The surgery of gallbladder polyps is not well defined due to the lack of evidence-based clinical guidelines.
ObjectiveTo analyze the management of polyps in Spain, and a review of the literature and treatment standards.
Material and methodsThe reports on cholecystectomy with gallbladder polyps (GBP) were extracted from the Pathology data base. Patients subjected to surgery with a diagnosis of GBP were identified in the Surgery data base. A single list was prepared and a review was made of the clinical histories, including, age, gender, clinical data, ultrasound report, and histopathology report.
ResultsA total of 30 patients, with a median age of 51 years (range 22–83), 21 of whom were female, were included. The ultrasound diagnosis was GBP in 19 patients, GBP and calculi in 7 cases, and calculi with no polyps in 4 cases. Other diagnoses concurrent with GBP were multiple haemangiomas (3), large single simple cyst (1), and multiple simple cysts (1). Eleven patients had typical pain (biliary origin), 5 of which showed no calculi on ultrasound. Eight had non-specific pain, which persisted in 3 cases after the cholecystectomy. Pseudopolyps were found in 20 gallbladders, and true polyps in 4 cases. In 3 cases, polyps were not found in the pathology study.
ConclusionsThe ultrasound report must specify the size, shape, and number of polyps. Patients with biliary type pain would benefit from a cholecystectomy. The probability of malignancy is minimum if the GBP is less than 10mm and aged under 50 years, and a cholecystectomy is not required. A GBP greater than 10mm should be an indication of cholecystectomy.
La cirugía por pólipo de vesícula biliar está poco definida debido a la carencia de guías clínicas basadas en la evidencia.
ObjetivoAnalizar el manejo de los pólipos en nuestro medio, y revisión de la literatura y estándares de tratamiento.
Material y métodosDe la base de datos de Patología se extrajeron los informes de colecistectomía con pólipos vesiculares (PV). De la base de datos de Cirugía se identificó a pacientes intervenidos con diagnóstico de PV. Se confeccionó un listado único y se llevó a cabo la revisión de las historias clínicas incluyendo edad, sexo, clínica, informe ecográfico e informe anatomopatológico.
ResultadosSe incluyó a 30 pacientes, mediana de edad 51 años (rango 22-83), 21 mujeres. En 19 pacientes el diagnóstico ecográfico fue PV, 7 de PV y litiasis, y 4 de litiasis sin pólipo. Otros diagnósticos concurrentes con PV fueron hemangiomas múltiples (3), gran quiste simple único (1), quistes simples múltiples (1). Once pacientes tuvieron dolor típico (origen biliar), 5 de los cuales sin litiasis ecográfica. Ocho presentaron dolor inespecífico, persistiendo en 3 tras la colecistectomía. Se encontraron pseudopólipos en 20 vesículas, y pólipos verdaderos en 4 casos. En 3 casos no se hallaron pólipos en el examen patológico.
ConclusionesEl informe ecográfico debe especificar el tamaño, forma y número de pólipos. Los pacientes con dolor biliar típico se beneficiarán de una colecistectomía. Ante un PV menor de 10mm y edad menor de 50 años la probabilidad de malignidad es mínima y no requiere colecistectomía. Los PV mayores de 10mm deben ser indicación de colecistectomía.
In 1970, Christensen and Ishak classified gallbladder polyps as benign tumors (adenoma), pseudotumors (adenomatous hyperplasia, adenomyoma, inflammatory polyp and cholesterol polyps), and malignant tumors (adenocarcinoma).1
The polyp-carcinoma sequence in the gallbladder, similar to what happens in colorectal carcinomas, was proposed years ago2,3 as a carcinogenic theory for gallbladder cancer, and it is one of the main reasons for ultrasound follow-up in patients diagnosed with gallbladder polyps (GBP). The other hypothesis for the genesis of gallbladder cancer that seems to prevail is the metaplasia–dysplasia–cancer sequence.4 A molecular study on the DNA of gallbladder adenomas and carcinomas demonstrated that the changes detected in dysplasia, carcinoma in situ and invasive cancer were absent in adenomas, and the authors concluded that the latter were not precursors for gallbladder adenocarcinoma.5 Other molecular studies suggest that, even though the 2 hypotheses may be true, the adenoma–carcinoma sequence is involved in the majority of gallbladder cancers.6–9
The published prevalence of GBP in the healthy population is 4.3% in Denmark,10 5.9% in Japan,11 6.1% in Germany (Ulm),12 6.9% in China (Taiwan),13 and 6.1% in Korea (Seoul).14 Most GBP are cholesterol polyps and require no treatment unless they are symptomatic.
