The high incidence of parastomal hernia and the controversy surrounding its repair make its prevention an area of intense research. The aim of this article is to describe the modified Sugarbaker technique with a new mesh for the prevention of parastomal hernia using a laparoscopic approach.
La elevada incidencia de la hernia paraestomal y la controversia en su reparación hacen que su prevención sea un área de intensa investigación. El objetivo del presente artículo es describir la técnica de Sugarbaker modificada con una nueva malla para la prevención de una hernia paraestomal, utilizando un abordaje laparoscópico.
The high incidence of parastomal hernias (PSH)1,2 and the controversy regarding the best method for their repair3 make the prevention of PSH one of the areas with the most intensive clinical research in abdominal wall surgery. In open surgery, prospective randomized trials have shown a significant decrease in the rate of PSH in patients with mesh placed in the preperitoneal position (sublay).4–6 In addition, recent meta-analyses and systematic reviews have confirmed these findings.7–9 In laparoscopic surgery, there have also been reports of techniques for placing prophylactic mesh in order to prevent PSH when creating a stoma.10,11 A prospective, randomized study has reported a significant reduction in PSH with the use of prophylactic mesh and a keyhole technique in an intraperitoneal position (IPOM).12
Given these data, it would seem very attractive to recommend the prophylactic placement of prostheses during the creation of an ostomy in cases of open as well as laparoscopic surgery. Nonetheless, the results of the techniques and the mesh used in the previously-mentioned studies are far from being ideal. Thus, further data is necessary in order to define which patient groups could benefit the most from the placement of prophylactic mesh and to clarify technical aspects, such as the best type of mesh and surgical technique.
Our objective is to describe a surgical technique for the placement of a new mesh with ideal characteristics for the prevention of parastomal hernias when using a laparoscopic approach.
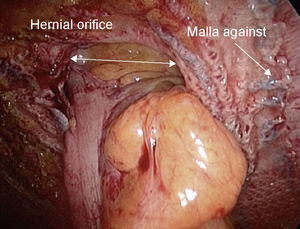
Surgical TechniqueAfter mechanical preparation of the colon and antibiotic prophylaxis in the induction of anesthesia, laparoscopic abdomino-perineal resection was performed in a patient with adenocarcinoma of the rectum. The trocars were placed in the supra-umbilical area (Hasson), right flank (5mm), right iliac fossa (11mm) and suprapubic region (optional) (5mm). The site for the ostomy was previously marked by the stomatherapy nurse, and a 5-mm port was inserted through this mark. After the resection, closure of the perineal wound and after evacuating the pneumoperitoneum, the terminal colostomy was brought out at the previously-marked site (without modifying the position of the patient). After having restored the pneumoperitoneum and before suturing the colon, the prosthesis was placed laparoscopically, introduced through the 11mm trocar. We used a 15×20cm oval, composite, flexible, low-profile mesh (Physiomesh®, Ethicon, Johnson & Johnson Co.) made of a non-absorbable macroporous polypropylene material laminated between 2 layers of poliglecaprone-25, with an unstained polydioxanone film joining the poliglecaprone-25 and the polypropylene layer, with a colored polydioxanone mark for orientation (Fig. 1). It is a mesh made specifically for laparoscopic incisional hernia repair that, as it is partially absorbable, leaves less material implanted in the patient. In addition, it is an adhesive, transparent mesh that allows for vision of the colon and mesocolon and its entrance in the orifice of the ostomy, which provides easy-to-use and correct placement, regardless of whichever side is used. The technique used for the placement of the mesh was a modified Sugarbaker technique.13 The placement of the mesh was performed with a double crown of reabsorbable straps (Securestrap®, Ethicon, Johnson & Johnson Co.). Mesh placement time was 15min (Fig. 2).
