A temporary diverting ileostomy is frequently used to reduce the consequences of a distal anastomotic leakage after total mesorectal excision in rectal cancer surgery. This surgical technique is associated with high morbidity and a not negligible mortality. The aim of this study is to evaluate the morbidity and mortality rate associated with an ileostomy and its posterior closure.
Materials and methodsBetween 2001 and 2012, 96 patients with temporary diverting ileostomy were retrospectively analyzed. Morbidity and mortality were analyzed before and after the stoma closure. The studied variables included age, sex, comorbidities, time for bowel continuity restoration and adjuvant chemotherapy.
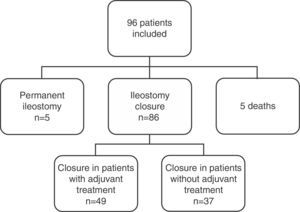
ResultsIn 5 patients the stoma was permanent and another 5 died. The morbidity and mortality rates associated with the stoma while it was present were 21% and 1% respectively. We performed a stoma closure in 86 patients, 57% of whom had previously received adjuvant therapy. There was no postoperative mortality after closure and the morbidity rate was 24%. The average time between initial surgery and restoration of intestinal continuity was 152.2 days. This interval was significantly higher in patients who had received adjuvant therapy. No statistically significant difference was found between the variables analyzed and complications.
ConclusionsDiverting ileostomy is associated with low mortality and high morbidity rates before and after closure. Adjuvant chemotherapy significantly delays bowel continuity restoration, although in this study did not influence the rate of complications.
La ileostomía derivativa temporal es utilizada frecuentemente para disminuir las consecuencias de una dehiscencia anastomótica distal tras la escisión total del mesorrecto en la cirugía del cáncer rectal. Esta técnica quirúrgica está asociada a una alta morbilidad y a una mortalidad no despreciable. El objetivo de este estudio es evaluar la morbilidad y la mortalidad asociadas a la ileostomía y su posterior cierre.
Material y métodosEntre 2001 y 2012 fueron analizados retrospectivamente 96 pacientes con ileostomía derivativa temporal. Se analizó la morbimortalidad tras la creación de la ileostomía y posteriormente al cierre de la misma, incluyendo como variables la edad, sexo, comorbilidades, tiempo transcurrido hasta la reconstrucción del tránsito y tratamiento adyuvante.
ResultadosEl estoma fue permanente en 5 pacientes y 5 fueron exitus. La morbimortalidad relacionada con el estoma mientras este estuvo presente fue del 21 y 1% respectivamente. Se realizó el cierre del estoma en 86 pacientes y el 57% había recibido previamente adyuvancia. No hubo mortalidad postoperatoria tras el cierre y la morbilidad fue del 24%. El tiempo medio entre la cirugía inicial y la reconstrucción intestinal fue de 152,2 días. Este intervalo fue significativamente superior en los pacientes que recibieron adyuvancia. No se encontró significación estadísticamente significativa entre las variables analizadas y las complicaciones.
ConclusionesLa ileostomía está asociada a una baja mortalidad y a una morbilidad alta antes y después de su cierre. La quimioterapia adyuvante retrasa significativamente la reconstrucción intestinal, aunque en este estudio no ha influido en el índice de complicaciones.
Anastomotic dehiscence is a serious complication in rectal cancer surgery. The consequences can be reduced by constructing a temporal derivative colostomy or ileostomy (TDI)1,2; the latter is preferable because it is linked to lower risk of complications.3–6
Constructing a TDI is considered a simple procedure, however, it is linked to 21%–70% of complications.7 Similarly, after closure, complications have a major impact on patients, with morbidity rates of up to 45.9%8; some case series report 6% mortality,9 and reoperation rates reaching 7%.10
Although reconstruction of intestinal transit is advised between 8 and 12 weeks11 after the original surgery and some authors recommend early closure,12,13 this time period may be influenced by several factors, including the need for adjuvant treatment.
This retrospective study aims to evaluate morbidity and mortality related to constructing and closing electively performed TDI in patients with colorectal anastomosis and total mesorectal excision (TME) for rectal cancer.
Materials and MethodsFrom April 2001 to December 2012, 134 patients who underwent loop ileostomy were included prospectively in the Colorectal Unit database at the Complejo Hospitalario Universitario de Vigo [Vigo University Hospital Complex]. We excluded cases where stoma was constructed in patients with a diagnosis other than rectal cancer or treated for anastomotic dehiscence. Finally, data from 96 consecutive patients were analyzed, who underwent TME with TDI for rectal cancer.
Ileostomy location was chosen by the surgeon. Although our unit has no current protocol for preoperative tests before ileostomy closure, in more than half of the cases gastrografin enema was performed to rule out complications of the anastomosis. Stoma closure was performed by circumferential incision; an end-to end manual anastomosis was performed, or a side-to-side anastomosis with manual or mechanical suturing as per the surgeon's indication. Incisions were closed primarily and patients received antibiotic prophylaxis. No intraabdominal drainage was placed. The surgeon decided the time for ileostomy closure time after adjuvant treatment in accordance with the oncologist.