Arguments in favor of an aggressive approach to GBP are that laparoscopic cholecystectomy—with low morbidity and anecdotal mortality—could resolve the problem, while the appearance of gallbladder cancer is associated with a poor prognosis.
Arguments against an aggressive approach to GBP are the anecdotal incidence of cancer in polyps smaller than 10mm, the absence of malignization in cholesterolosis, and the serious prognosis of some lesions of the bile duct associated with cholecystectomy.
There are no clinical guidelines or evidence-based studies for the management of GBP. This paper provides the experience of our Hospital and retrospectively analyzes the diagnostic-therapeutic approach in order to review GBP management.
Material and MethodsFrom the Pathology Department database, we gathered the histologic reports of gallbladder specimens with polyps from the period between January 2002 and June 2011. We included all those patients who had been treated surgically for GBP even though the definitive histologic results demonstrated absence of lesions. We carried out a retrospective study of the medical files of patients who underwent cholecystectomy, analyzing age, sex, preoperative diagnosis, surgical indication and histologic diagnosis of the polyps.
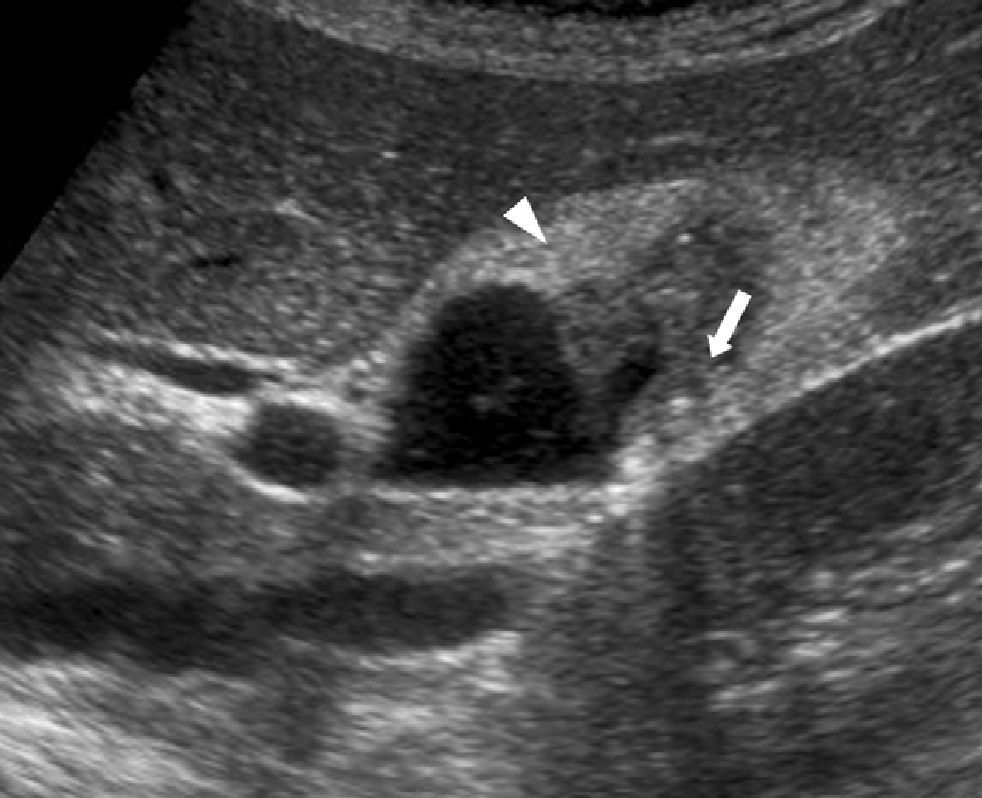
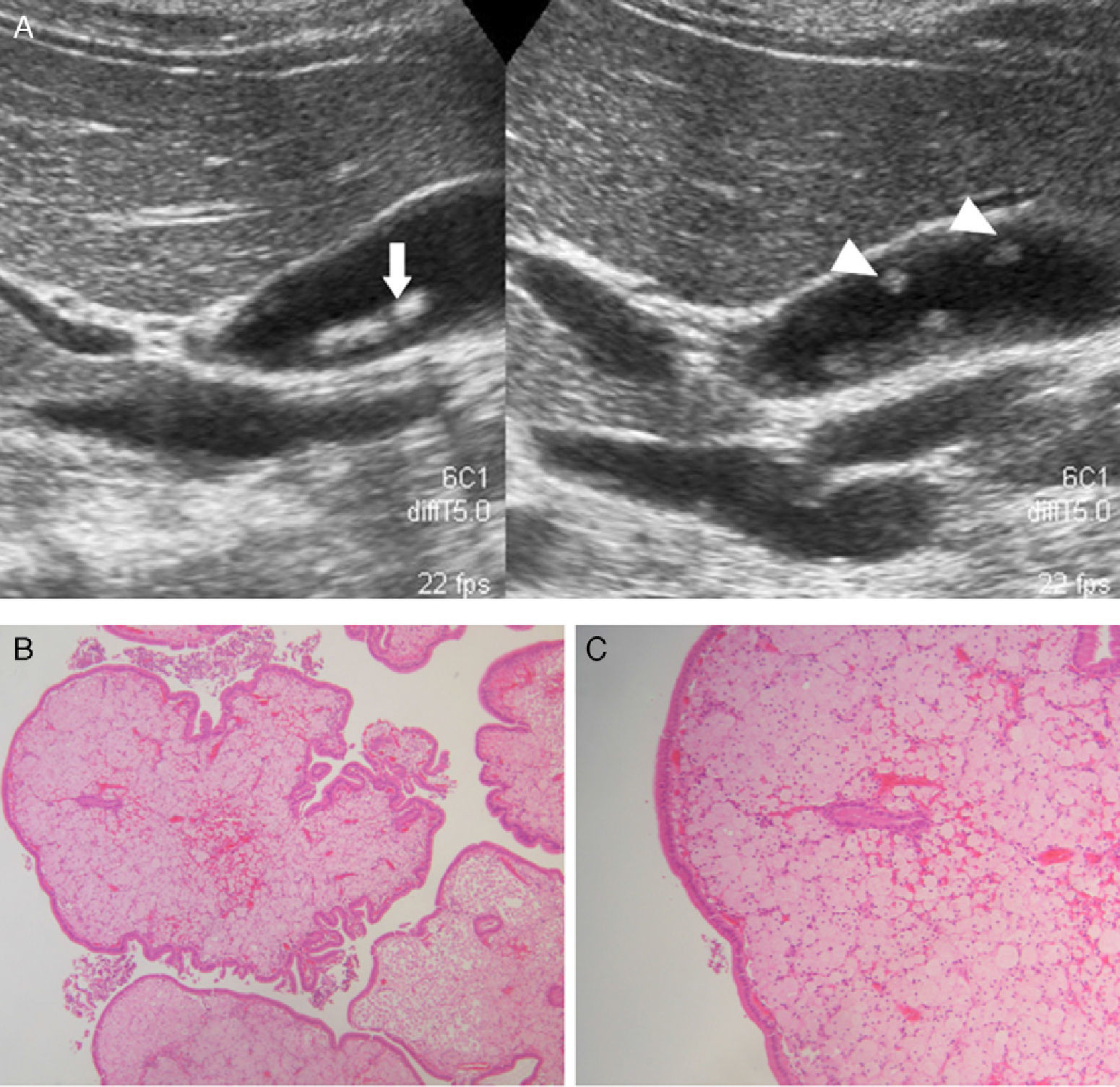
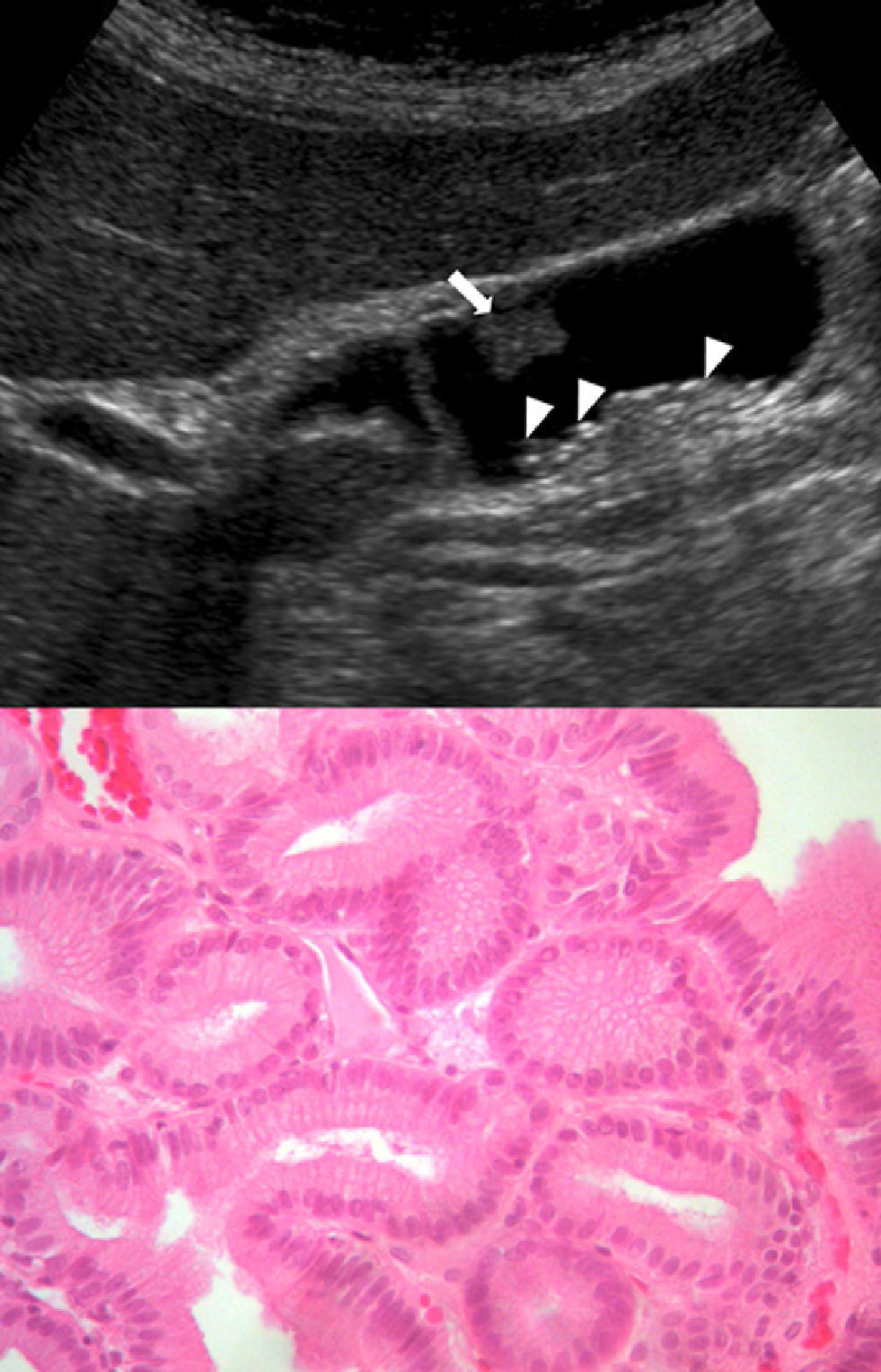
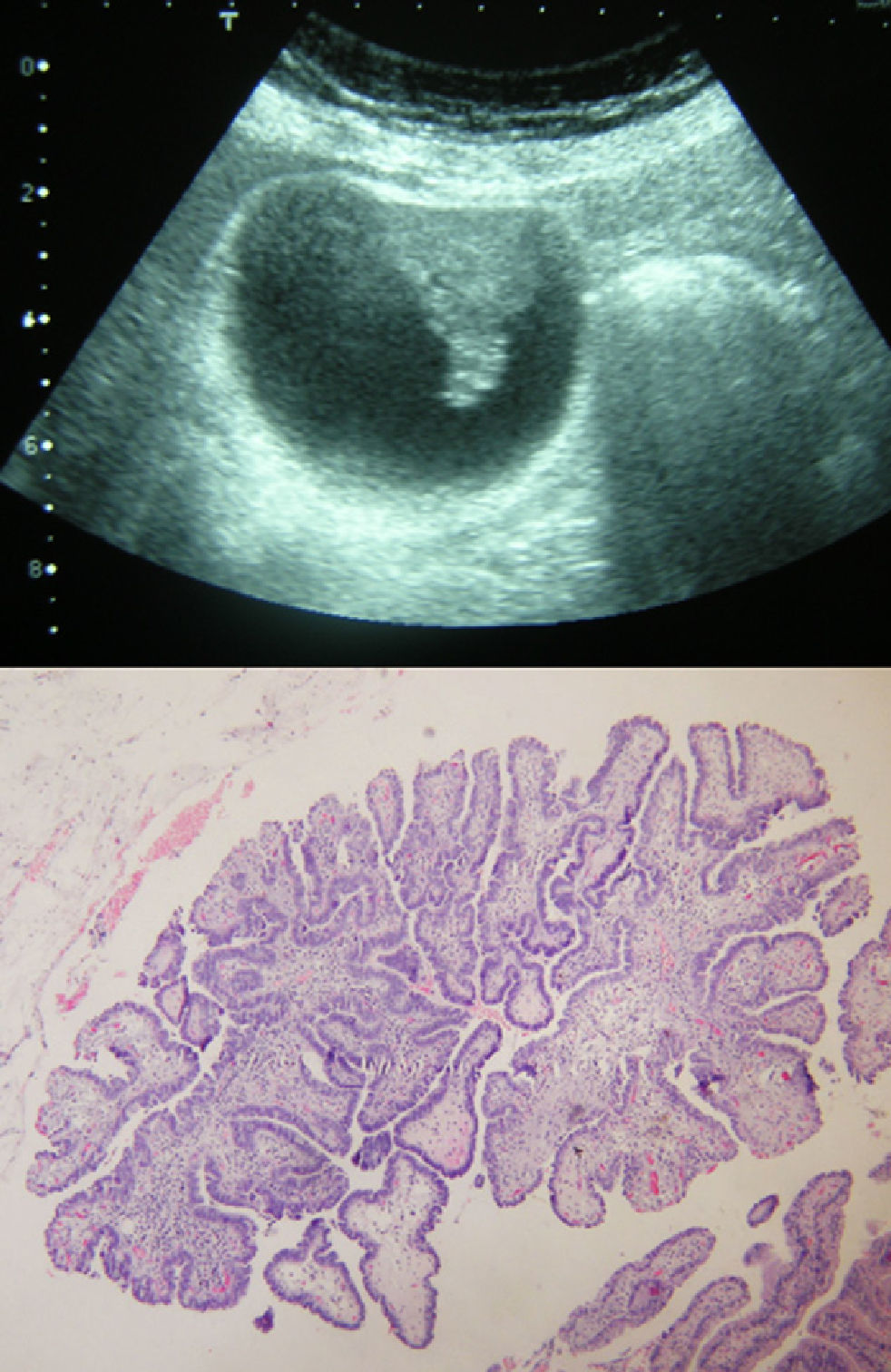
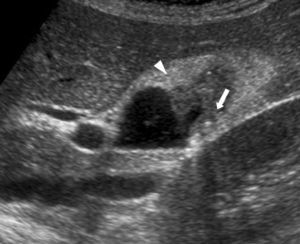
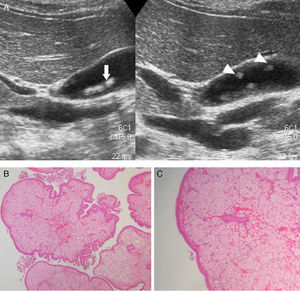