DiscussionIn our opinion, the technique described is easy to do and can be useful in the prevention of PSH. The reason for describing this technique is based on the experience of our previous studies.5,12 In these studies, a low-density mesh was used with an orifice in the center of the same keyhole that allows bringing out the colostomy. It has been mentioned that the keyhole technique used in open surgery may possibly prevent the development of PSH because the orifice created in the mesh for the passage of the intestine will remain constant and will not later become enlarged.14
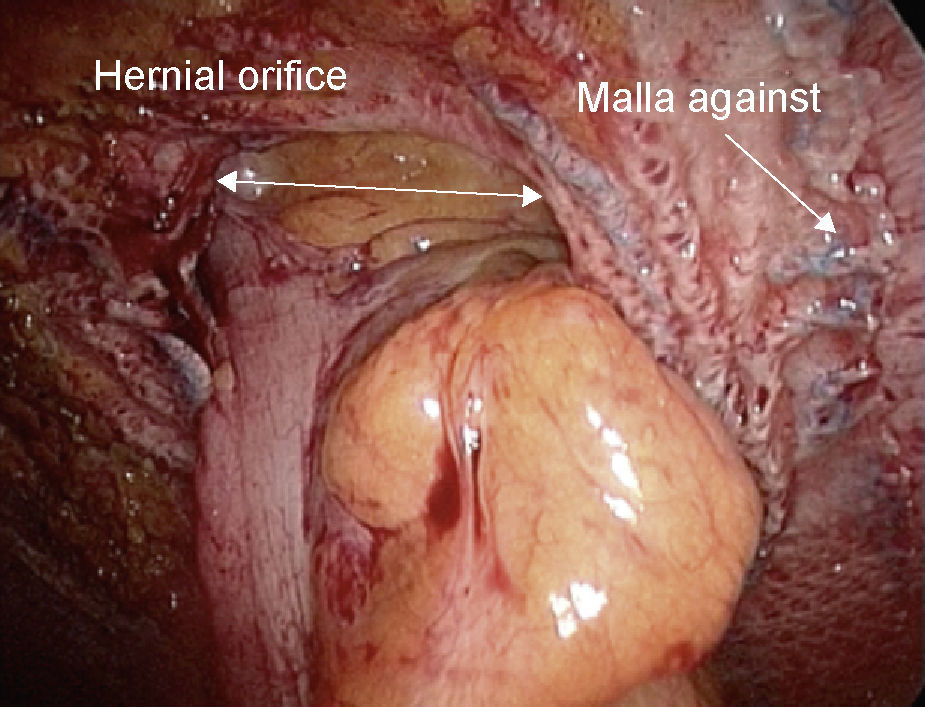
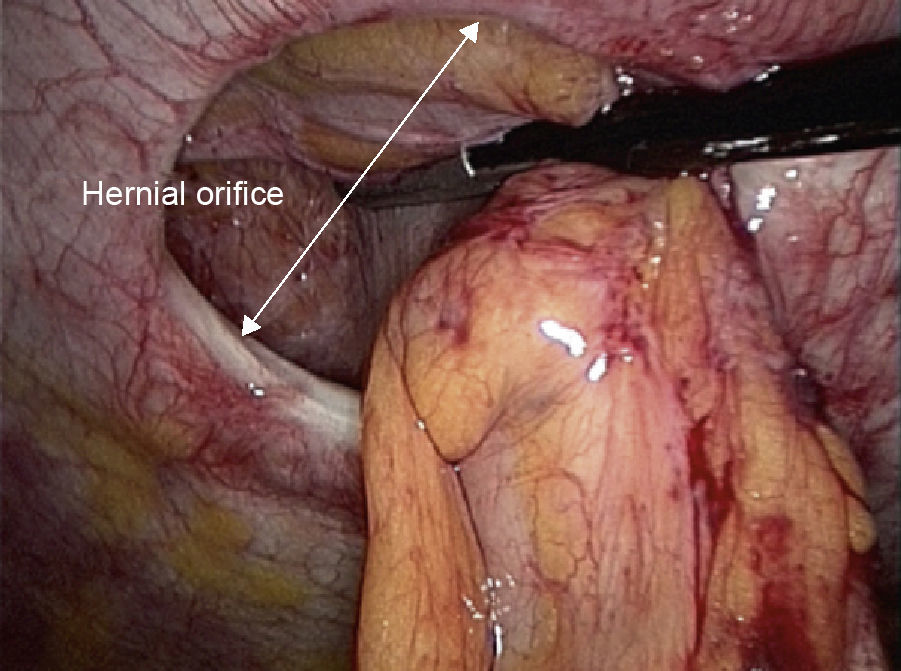
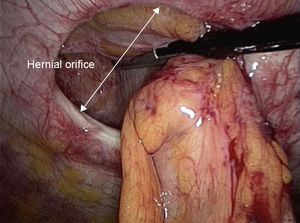
When we used the laparoscopic approach, the mesh was significantly effective in the prevention of PSH. However, it was observed that the incidence of PSH in the group with mesh was surprisingly high,12 although few patients were symptomatic. In addition, in the patients of the group with mesh who needed reoperation, we observed that the mesh was contracted and had an enlarged central orifice (Fig. 3), practically identical to the wide central orifice of patients who had been reoperated due to PSH in the group without mesh (Fig. 4). We believe that the contraction of the mesh does not just “shrink”, but it also facilitates the enlargement of the central orifice, favoring the development of PSH. The modified Sugarbaker technique that is reported does not require creating an orifice in the mesh and may avoid the described disadvantages related to the contraction of the material. On the other hand, since the mesh used is light, partially absorbable, transparent, and adhesive, has a mark for centering and is able to contact with the abdominal viscera on both sides, the technique is easily performed. Currently, a prospective, controlled, randomized study is being carried out on the efficacy of this technique and with this mesh in the prevention of PSH when using a laparoscopic approach.15 Although the follow-up period is still short, for the moment no perioperative morbidity has been detected related to either the technique or the mesh.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: López-Cano M, Serra-Aracil X. Prevención laparoscópica de la hernia paraestomal mediante técnica de Sugarbaker modificada con malla compuesta (Physiomesh®). Cir Esp. 2013;91:331–334.