Postoperative complications were divided into 2 groups, i.e., major complications and minor complications depending on whether they required resurgery or otherwise.
The following variables were included: sex, age, time elapsed since the first surgery, presence or absence of comorbidities (diabetes, hypertension, chronic obstructive pulmonary disease, heart disease), and adjuvant treatment time. Stoma-related morbidity and mortality were analyzed based on 2 stages: after construction (stage I), and after closure (stage II).
Windows-based SPSS® (SPSS version 21, SPSS, Chicago, IL, USA) software was used for result analysis. The Student's t test was used to compare quantitative variables. Normality of variables was verified by the Kolmogorov–Smirnov test. The chi square test was applied to compare qualitative variables. Values of P<.05 were considered statistically significant.
ResultsIleostomy was performed after TME in 96 patients with rectal cancer, 60 males (62%), mean age was 63.7±10 years. The stoma was created to protect low colorectal anastomosis in 80 patients (83%) and coloanal anastomosis in 16 (17%). Neoadjuvant treatment was prescribed in 56 cases (58%), and 49 patients (57%) received adjuvant treatment. The stoma remained permanent in 5 patients (5%) due to disease progression or problems with the colorectal anastomosis. Four patients died after surgery due to problems unrelated to the stoma, and another died of related TDI complications. Fig. 1 shows a patient progression diagram.
The stoma was closed in 86 patients (90%), in a mean time of 152.5±152 days from the initial surgery. This time period was ≥6 months in 38% of cases, due to complications arising during adjuvant treatment or problems with the waiting list. Average hospital stay following stoma closure was 8.9±6 days (Table 1).
Demographic and Clinical Characteristics of Patients.
| Patients | 96 |
| Men | 60 |
| Women | 36 |
| Mean age (years) | 63.7 (32–83) |
| No. of comorbidities ≥1 | 60 |
| Neoadjuvant treatment | 55 |
| Stoma closure | 86 |
| Mean time between 1st surgery and closure (days) | 152.5 (6–780) |
| Adjuvant treatment | 49 |
| No adjuvant treatment | 37 |
| Mean hospital stay after closing (days) | 8.9 (3–36) |
Stoma-related morbidity was 43%, and mortality 1%. Six patients (6%) required reoperation for ileostomy complications. Table 2 shows the analysis of complications by stages.
Stages: Complications.
| Complications | No. of patients (%) |
| Stage I | 91 |
| Dermatitis | 6 (7) |
| High output | 5 (5) |
| Parastomal hernia | 4 (4) |
| Bleeding | 2 (2) |
| Prolapse | 1 (1) |
| Fasciitis | 1 (1) |
| Resurgery | 2 (2)a |
| Mortality | 1 (1) |
| Stage II | 86 |
| Wound infection | 9 (10) |
| Prolonged ileus | 6 (7) |
| Intra-abdominal abscess | 2 (2) |
| Ileal anastomosis fistula | 1 (1) |
| Entero-cutaneous fistula | 1 (1) |
| Laparocele | 1 (1) |
| Resurgery | 4 (5)b |
Stage I: Since ileostomy construction. Stage II: After ileostomy closure.
In stage I, 19 patients (21%) had stoma-related complications: dermatitis (7%), high output (5%), parastomal hernia (4%), bleeding (2%), prolapse (1%), and fasciitis (1%) resulting in death. A total of 2 patients (2%) underwent reoperation.
Twenty-one patients (24%) had complications after ileostomy closure (stage II): wound infection (10%), prolonged ileus (7%), intraabdominal abscess (2%), anastomotic leak (1%), enterocutaneous fistula (1%), and laparocele (1%). Four patients (5%) underwent reoperations, 2 of them early (<30 days).
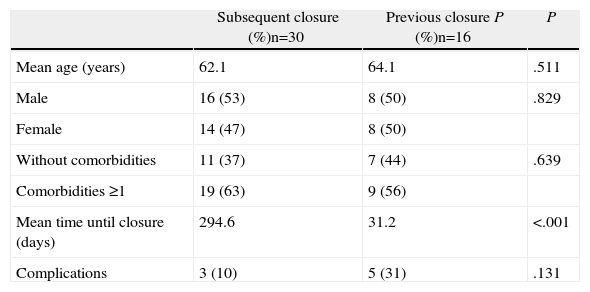
Stoma closure was performed in 30 of 49 patients who received adjuvant treatment after treatment completion, and before completion in 16. In 3 cases, due to problems with the stoma, closure was performed earlier, performed during adjuvant treatment. Average time between initial surgery and stoma closure was longer in patients who received adjuvant treatment compared to those who did not (194.2 days vs 97.4 days, P<.005). Among patients who received adjuvant chemotherapy, this time period was also shorter in those undergoing reconstruction after chemotherapy compared to those who had it prior (294.6 days vs 31.2 days, P<.001). This variable, the same as age, sex, and number of comorbidities, was not statistically significant for post-operative complications (Tables 3 and 4).