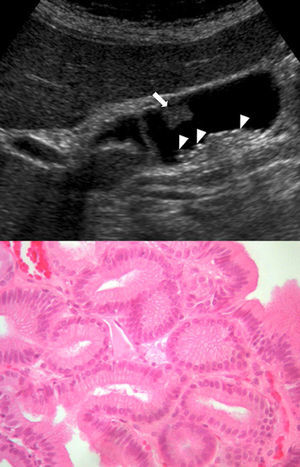
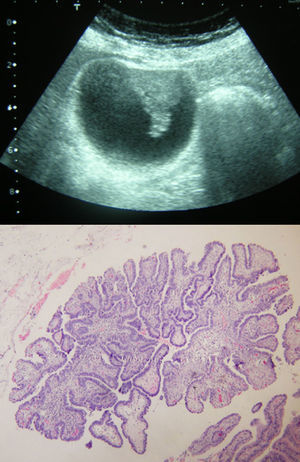
Abdominal ultrasounds (Philips SD800 with 5MHz abdominal transducer, and Toshiba Aplio XV with 3.5MHz abdominal transducer) were performed by radiologists with experience in the field of abdominal ultrasound, with the patient in supine decubitus and in right lateral decubitus, after 6h of fasting. According to the ultrasound images, the gallbladder polyps were classified as pseudotumor or tumor lesions. The group of pseudotumor lesions included focal adenomyomatosis or adenomyoma (focal wall thickening, cystic spaces in the interior with echogenic content within the cyst, and “comet-tail” artifact; Fig. 1); cholesterol polyps (focal form of cholesterolosis characterized by oval-shaped, multiple, hyperechogenic lesions in contact with the wall, without posterior shading, that are immobile with changes in posture; Fig. 2); and inflammatory polyps reactive to an acute or chronic inflammatory process, although there are no descriptions in the radiological literature that characterize them and the diagnosis is made by pathology study after cholecystectomy. Within the group of the tumor lesions, we find adenomas (echogenicity similar to the liver, pedunculated or sessile, may present Doppler flow in the interior; Fig. 3), suspicious large-sized lesions, thickening adjacent to the gallbladder wall, internal circulation or associated signs of malignancy such as lymphadenopathies or metastases.
