylase and lipase levels were normal, but C-reactive protein was 21mg/L and leukocytes 13200/mm3. Upper gastrointestinal endoscopy detected a large ulcerated lesion with a foreign object in the area of the fundus and proximal antrum, which was the connector tube of the gastric band. Under fluoroscopy, contrast medium was injected into the pouch, which showed evidence of migration of the band to the right iliac fossa. Another abdominal/pelvic CT scan with contrast revealed the intraluminal position of the band (Fig. 1).
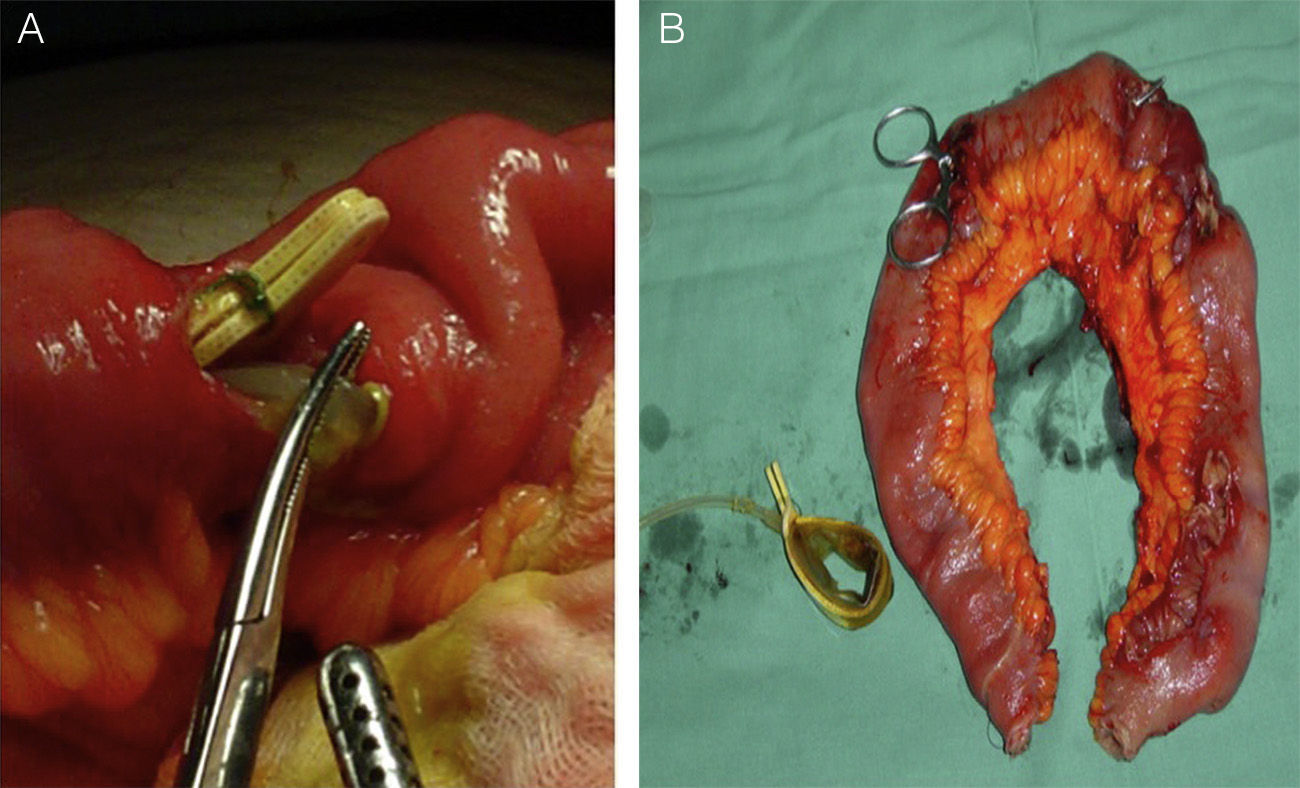
Surgery was indicated, so we carried out exploratory laparoscopy, which revealed the connector tube penetrating the gastric wall. The gastric band, however, could not be located, so the procedure was converted to open surgery. While exploring the cavity, multiple small bowel perforations were detected and the band was finally found 20cm from the ileocecal valve. We resected 40cm of the ileum, which was reconstructed with an end-to-end anastomosis (Fig. 2). Postoperative recovery was uneventful.
Long-term complications of gastric bands include port and connector problems, reflux, pouch dilation, prolapse, oesophageal dilatation and erosion. These often lead to revision surgeries that result in the withdrawal of the band and patient rejection of the technique.
Band erosion and intragastric migration are feared complications that persist as long as the band is installed. Proposed causes are related to subclinical gastric lesions at the time of placement, overly tight closure, elevated internal pressure after the ingestion of very large food quantities, and abnormal reaction of the tissue in contact with the prosthesis.2
In the literature, there are 8 case reports of band migration towards the small bowel, one of which presented perforations.2–9 There have also been cases in which the connector tube becomes disconnected and perforates the intestinal wall from the outside.10 Clinically, these patients can present symptoms compatible with intestinal obstruction, port infection or failure to lose weight.3–8 As the perforations are slow to develop, they normally do not present peritonitis, which allows the chronic inflammatory reaction to isolate them. In our case, it is interesting that the patient had pancreatitis previously, which seems to have been circumstantial.
Diagnosis is complex, and a high rate of suspicion is necessary. Persistent infection of the port site can be the first manifestation. CT scan with iv contrast should be the diagnostic technique of choice as it is able to more precisely identify the location of the band and determine its repercussions.4 Fluoroscopy, on the other hand, is simple to do and detects the migration of the band, while upper gastrointestinal endoscopy can be therapeutic for withdrawal of the band when possible.3
Treatment will depend on symptoms and degree of band migration. If more than 50% of the band's circumference is within the stomach, endoscopic extraction can be attempted, which is less invasive and causes less morbidity.2 In cases where it has migrated towards the small bowel or further and is associated with perforations, an open approach is required. The withdrawal of the band followed by immediate reinstallation is not recommended because of the high rates of failure and risk.
Please cite this article as: Oppliger F, Ríos H, Manríquez L. Migración y perforación de una banda gástrica en el intestino delgado. Cir Esp. 2015;93:601–603.