Non-adjuvant vs Adjuvant Treatment. Complications After Ileostomy Closure.
| Non-adjuvant treatment (%)n=37 | Adjuvant treatment (%)n=49 | P | |
| Mean age (years) | 64.8 | 62.5 | .330 |
| Male | 27 (73) | 27 (55) | .090 |
| Female | 10 (27) | 22 (45) | |
| Without comorbidities | 12 (32) | 21 (43) | .325 |
| Comorbidities ≥1 | 25 (68) | 28 (57) | |
| Mean time until closure (days) | 97.4 | 194.2 | <.005 |
| Complications | 10 (27) | 8 (16) | .227 |
| Major complications | 2 (5) | 0 | .100 |
| Minor complications | 8 (21) | 8 (16) | .532 |
Complications: Subsequent Closure vs Prior to Adjuvant Treatment.
| Subsequent closure (%)n=30 | Previous closure P (%)n=16 | P | |
| Mean age (years) | 62.1 | 64.1 | .511 |
| Male | 16 (53) | 8 (50) | .829 |
| Female | 14 (47) | 8 (50) | |
| Without comorbidities | 11 (37) | 7 (44) | .639 |
| Comorbidities ≥1 | 19 (63) | 9 (56) | |
| Mean time until closure (days) | 294.6 | 31.2 | <.001 |
| Complications | 3 (10) | 5 (31) | .131 |
Overall morbidity in this case series (43%) was similar to that reported by other authors.14 The percentage of complications attributable to TDI before closure ranges between 5% and 28%.15–19 In our study it was 21%, and similar to other case series, the most frequent were dermatitis, high intestinal output and parastomal hernia. Updated literature has no references on postoperative mortality attributable to stomas prior to closure. One patient in this series died 20 days after several reoperations due to abdominal wall fasciitis from ischemia and intestinal perforation in the ileum–fascial junction.
In an update of 46 studies, Chow et al.,20 analyzing results from 6107 patients, reported morbidity following TDI closure in 17.3% and a mortality rate of 0.4%. The most frequent complications were intestinal obstruction and abdominal wall infection. Our complication rate after TDI closure was 24% and 4 patients (5%) had to be reoperated on. The most common complications were wound infection and prolonged ileus. Reoperation rate was lower than that reported by other authors.14,20 There was no postoperative mortality.
We found that complication rates were significantly higher, and morbidity attributable to ileostomy prior to and after its closure is similar to those from other studies.
Optimal time between TDI construction and its closure is controversial. A period between 8 and 12 weeks from first surgery would be sufficient to allow full patient recovery time, reduce intra-abdominal adhesion density and allow for inflammation and edema resolution between abdomen and stoma.20 A time period less than 8.5 weeks would increase the risk of complications,21 and a longer period would be a negative outcome predictor.22 However, other authors13,23 conclude that in selected patients, stoma closure can be performed on the first hospital admission without increased morbidity. In 43% of our patients stoma closure was performed at a 97.4-day-period, since they did not receive adjuvant treatment, and the percentage of minor or major complications was not statistically significant compared to the group with greater wait time.
However, for patients with stages II–IV rectal cancer, this time period is determined by the need to complete chemotherapy cycles or start radio-chemotherapy, when these were not administered previously to surgery, so that temporary stoma closure may interfere with their start. This determines delaying loop ileostomy closure until after completion of adjuvant treatment.9,10
Some authors,24,25 in their univariate result analysis, reported a rate of complications after TDI closure significantly higher in patients receiving chemotherapy or radiotherapy. In a recent study25 on 5401 patients, while chemotherapy and radiotherapy were significantly related to an increased rate of complications, this significance was lost when other factors were included in the multivariate analysis. This relationship has not been verified in our case series and those of other authors.8,10 Performing histopathological analysis in patients with low rectal cancer undergoing adjuvant treatment yielded no significant differences relative to the control group on postoperative complications after ileostomy closure or differences in crypt distortion, mucin depletion, acute or chronic inflammation and eosinophil infiltration in ileum.26 Therefore, it is conceivable that, in addition to adjuvant treatment, other factors such as advanced cancer and poorer health may have an impact on increased complications after TDI closure.
In our opinion, the time period to wait for stoma closure in the event the patient receives adjuvant treatment is too long and it should be performed as soon as possible. However, due to the small sample size, we cannot assume any recommendation on ideal stoma closure time in patients with rectal cancer requiring adjuvant treatment.
Complications prior to intestinal reconstruction must strongly emphasize that although this is a simple surgical procedure, we must be very meticulous in performing the technique, since in our experience it is one of the most important factors in developing morbidity in relation to the stoma.
In view of the above findings, we concluded that a TDI cannot always avoid the serious consequences of a colorectal anastomotic fistula, but the overall morbidity potential to patients with rectal cancer is very high. Therefore, the possible benefits of TDI must be considered in correlation with the potential adverse effects demonstrated in this study.
Conflict of InterestAuthors declare having no conflict of interest.
Please cite this article as: Pérez Domínguez L, García Martínez MT, Cáceres Alvarado N, Toscano Novella Á, Higuero Grosso AP, Casal Núñez JE. Morbilidad y mortalidad de la ileostomía derivativa temporal en la cirugía por cáncer de recto. Cir Esp. 2014;92:604–608.