During the study period, GBP was diagnosed in 30 patients. Twenty-seven patients were included from the Pathology Department database, and another 3 patients had a preoperative diagnosis of GBP. Mean age was 52.24±15.6 (range 22–83, median 51), and 21 were women. Seventeen of the 30 patients were 50 years of age or older.
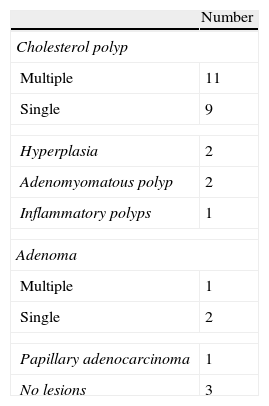
Out of the 30 patients, 19 had a previous ultrasound diagnosis of GBP, 7 GBP and calculi, and 4 calculi without polyps. Diagnoses associated with GBP included: 3 patients with associated multiple hemangiomas, one patient with suspicion of a hydatid cyst that was actually a simple cyst, and one patient with multiple simple cysts. The majority of the polyps were cholesterol polyps (Table 1). In 4 cases, the polyps were true neoplastic lesions. Two gallbladders contained tubular adenomas while another gallbladder contained multiple adenomatous lesions. There were no cases of dysplasia. In one patient, there was an incidental detection (during an ultrasound study for acute pancreatitis) of a polyp that was suspicious for malignancy due to size (32mm) and shape (sessile) that turned out to be a papillary adenocarcinoma (Fig. 4). In this patient, the study was completed with abdominal CT, which provided no additional information, and open cholecystectomy was performed with resection of the hepatic gallbladder bed at a thickness of 2cm and lymphadenectomy of the hepatic pedicle. The result was T1N0M0. In 2 patients, there was a coincidence of different types of polyps in the same cholecystectomy specimen. One presented adenomatous hyperplasia together with cholesterol polyps and inflammatory polyps. The other patient associated 2 hyperplastic polyps, one cholesterol polyp and gallbladder cholesterolosis.
Anatomic Pathology Diagnoses of the Polyps Found on Cholecystectomy.a
| Number | |
| Cholesterol polyp | |
| Multiple | 11 |
| Single | 9 |
| Hyperplasia | 2 |
| Adenomyomatous polyp | 2 |
| Inflammatory polyps | 1 |
| Adenoma | |
| Multiple | 1 |
| Single | 2 |
| Papillary adenocarcinoma | 1 |
| No lesions | 3 |
In 3 cases with previous ultrasound diagnosis for GBP, the lesions were not found during the pathology examination.
With regard to symptoms, 11 patients presented typical pain (pain in the right hypochondrium radiating toward the scapula). Of these, 5 presented ultrasound images of GBP without associated calculi. One of the patients included in these 11 cases was diagnosed with GBP as an incidental finding on a gynecological ultrasound, and during follow-up developed typical symptoms. Eight patients debuted with nonspecific pain (including in this group dyspepsia and epigastralgia). After cholecystectomy, the nonspecific pain persisted in 3 out of 8 cases, and the other 5 were asymptomatic.
DiscussionAmong the indications for cholecystectomy, we found symptomatic calculi, symptomatic polyps or polyps larger than 10mm, ultrasound suspicion for symptomatic cholesterolosis, and ultrasound suspicion for adenomyomatosis, both symptomatic and asymptomatic. The number of polyps alone is not an indication for surgery but, if it were, solitary polyps would be a reason for alarm, as there is a lower probability for lesions with uncertain prognosis when the polyps are multiple. The symptoms do not differ from those that appear in symptomatic cholelithiasis. There is an anecdotal case described in which a detached cholesterol polyp originated an otherwise acalculous cholecystitis.15
For most groups, there is no indication for surgery if the polyp is smaller than 10mm. Nonetheless, there are isolated groups who support a more aggressive attitude after having found cases of cancer with smaller polyps. Kubota et al.16 discovered 13% of gallbladder carcinomas in polyps smaller than 10mm. Shinkai et al.17 have proposed cholecystectomy when the number of lesions is fewer than 3, regardless of size. In the series of polyps smaller than 20mm that they analyzed, the mean size of the malignant polyps was 10.8mm±4.16. This incidence of malignant polyps in lesions smaller than 1cm has not been seen in most published series. De Matos et al.18 found 2 malignant polyps out of the 93 analyzed in their series, and the mean size in both lesions was 21.5mm. Kwon et al.19 found 35 malignant polyps out of 291 analyzed, and their mean size was 27.97mm±2.46, although among them there was one of 8mm and another of 9mm. Out of 80 patients who underwent cholecystectomy due to polyps, Ito et al.20 found one 14mm lesion with high-grade dysplasia (carcinoma in situ) and no invasive adenocarcinoma.
The increasing size of the polyps during follow-up, their association with calculi, or the suspicious characteristics of the lesions may determine the indication for cholecystectomy in some cases. The definition of increase in size has not been clearly established in the literature. If a polyp grows 4–6mm in an interval of 18 months, should we perform cholecystectomy? For some groups, the growth of a polyp is only significant if it surpasses 3mm or more,14,20,21 which is a measurement that was established arbitrarily as there are no evidence-based data to either support or revise this threshold.
Some authors have warned about the increased risk for cancer when the polyps are associated with calculi.22 Choi et al.,23 however, did not detect the appearance of gallbladder cancer in 361 patients who had been followed for 6.5 years in a study comparing the change in polyp size among patients with asymptomatic calculi and polyps (176 patients) and those with just polyps (185 patients), without finding differences in the behavior of the GBP. Kwon et al.19 studied 291 patients who underwent cholecystectomy with histologic confirmation of GBP: 256 were benign and 35 malignant. The association with calculi was not a statistically significant difference between the two groups (21.5% in benign [55/256]; 17.1% in malignant [6/35], P=.554). Park et al.14 found 25 (14%) adenocarcinomas in 280 patients, only 2 of which had associated calculi. Therefore, it seems highly probable that calculi associated with GBP is not a risk factor, at least no greater than when they are not associated with polyps.
In contrast with cholesterolosis, adenomyomatosis has been associated with carcinoma.24,25 Adenomyomatosis is a mucosal hyperplasia with growth toward the muscular layer, which is thickened. Cholesterolosis is a mucosal hyperplasia with accumulation of cholesteryl esters and triglycerides in the epithelial macrophages. The differential diagnosis between these entities can be performed with abdominal ultrasound.
A study by the Radiology Department at Beth Israel Deaconess Medical Center26 concluded that it is not necessary to follow-up polyps measuring less than 6mm. They reviewed 346 patients with an ultrasound diagnosis of GBP and a mean follow-up of 8 years (range, 5–10.4 years). But the ultrasound follow-up was only done in 149 (43%), clinical follow-up in 155 (45%), and cholecystectomy was performed in 42 patients (12%). No cases of cancer were found in the 346 patients, but this result must be considered with the possible bias of the absence of ultrasound data for 197 patients, and the logical absence of histology in the 304 patients without cholecystectomy. Thus, although GBP seem to be mostly benign in behavior and may not even require further ultrasound studies, this approach has not been shown to be reliable based only on a size smaller than 6mm, either in this study or any other studies. Therefore, as we still have no cost analysis studies or large-scale assays, it is still daring, as argued by Mitchell E. Tublin in 2001,27 not to normally recommend ultrasound follow-up.
The analysis of our series of cholecystectomies due to polyps suggests an aggressive tendency toward this diagnosis, since only 16 patients out of 30 presented an age over 49. The pathology results confirm the suspicion since the majority were cholesterol polyps diagnosed as incidental findings or with nonspecific abdominal symptoms. As there are no evidence-based clinical guidelines, the decision to operate for diagnosis of GBP will be conditioned by the information that the surgeon offers the patient. With the current published data, the probability that a polyp smaller than 10mm is malignant is small, the probability that a true polyp smaller than 10mm will degenerate over time into an adenocarcinoma is small, and the probability that multiple lesions smaller than 10mm are pseudopolyps is high.
In the series by the Memorial Sloan Kettering Cancer Center group, which is renowned for its prestigious work in hepatobiliary surgery, only 80 patients out of 470 underwent cholecystectomy. Out of these 80, 17 (21%) had surgery for lesions greater than 10mm, 18 (22.5%) because of symptoms, 11 (14%) due to patient choice despite having polyps smaller than 10mm, and 34 (42.5%) during surgery due to another unrelated abdominal disease. These data demonstrate a restrictive approach with regards to the surgical indication for GBP.
In our series, the cholecystectomy specimens reported no findings in 3 patients. In the literature, this is not uncommon. Ito et al.20 found no polyps in 26 (32.5%) out of 80 patients who underwent cholecystectomy with diagnosis for GBP. In their discussion, they provide no explanation for this datum and consider these cases false positives of the ultrasound studies. Csendes et al.21 found no lesions in 3 (11%) out of 27 cholecystectomy pieces, but did not discuss this fact. With the few cases seen in our analysis, we cannot reach any conclusions in this regard, but it was suspected that opening the gallbladder after having removed it in the operating room could have influenced in the loss of polyps in 2 cases, especially cholesterol polyps, when the specimens were put into formaldehyde. And it was also suspected in the third case that the cholesterol polyps could have easily become detached and lost with the bile when the gallbladder was being opened in the pathology laboratory.
Some authors have studied possible risk factors that would help predict the malignancy of polyps. In a univariate study, Park et al.14 found risk factors to be age (≥57yrs), presence of symptoms, size (≥10mm), and morphology (sessile). In their multivariate analysis, only age and size were maintained as independent predictors for malignancy. In the univariate analysis of the study by Kwon et al.,19 risk factors for malignancy included age, presence of symptoms, sessile morphology, size, and single polyps. The multivariate analysis maintained age, morphology, and size as prognostic criteria for malignancy. The cut-off levels for age and size obtained with ROC curves were 57.5yrs and 12.5mm, but these were rounded up and down to 60yrs and 10mm, respectively, and the sessile criterion was added. With these variations, 77.8% (14/18) of the malignant polyps met the 3 criteria, 28.6% (12/42) met 2 criteria and 7.8% (9/116) met one criterion. In the 115 patients without any of the 3 criteria, there were no cases of malignant polyps.
As for the surgical approach of GBP, the laparoscopic method is most widely used. Nevertheless, when there is a preoperative suspicion for malignancy (for example, sessile polyp and size larger than one centimeter, or other radiographic signs), the general recommendations are to use an open approach. For this reason, we decided on open cholecystectomy in one patient of the series who presented with a large, sessile polyp. This topic is also controversial, however, and more studies would be required to support the advantages of the open technique in this type of polyps.
In conclusion, the ultrasound diagnosis of a gallbladder polyp should be accompanied by a detailed report of its size, shape and number. When the polyps are symptomatic, cholecystectomy should be offered as treatment. Polyps smaller than 10mm detected in patients under the age of 50 have a minimal probability of malignancy, and ultrasound follow-up is safe. The presence of multiple lesions in a young patient suggests benignity. In patients with polyps larger than 10mm, cholecystectomy is recommended. In patients with smaller polyps but with suspicious characteristics seen on ultrasound who are over the age of 50, surgery should be recommended even though the probability of malignancy is low. Care should be taken when opening the surgical specimen for inspection, and this should be done on a surface for proper collection.
Although some published studies do not recommend the ultrasound follow-up of unremoved polyps, we recommend a 6-month ultrasound and then annual ultrasounds for 2 or 3 years until studies are published with greater evidence for ruling out this recommendation.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Morera-Ocón FJ, Ballestín-Vicente J, Calatayud-Blas AM, de Tursi-Rispoli LC, Bernal-Sprekelsen JC. Indicaciones quirúrgicas en los pólipos de vesícula biliar. Cir Esp. 2013;91:324–330.